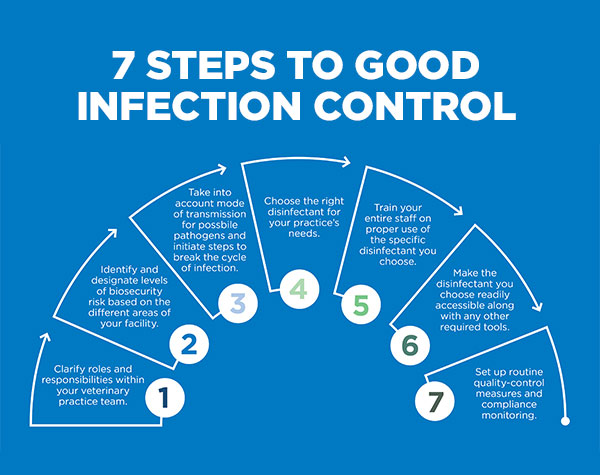
Infection Control
How Infections Spread
Germs are a part of everyday life and are found in our air, soil, water, and in and on our bodies. Some germs are helpful, others are harmful. Many germs live in and on our bodies without causing harm and some even help us to stay healthy. Only a small portion of germs are known to cause infection.
How Do Infections Occur?
An infection occurs when germs enter the body, increase in number, and cause a reaction of the body.
Three things are necessary for an infection to occur:
- Source: Places where infectious agents (germs) live (e.g., sinks, surfaces, human skin)
- Susceptible Person with a way for germs to enter the body
- Transmission: a way germs are moved to the susceptible person
Click on a tab below to learn more.
- Source
- Susceptible Person
- Transmission
Source
A Source is an infectious agent or germ and refers to a virus, bacteria, or other microbe.
In healthcare settings, germs are found in many places. People are one source of germs including:
- Patients
- Healthcare workers
- Visitors and household members
People can be sick with symptoms of an infection or colonized with germs (not have symptoms of an infection but able to pass the germs to others).
Germs are also found in the healthcare environment. Examples of environmental sources of germs include:
- Dry surfaces in patient care areas (e.g., bed rails, medical equipment, countertops, and tables)
- Wet surfaces, moist environments, and biofilms (e.g., cooling towers, faucets and sinks, and equipment such as ventilators)
- Indwelling medical devices (e.g., catheters and IV lines)
- Dust or decaying debris (e.g., construction dust or wet materials from water leaks)
Susceptible Person
A susceptible person is someone who is not vaccinated or otherwise immune, or a person with a weakened immune system who has a way for the germs to enter the body. For an infection to occur, germs must enter a susceptible person’s body and invade tissues, multiply, and cause a reaction.
Devices like IV catheters and surgical incisions can provide an entryway, whereas a healthy immune system helps fight infection.
When patients are sick and receive medical treatment in healthcare facilities, the following factors can increase their susceptibility to infection.
- Patients in healthcare who have underlying medical conditions such as diabetes, cancer, and organ transplantation are at increased risk for infection because often these illnesses decrease the immune system’s ability to fight infection.
- Certain medications used to treat medical conditions, such as antibiotics, steroids, and certain cancer fighting medications increase the risk of some types of infections.
- Lifesaving medical treatments and procedures used in healthcare such as urinary catheters, tubes, and surgery increase the risk of infection by providing additional ways that germs can enter the body.
Recognizing the factors that increase patients’ susceptibility to infection allows providers to recognize risks and perform basic infection prevention measures to prevent infection from occurring.
Transmission
Transmission refers to the way germs are moved to the susceptible person.
Germs don’t move themselves. Germs depend on people, the environment, and/or medical equipment to move in healthcare settings.
There are a few general ways that germs travel in healthcare settings – through contact (i.e., touching), sprays and splashes, inhalation, and sharps injuries (i.e., when someone is accidentally stuck with a used needle or sharp instrument).
- Contact moves germs by touch (example: MRSA or VRE). For example, healthcare provider hands become contaminated by touching germs present on medical equipment or high touch surfaces and then carry the germs on their hands and spread to a susceptible person when proper hand hygiene is not performed before touching the susceptible person.
