Insomnia
Insomnia
Insomnia is a common sleep disorder that can make it hard to fall asleep or stay asleep. It also can cause you to wake up too early and not be able to get back to sleep. You may still feel tired when you wake up. Insomnia can drain your energy level and affect your mood. It also can affect your health, work performance and quality of life.
How much sleep is enough varies from person to person. But most adults need 7 to 9 hours a night.
At some point, many adults have short-term insomnia. This can last for days or weeks. Short-term insomnia is usually due to stress or a distressing event. But some people have long-term insomnia, also called chronic insomnia. This lasts for three months or more. Insomnia may be the main problem, or it may be related to other medical conditions or medicines.
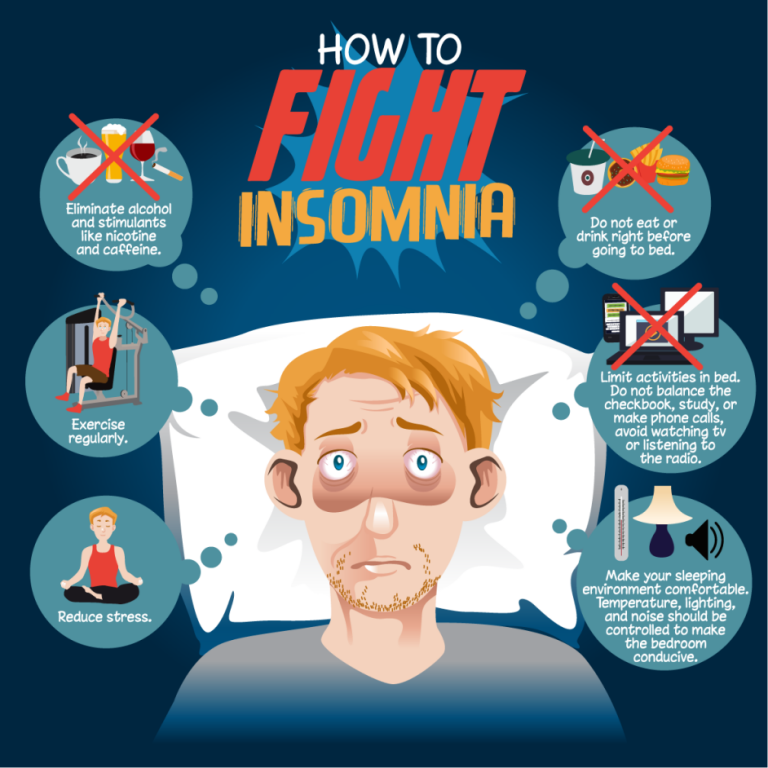
You do not have to put up with sleepless nights. Simple changes in your daily habits often can help.
Symptoms
Insomnia symptoms may include:
- Having a hard time falling asleep at night.
- Waking up during the night.
- Waking up too early.
- Feeling tired or sleepy during the day.
- Feeling cranky, depressed or anxious.
- Having a hard time paying attention, focusing on tasks or remembering.
- Making more errors or having more accidents.
- Having ongoing worries about sleep.
When to see a doctor
If insomnia makes it hard for you to do daily activities, see your doctor or another primary care professional. Your doctor will search for the cause of your sleep problem and help treat it. If it’s thought that you could have a sleep disorder, your doctor might suggest going to a sleep center for special testing.
Causes
Insomnia may be the main problem or it may be related to other conditions.
Long-term insomnia is usually due to stress, life events or habits that disrupt sleep. While treating the cause of your sleep problem may stop your insomnia, sometimes it can last for years.
Common causes of long-term insomnia include:
- Stress. Concerns about work, school, health, money or family can keep your mind active at night, making it hard to sleep. Stressful life events, such as the death or illness of a loved one, divorce, or a job loss, also may lead to insomnia.
- Travel or work schedule. Your body’s “internal clock,” known as circadian rhythms, guides things such as your sleep-wake cycle, metabolism and body temperature. Disrupting these rhythms can lead to insomnia. Causes include feeling jet lag from traveling across multiple time zones, working a late or early shift, or changing shifts often.
- Poor sleep habits. Poor sleep habits include going to bed and waking up at different times each day, taking naps, being too active before bedtime and having a sleep area that is not comfortable. Other poor sleep habits include working, eating or watching TV while in bed. Using computers or smartphones, playing video games, or watching TV just before bed can disrupt your sleep cycle.
- Eating too much late in the evening. Having a light snack before bedtime is OK. But eating too much may cause you to feel uncomfortable while lying down. Many people also have heartburn. This is when stomach acid backs up into the tube that carries food from your mouth to your stomach. This tube is called the esophagus. Heartburn may keep you awake.
- Mental health disorders. Anxiety disorders, such as post-traumatic stress disorder, may disrupt your sleep. Waking up too early can be a sign of depression. Insomnia often occurs with other mental health conditions.
- Medicines. Many prescription drugs can interfere with sleep, such as certain antidepressants and medicines for asthma or blood pressure. Many medicines available without a prescription, such as some pain medicines, allergy and cold medicines, and weight-loss products, contain caffeine and other stimulants that can disrupt sleep.
- Medical conditions. Examples of conditions linked with insomnia include ongoing pain, cancer, diabetes, heart disease, asthma, gastroesophageal reflux disease (GERD), overactive thyroid, Parkinson’s disease and Alzheimer’s disease.
- Sleep-related disorders. Sleep apnea causes you to stop breathing at times during the night, disrupting your sleep. Restless legs syndrome causes a strong uncomfortable urge to move your legs when trying to fall asleep. This may keep you from falling asleep or getting back to sleep.
