Sleep Disorder
Sleep disorders are conditions that result in changes in the way that you sleep.
A sleep disorder can affect your overall health, safety and quality of life. Sleep deprivation can affect your ability to drive safely and increase your risk of other health problems.
Some of the signs and symptoms of sleep disorders include excessive daytime sleepiness, irregular breathing or increased movement during sleep. Other signs and symptoms include an irregular sleep and wake cycle and difficulty falling asleep.
There are many different types of sleep disorders. They’re often grouped into categories that explain why they happen or how they affect you. Sleep disorders can also be grouped according to behaviors, problems with your natural sleep-wake cycles, breathing problems, difficulty sleeping or how sleepy you feel during the day.
Some common types of sleep disorders include:
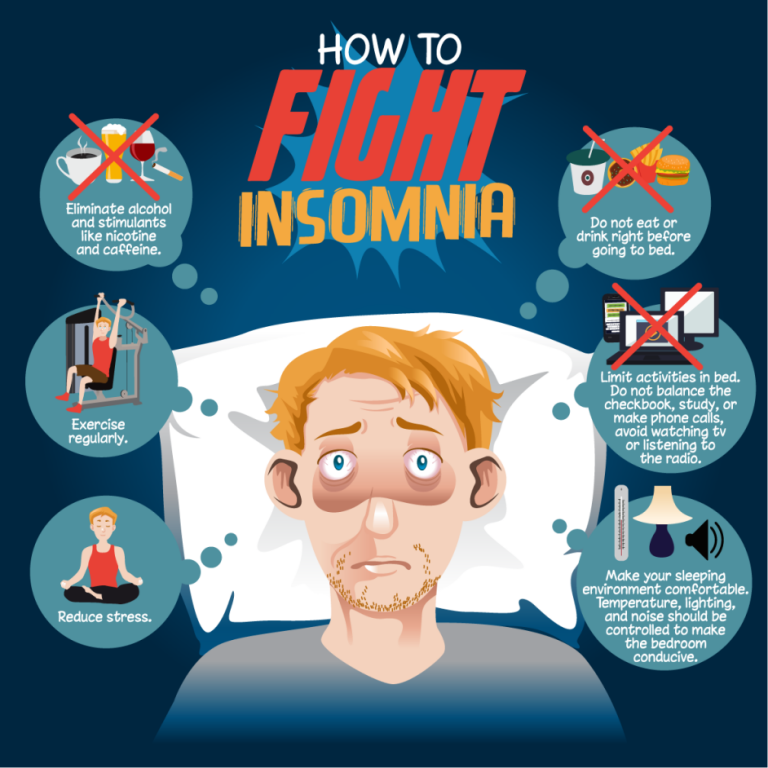
- Insomnia, in which you have difficulty falling asleep or staying asleep throughout the night.
- Sleep apnea, in which you experience abnormal patterns in breathing while you are asleep. There are several types of sleep apnea.
- Restless legs syndrome (RLS), a type of sleep movement disorder. Restless legs syndrome, also called Willis-Ekbom disease, causes an uncomfortable sensation and an urge to move the legs while you try to fall asleep.
- Narcolepsy, a condition characterized by extreme sleepiness during the day and falling asleep suddenly during the day.
There are many ways to help diagnose sleep disorders. Doctors can usually treat most sleep disorders effectively once they’re correctly diagnosed.
Symptoms
Symptoms of sleep disorders include being very sleepy during the daytime and having trouble falling asleep at night. Some people may fall asleep at inappropriate times, such as while driving. Other symptoms include breathing in an unusual pattern or feeling an uncomfortable urge to move while you are trying to fall asleep. Unusual or bothersome movements or experiences during sleep are also possible. Having an irregular sleep and wake cycle is another symptom of sleep disorders.
Sleep terrors (night terrors)
Sleep terrors are times of screaming or crying, intense fear, and sometimes waving arms and legs when not fully awake. Also known as night terrors, sleep terrors may lead to sleepwalking. Like sleepwalking, sleep terrors are a type of parasomnia. Parasomnias are disturbing or strange behaviors or experiences during sleep. A sleep terror usually lasts from seconds to a few minutes, but it may last longer.
Sleep terrors may happen in children between the ages of 1 and 12 years. They happen much less often in adults. Although sleep terrors can be frightening to those around the person with sleep terrors, they aren’t usually a cause for concern. Most children outgrow sleep terrors by their teenage years.
Sleep terrors may need treatment if they cause problems with getting enough sleep or cause a safety risk.
Symptoms
Sleep terrors differ from nightmares. A nightmare is a bad dream. The person who has a nightmare wakes up from the dream and may remember details. A person who has a sleep terror remains asleep. Children usually don’t remember anything about their sleep terrors in the morning. Adults may recall part of a dream they had during the sleep terrors.
Sleep terrors generally happen in the first part of sleep time, and rarely during naps. A sleep terror may lead to sleepwalking.
During a sleep terror, a person may:
- Start by screaming, shouting or crying.
- Sit up in bed and look scared.
- Stare wide-eyed.
- Sweat, breathe heavily, and have a racing pulse, flushed face and enlarged pupils.
- Kick and thrash.
- Be hard to wake up and be confused if awakened.
- Not be comforted or soothed.
- Have no or little memory of the event the next morning.
- Possibly, get out of bed and run around the house or have aggressive behavior if blocked or held back.
When to see a doctor
Occasional sleep terrors aren’t usually a cause for concern. If your child has sleep terrors, you can simply mention them at a routine well-child exam. But if you have concerns for you or your child, talk to your doctor or other healthcare professional sooner, especially if sleep terrors:
- Happen more often.
- Regularly disrupt the sleep of the person with sleep terrors or other family members.
- Lead to safety concerns or injury.
- Result in daytime symptoms of extreme sleepiness or problems with daily activities.
- Continue beyond the teen years or start as an adult.
Causes
Sleep terrors are a type of parasomnia. A parasomnia is a disturbing or strange behavior or experience during sleep. People who have sleep terrors don’t completely wake up from sleep during the episodes. Their appearance may suggest they are awake, but they remain partially asleep.
Several issues can contribute to sleep terrors, such as:
- Serious lack of sleep and extreme tiredness.
- Stress.
- Sleep schedule changes, travel or sleep interruptions.
- Fever.
Sleep terrors sometimes can be triggered by conditions that interfere with sleep, such as:
- Sleep-disordered breathing — a group of disorders that include breathing patterns that are not typical during sleep. The most common type of sleep-disordered breathing is obstructive sleep apnea.
- Restless legs syndrome.
- Some medicines.
- Mood disorders, such as depression and anxiety.
- Alcohol use.
Risk factors
Sleep terrors are more common if family members have a history of sleep terrors or sleepwalking.
Complications
Some complications that may result from sleep terrors include:
- Being too sleepy during the day, which can lead to problems at school or work or with everyday tasks.
- Disturbed sleep.
- Embarrassment about the sleep terrors or problems with relationships.
- Injury to the person having a sleep terror or, rarely, to someone nearby.