- Sprays and splashes occur when an infected person coughs or sneezes, creating droplets which carry germs short distances (within approximately 6 feet). These germs can land on a susceptible person’s eyes, nose, or mouth and can cause infection (example: pertussis or meningitis).
- Close range inhalation occurs when a droplet containing germs is small enough to breathe in but not durable over distance.
- Inhalation occurs when germs are aerosolized in tiny particles that survive on air currents over great distances and time and reach a susceptible person. Airborne transmission can occur when infected patients cough, talk, or sneeze germs into the air (example: TB or measles), or when germs are aerosolized by medical equipment or by dust from a construction zone (example: Nontuberculous mycobacteria or aspergillus).
- Sharps injuries can lead to infections (example: HIV, HBV, HCV) when bloodborne pathogens enter a person through a skin puncture by a used needle or sharp instrument.
What is breast Cancer?
Breast Cancer Awareness
Wondering when to start or how often to get screening mammograms?
Ask your doctor when you should get a mammogram.
Other than skin cancer, breast cancer is the most common cancer among American women. Mammograms are the best way to find breast cancer early, when it is easier to treat and before it is big enough to feel or cause symptoms.
Kinds of Breast Cancer
The most common kinds of breast cancer are—
- Invasive ductal carcinoma. The cancer cells begin in the ducts and then grow outside the ducts into other parts of the breast tissue. Invasive cancer cells can also spread, or metastasize, to other parts of the body.
- Invasive lobular carcinoma. Cancer cells begin in the lobules and then spread from the lobules to the breast tissues that are close by. These invasive cancer cells can also spread to other parts of the body.
What Are the Symptoms?
There are different symptoms of breast cancer, and some people have no symptoms at all. Symptoms can include—
- Any change in the size or the shape of the breast.
- Pain in any area of the breast.
- Nipple discharge other than breast milk (including blood).
- A new lump in the breast or underarm.
If you have any signs that worry you, see your doctor right away.
How Can I Lower My Risk?
You can do things to help lower your breast cancer risk.
- Keep a healthy weight and exercise regularly.
- Choose not to drink alcohol, or drink alcohol in moderation.
- If you are taking hormone replacement therapy or birth control pills, ask your doctor about the risks.
- Breastfeed your children, if possible.
Fast Facts About Breast Cancer
- Each year in the United States, about 240,000 women get breast cancer and 42,000 women die from the disease.
- Men also get breast cancer, but it is not very common. About 1 out of every 100 breast cancers diagnosed in the United States is found in a man.
- Most breast cancers are found in women who are 50 years old or older, but breast cancer also affects younger women.
How is a mammogram done?
You will stand in front of a special X-ray machine. A technologist will place your breast on a plastic plate. Another plate will firmly press your breast from above. The plates will flatten the breast, holding it still while the X-ray is being taken. You will feel some pressure. The steps are repeated to make a side view of the breast. The other breast will be X-rayed in the same way. You will then wait while the technologist checks the X-rays to make sure the pictures do not need to be redone. Keep in mind that the technologist cannot tell you the results of your mammogram. Each woman’s mammogram may look a little different because all breasts are a little different.
What You Can Do to Protect Youth From the Harms of Vaping
Parents and educators—including teachers, administrators, and coaches—can play an important role in protecting youth from e-cigarettes, also known as vapes. As students go back to school, it’s the perfect time to educate them about the dangers of vaping.
E-cigarettes are electronic devices that heat a liquid and produce an aerosol, or a mix of small particles in the air. This aerosol is breathed into the lungs of the person using the device. E-cigarette aerosol can contain harmful and potentially harmful substances. While use of e-cigarettes is unsafe for everyone, this is especially true for kids, teens, and young adults.
E-cigarettes, or vapes, are known by many different names. They are also called “e-cigs,” “e-hookahs,” “mods,” “vape pens,” “tank systems,” and “electronic nicotine delivery systems (ENDS).” E-cigarettes come in many shapes and sizes. Some are made to be recharged, some to be refilled, and some to be thrown away (disposable).
E-cigarette Use Among Youth
E-cigarettes are the most commonly used tobacco product among U.S. middle and high school students.
- In 2022, about 1 in 10 or 2.55 million U.S. middle and high school students used e-cigarettes at least once in the past 30 days, including 3.3% of middle school students and 14.1% of high school students.
Disposable e-cigarettes are the most commonly used device type among U.S. middle and high school students who vape. In addition, nearly 85% of middle and high school students who used e-cigarettes reported using flavored e-cigarettes. Many e-cigarettes come in kid-friendly flavors—like candy, desserts, other sweets, mint, and menthol. This makes them more appealing to youth.
- Among middle and high school students who currently used any type of flavored e-cigarette in 2022, the most commonly used flavors were fruit (69.1%), candy, desserts, or other sweets (38.3%), mint (29.4%), and menthol (26.6%).
Health Risks of Vaping for Youth
CDC: Educators: What Are the Health Risks of Vaping for Youth?
From a US national health authority
Vaping can have health risks for youth. Most vapes have nicotine in them, which is highly addictive. Nicotine use in adolescence:
- Can harm brain development, which continues until about age 25.
- Can impact attention, learning, mood, and impulse control.
- May increase risk for future addiction to other drugs.
Not only can nicotine in e-cigarettes pose health risks for youth, but youth who vape may also be more likely to go on to use regular cigarettes.
In addition to nicotine, e-cigarette aerosol can contain other harmful and potentially harmful substances. These substances include:
- Cancer-causing chemicals
- Volatile organic compounds
- Ultrafine particles
- Flavorings that have been linked to lung disease
- Heavy metals such as nickel, tin, and lead
Nicotine Addiction Can Be a Source of Stress
When a person is dependent on (or is addicted to) nicotine and stops using it, their body and brain must get used to not having nicotine. This can result in temporary symptoms of nicotine withdrawal. People might keep using tobacco products, like vapes, to try to make these symptoms feel better. Nicotine withdrawal symptoms include:
- Irritability
- Restlessness
- Feeling anxious or depressed
- Trouble sleeping
- Problems concentrating
- Craving nicotine
Youth might turn to vaping to try to deal with stress or anxiety. This can create a cycle of nicotine addiction, which can also be a source of stress.
Youth vaping and cigarette use have also been linked to mental health symptoms, such as depression.
All signs point to a rise in Covid
Covid hospitalizations, deaths and wastewater data — among other indicators — are all increasing as the U.S. heads into fall.
Signs in the U.S. continue to point to a rise in Covid activity as fall approaches.
Hospitalizations are rising. Deaths have ticked up. Wastewater samples are picking up the virus, as are labs across the country.
“Every single one of those things is showing us that we have increased rates of Covid transmission in our communities,” said Jodie Guest, a professor of epidemiology at Emory University’s Rollins School of Public Health in Atlanta.
While individual cases have become more difficult to track as states are no longer required to report numbers to the Centers for Disease Control and Prevention and at-home test use has increased, experts have turned to other tools to track the virus.
Hospitalizations, for example, are “a very good indicator of severity of Covid disease,” Guest said.
The number of hospitalized Covid patients has continued to rise after hitting an all-time low in late June. The week ending Aug. 26, the most recent date for which data is available, there were just over 17,400 people hospitalized with Covid, up nearly 16% from the previous week, according to the CDC.
The increase comes even as hospital testing protocols have changed. At the height of the pandemic, every patient admitted to the hospital was tested for Covid, whether they had symptoms or not.
“We’re now only testing people who are symptomatic,” said Guest, who added that this makes it difficult to directly compare hospitalization numbers to what was seen previously in the pandemic. Current numbers may be missing asymptomatic cases and therefore be lower than earlier ones.
Dr. Peter Chin-Hong, a professor of medicine at the University of California, San Francisco, said that at his hospital system, 21 patients are hospitalized with Covid. Earlier in the summer, it ranged from 10 to 15 patients, he said, so while the numbers have gone up, it’s nothing like what the hospital saw last winter, when more than 100 patients were hospitalized with Covid.
Emergency room visits with a Covid diagnosis in the U.S. have been on the rise since early July. The week ending Aug. 19 saw 2.3% of ER visits with a Covid diagnosis, up from 0.5% the week ending July 1, according to the CDC.

Wastewater samples are also showing an increase in Covid.
“The wastewater is giving us a pretty clear picture that there has been, you know, quite an uptick in cases in these communities that we’re monitoring recently,” said Marlene Wolfe, an assistant professor of environmental health at Emory University and program director for WastewaterSCAN, which monitors 171 wastewater treatment sites in 34 states.
“We are in a period of higher levels of SARS-CoV-2 in wastewater right now, and that’s associated with an increase in the number of cases in the community,” Wolfe said, referring to the virus that causes Covid.
Deaths appear to be up slightly, after a summer in which weekly totals hovered under 600 — and occasionally dipped below 500 — for much of June and July. The week ending Aug. 19 saw 636 deaths, according to the CDC.
Other signs of increased Covid activity are easy for the general public to spot.
“When you know multiple people who are currently experiencing symptoms of Covid or tested positive of Covid, that’s another great marker to recognize how much of it there is in your community,” Guest said. “We also see Covid tests being absent on their shelves in Walgreens and CVS and other places as well, because people have more transmission right now.”
Is the BA.2.86 variant to blame?
Experts say no. While there are a slew of variants in circulation in the U.S., BA.2.86 remains very rare. As of Aug. 30, the CDC said that the variant had been detected in four states: in Michigan, New York, Ohio and Virginia.
Instead, the current increases in cases and hospitalizations are likely due to the XBB subvariants, the CDC says. Those include subvariants called EG.5 (which accounted for 21.5% of new cases for the week ending Sept. 2) and FL.1.5.1 (14.5% of new cases).
What’s more, the BA.2.86 variant — dubbed “Pirola” by some on social media — may not be as bad as scientists initially feared.
“Just looking at the virus, structurally, it looks scary with all the mutations compared to XBB.1.5, which the vaccine was based on,” Chin-Hong said. XBB.1.5 is the subvariant that the new boosters, coming out later this month, were designed to target.
But new research shows that people who had been infected with an XBB subvariant in the past six months performed well against BA.2.86, Chin-Hong said. That suggests that the new boosters would be able to fend off this variant, even if it does become dominant, he added.
How can people protect themselves and others?
The advice to protect against Covid remains the same, including masking, staying home when sick, getting tested for Covid if exposed or symptomatic, and staying up to date on vaccines.
“If you’re in a crowded situation, recognizing the odds are that someone in that room probably does have Covid-19 at this point in time and so masking is a great way to protect yourself and to protect others that you’re going to be around later,” Guest said.
Chin-Hong advised carrying around a mask and bring it out for risky situations, like while using public transit or at the airport.
He also suggested that people have a plan to get therapies like Paxlovid or remesdivir if they test positive, particularly older or immune-comprosmised individuals who are at higher risk for complications.
The CDC also notes that improving ventilation indoors can help protect against infection. That can involve opening windows, turning on fans and using air filters to clean the air.
The Food and Drug Administration and the CDC are expected to sign off on new Covid boosters in the next few weeks, which target one of the XBB variants.
Guest said people should wait for the new boosters to become available. “But we want people to get that booster when it comes out,” she said.
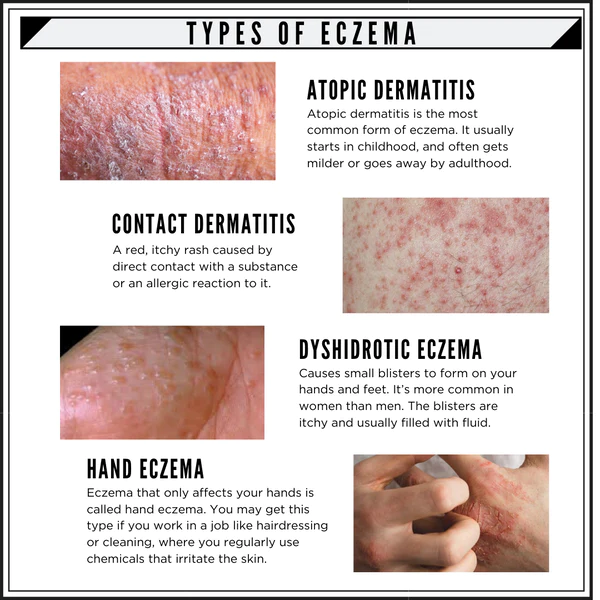
What to know about eczema
Eczema is a condition in which patches of skin become inflamed, itchy, cracked, and rough. Some types can also cause blisters. Home remedies and medical treatment can help manage and prevent flares.
Different types and stages of eczema affect 31.6 million people in the United States, which equals more than 10% of the population.
Many people use the word eczema when referring to atopic dermatitis, which is the most common type. The term atopic refers to a collection of conditions that involve the immune system, including atopic dermatitis, asthma, and hay fever. The word dermatitis refers to inflammation of the skin.
Certain foods, such as nuts and dairy, can trigger symptoms of eczema. Environmental triggers can include smoke, pollen, soaps, and fragrances. Eczema is not contagious.
About a quarter of children in the U.S. have the condition, as well as 10% of African Americans, 13% of Asian Americans and Pacific Islanders, 13% of Native Americans, and 11% of people who are white.
Some people outgrow the condition, while others will continue to have it throughout adulthood. This article will explain what eczema is and discuss its symptoms, treatments, causes, and types.
The symptoms of atopic dermatitis can vary depending on a person’s age and the condition’s severity and can vary by individual.
People with the condition will often experience periods of time when their symptoms worsenTrusted Source, followed by periods of time when their symptoms will improve or clear up.
The following sections will outline some of the potential differences in symptoms in more detail.
General eczema symptoms
In most cases eczema symptoms are mild. The most common symptoms of atopic dermatitis include:
- dry, scaly skin
- skin flushing
- itching
- open, crusted, or weeping sores
People with severe eczema may need more intensive treatment to relieve their symptoms. Continuous rubbing and scratching can also lead to skin infections.
Eczema symptoms in People of Color
In People of Color, an eczema rash may appear gray or brown. This can make outbreaks harder to see.
However, People of Color who get eczema may also get dark or light skin patches even after eczema symptoms go away. These can last a long time. Doctors call these patches hyperpigmentation and depigmentation or hypopigmentation.
A dermatologist can evaluate these patches, which may respond to treatments like steroid creams.
Infant eczema symptoms
The following atopic dermatitis symptoms are common in babies under the age of 2:
- rashes on the scalp and cheeks
- rashes that bubble up before leaking fluid
- rashes that can cause extreme itchiness, which may interfere with sleeping
Childhood eczema symptoms
The following atopic dermatitis symptoms are common in children age 2 and above:
- rashes that appear behind the creases of elbows or knees
- rashes that appear on the neck, wrists, ankles, and the crease between the buttocks and legs
- bumpy rashes
- rashes that can become lighter or darker
- skin thickening, also known as lichenification, which can then develop into a permanent itch
Most people with the condition develop it before the age of 5 years. An estimated 60% of children will no longer show symptoms by adolescence.
African American and Hispanic children may have more severe eczema than children who are white.
Symptoms in adults
The following atopic dermatitis symptoms are common in adults:
- rashes that are more scaly than those occurring in children
- rashes that commonly appear in the creases of the elbows or knees or the nape of the neck
- rashes that cover much of the body
- very dry skin on the affected areas
- rashes that are permanently itchy
- skin infections
Adults who developed atopic dermatitis as children but no longer experience the condition may still have dry or easily irritated skin, hand eczema, and eczema on the eyelids.
The appearance of skin affected by atopic dermatitis will depend on how much a person scratches and whether the skin is infected. Scratching and rubbing can further irritate the skin, increase inflammation, and make the itching worse.
There is currently no cure for eczema. Treatment for the condition aims to heal the affected skin and prevent flares of symptoms.
Doctors will suggest a treatment plan based on an individual’s age, symptoms, and current state of health.
For some people, eczema goes away over time. For others, however, it is a lifelong condition.
The sections below will list some treatment options.
Medications
Doctors can prescribe several medications to treat the symptoms of eczema, including:
- Topical corticosteroid creams and ointments: These are anti-inflammatory medications and should relieve the main symptoms of eczema, such as inflammation and itchiness. People can apply them directly to the skin. Some people may benefit from prescription-strength medications.
- Oral medications: If topical treatments are not effective, a doctor may prescribe oral medications like systemic corticosteroids or immunosuppresants. These are available as injections or oral tablets. People should only use them for short periods of time. Also, it is important to note that the symptoms may worsen upon stopping these drugs if the person is not already taking another medication for the condition.
- Antibiotics: Doctors prescribe antibiotics if eczema occurs alongside a bacterial skin infection.
- Antihistamines: These can reduce the risk of nighttime scratching, as they tend to cause drowsiness.
- Topical calcineurin inhibitors: This drug suppresses the activities of the immune system. It decreases inflammation and helps prevent flares.
- Barrier repair moisturizers: These reduce water loss and work to repair the skin.
- Phototherapy: This involves exposure to UVA or UVB waves. This method can treat moderate dermatitis. A doctor will monitor the skin closely throughout the treatment.
- Injected biologic drugs: These medications block proteins in the immune system to limit immune system response.
To treat moderate to severe eczema, a doctor may prescribe a combination of topical and systemic treatments, such as biologics.
The Food and Drug Administration (FDA) has approved two biologics to treat eczema: dupilumab (Dupixent) and tralokinumab-ldrm (Adbry).
These biologics target specific proteins in the immune system that trigger inflammation, which can help reduce eczema symptoms. They can sometimes cause side effects, which are usually mild and manageable.
Even after an area of skin has healed, it is important to keep looking after it, as it may easily become irritated again.
Even though the condition itself is not currently curable, each person should consult with a doctor to get a tailored treatment plan.
Home care
There are several things that people with eczema can do to support skin health and alleviate symptoms.
They can try:
- taking lukewarm baths
- applying moisturizer within 3 minutes of bathing to “lock in” moisture
- moisturizing every day
- wearing cotton and soft fabrics
- avoiding rough, scratchy fibers and tight fitting clothing
- using a humidifier in dry or cold weather
- using a mild soap or a non-soap cleanser when washing
- taking extra precautions to prevent eczema flares in winter
- air drying or gently patting the skin dry with a towel, rather than rubbing the skin dry after bathing or taking a shower
- where possible, avoiding rapid changes of temperature and activities that cause sweating
- learning and avoiding individual eczema triggers
- keeping fingernails short to prevent scratching from breaking the skin
People can also try various natural remedies for eczema, including aloe vera, coconut oil, and apple cider vinegar.
Researchers do not know the definitive cause of eczema, but many health professionals believe that it develops from a combination of genetic and environmental factors.
Children are more likely to develop eczema if a parent has it or another atopic condition. If both parents have an atopic condition, the risk is even higher.
Some environmental factors may also bring out the symptoms of eczema. These include:
- Irritants: These include soaps, detergents, shampoos, disinfectants, juices from fresh fruits, meats, and vegetables.
- Allergens: Dust mites, pets, pollens, and mold can all lead to eczema. This is known as allergic eczema.
- Microbes: These include bacteria such as Staphylococcus aureus, viruses, and certain fungi.
- Hot and cold temperatures: Very hot and very cold weather, high and low humidity, and perspiration from exercise can bring out eczema.
- Foods: Dairy products, eggs, nuts and seeds, soy products, and wheat can cause eczema flares.
- Stress: This is not a direct cause of eczema, but it can make the symptoms worse.
- Hormones: Females may experience increased eczema symptoms when their hormone levels are changing, such as during pregnancy and at certain points in the menstrual cycle.
There are several types of eczema. Besides atopic dermatitis, other types include:
- Allergic contact dermatitis: This is a skin reaction that occurs following contact with a substance or allergen that the immune system recognizes as foreign.
- Dyshidrotic eczema: This refers to irritation of the skin on the palms of the hands and soles of the feet. It is characterized by blisters.
- Neurodermatitis: This leads to scaly patches of skin on the head, forearms, wrists, and lower legs. It occurs due to a localized itch, such as from an insect bite.
- Discoid eczema: Also known as nummular eczema, this type presents as circular patches of irritated skin that can be crusted, scaly, and itchy.
- Stasis dermatitis: This refers to skin irritation of the lower leg. It is usually related to circulatory problems.
Eczema is a common inflammatory skin condition. The most common type is called atopic dermatitis. Eczema is most common in children, but the majority of children will grow out of it by the time they reach adolescence.
Eczema can cause discomfort and can vary in severity. It can present differently depending on a person’s age. In people with darker skin tones, the symptoms may be harder to see.
Although there is currently no cure, people can treat and prevent eczema flares using home remedies, moisturizers, medications, and lifestyle changes.
Healthy Lifestyles
A healthy lifestyle can help you thrive as you move through your life’s journey. Making healthy choices isn’t always easy – it can be hard to find the time and energy to exercise regularly or prepare healthy meals. However, your efforts will pay off in many ways, and for the rest of your life.
Steps you can take:
- Be physically active for 30 minutes most days of the week. Break this up into three 10-minute sessions when pressed for time. Healthy movement may include walking, sports, dancing, yoga or running.
- Eat a well-balanced, low-fat diet with lots of fruits, vegetables, and whole grains. Choose a diet that’s low in saturated fat and cholesterol, and moderate in sugar, salt and total fat.
- Avoid injury by wearing seatbelts and bike helmets, using smoke and carbon monoxide detectors in the home, and using street smarts when walking alone. If you own a gun, recognize the dangers of having a gun in your home. Use safety precautions at all times.
- Don’t smoke, and quit if you do. Ask your health care provider for help. UCSF offers a smoking cessation program.
- If you drink alcohol, drink in moderation. Never drink before or when driving, or when pregnant.
- Ask someone you trust for help if you think you might be addicted to drugs or alcohol.
- Help prevent sexually transmitted infections (STIs) and HIV/AIDS by using condoms every time you have sexual contact. Keep in mind, condoms are not 100 percent foolproof, so discuss STI screening with your provider. Birth control methods other than condoms, such as pills and implants, won’t protect you from STIs or HIV.
- Brush your teeth after meals with a soft or medium bristled toothbrush. Also brush after drinking, before going to bed. Use dental floss daily.
- Stay out of the sun, especially between 10 a.m. and 3 p.m. when the sun’s harmful rays are strongest. Don’t think you are safe if it is cloudy or if you are in the water, as harmful rays pass through both. Use a broad spectrum sunscreen that guards against both UVA and UVB rays, with a sun protection factor (SPF) of 15 or higher. Select sunglasses that block 99 to 100 percent of the sun’s rays.
Healthy Outlook
You may feel pulled in different directions and experience stress from dealing with work, family and other matters, leaving little time for yourself. Learning to balance your life with some time for yourself will pay off with big benefits – a healthy outlook and better health.
Steps you can take:
- Stay in touch with family and friends.
- Be involved in your community.
- Maintain a positive attitude and do things that make you happy.
- Keep your curiosity alive. Lifelong learning is beneficial to your health.
- Healthy intimacy takes all forms but is always free of coercion.
- Learn to recognize and manage stress in your life. Signs of stress include trouble sleeping, frequent headaches and stomach problems; being angry a lot; and turning to food, drugs and alcohol to relieve stress.
Good ways to deal with stress include regular exercise, healthy eating habits, and relaxation exercises such as deep breathing or meditation. Talking to trusted family members and friends can help a lot. Some women find that interacting with their faith community is helpful in times of stress. - Get enough sleep and rest – adults need around eight hours of sleep a night.
- Talk to your health care provider if you feel depressed for more than a few days. Depression is a treatable illness. Signs of depression include feeling empty and sad, crying a lot, loss of interest in life, and thoughts of death or suicide. If you or someone you know has thoughts of suicide, get help right away. Call 911, a local crisis center or (800) SUICIDE.