- Caffeine, nicotine and alcohol. Coffee, tea, cola and other drinks that have caffeine are stimulants. Drinking them in the late afternoon or evening can keep you from falling asleep at night. Nicotine in tobacco products is another stimulant that can disrupt sleep. Alcohol may help you fall asleep, but it prevents deeper stages of sleep and often results in waking up in the middle of the night.
Insomnia and aging
Insomnia becomes more common with age. As you get older, you may:
- Change your sleep patterns. Sleep often becomes less restful as you age, so noise or other changes in your surroundings are more likely to wake you. With age, your internal clock often moves forward in time, so you get tired earlier in the evening and wake up earlier in the morning. But older people typically still need the same amount of sleep as younger people.
- Change your level of activity. You may be less physically or socially active. A lack of activity can disrupt a good night’s sleep. Also, the less active you are, the more likely you may be to take a daily nap. Napping can disrupt sleep at night.
- Have changes in your health. Ongoing pain from conditions such as arthritis or back problems, as well as depression or anxiety, can disrupt sleep. Issues that make it more likely that you’ll need to urinate during the night, such as prostate or bladder problems, can disrupt sleep. Sleep apnea and restless legs syndrome become more common with age.
- Take more medicines. Older people typically use more prescription drugs than younger people do. This raises the chance of insomnia related to medicines.
Insomnia in children and teens
Sleep problems may be a concern for children and teenagers too. But some children and teens simply have trouble getting to sleep or resist a regular bedtime because their internal clocks are more delayed. They want to go to bed later and sleep later in the morning.
Risk factors
Nearly everyone has an occasional sleepless night. But you’re more likely to have insomnia if:
- You’re a woman. Changes in hormones during the menstrual cycle and in menopause may play a role. During menopause, night sweats and hot flashes often disrupt sleep. Insomnia also is common during pregnancy.
- You’re over 60. Because of changes in sleep patterns and health, it’s more likely you’ll have insomnia as you get older.
- You have a mental health or physical health condition. Many issues that affect your mental or physical health can disrupt sleep.
- You’re under a lot of stress. Being stressed can cause short-term insomnia. Major or long-lasting stress can lead to long-term insomnia.
- You do not have a regular schedule. For example, changing shifts at work or traveling can disrupt your sleep-wake cycle.
Complications
Sleep is as important to your health as a healthy diet and regular physical activity. Whatever is keeping you from sleeping, insomnia can affect you mentally and physically. People with insomnia report a lower quality of life compared with people who sleep well.
Complications of insomnia may include:
- Lower performance on the job or at school.
- Slowed reaction time while driving and a higher risk of accidents.
- Mental health conditions, such as depression, anxiety or substance misuse.
- Higher risk or worsening of long-term diseases or conditions, such as high blood pressure and heart disease.
Prevention
Good sleep habits like these can help prevent insomnia:
- Keep the time you go to bed and the time you wake up the same every day, including weekends.
- Stay active. Regular activity can lead to a good night’s sleep.
- Limit naps or do not nap at all.
- Limit or do not use caffeine, alcohol and nicotine.
- Do not eat large meals or drink a lot of fluids before bed.
- Make your bedroom comfortable for sleep and only use it for sex or sleep.
- Create a relaxing bedtime ritual, such as taking a warm bath, reading or listening to soft music.
Prostate Cancer
Prostate cancer
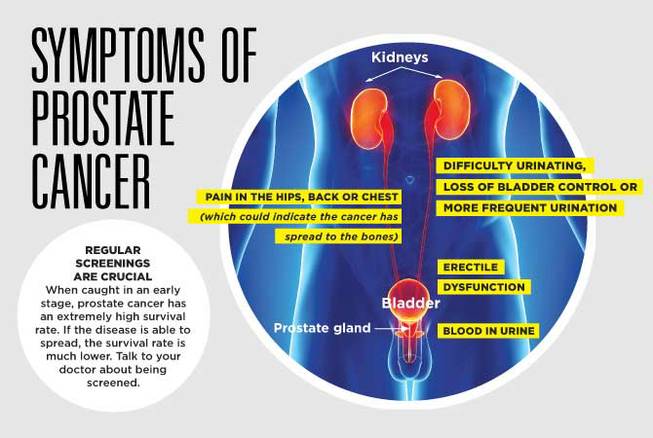
Prostate cancer is cancer that occurs in the prostate. The prostate is a small walnut-shaped gland in males that produces the seminal fluid that nourishes and transports sperm.
Prostate cancer is one of the most common types of cancer. Many prostate cancers grow slowly and are confined to the prostate gland, where they may not cause serious harm. However, while some types of prostate cancer grow slowly and may need minimal or even no treatment, other types are aggressive and can spread quickly.
Prostate cancer that’s detected early — when it’s still confined to the prostate gland — has the best chance for successful treatment.
Symptoms
Prostate cancer may cause no signs or symptoms in its early stages.
Prostate cancer that’s more advanced may cause signs and symptoms such as:
- Trouble urinating
- Decreased force in the stream of urine
- Blood in the urine
- Blood in the semen
- Bone pain
- Losing weight without trying
- Erectile dysfunction
When to see a doctor
Make an appointment with your doctor if you have any persistent signs or symptoms that worry you.
Causes
It’s not clear what causes prostate cancer.
Doctors know that prostate cancer begins when cells in the prostate develop changes in their DNA. A cell’s DNA contains the instructions that tell a cell what to do. The changes tell the cells to grow and divide more rapidly than normal cells do. The abnormal cells continue living, when other cells would die.
The accumulating abnormal cells form a tumor that can grow to invade nearby tissue. In time, some abnormal cells can break away and spread (metastasize) to other parts of the body.
Risk factors
Factors that can increase your risk of prostate cancer include:
- Older age. Your risk of prostate cancer increases as you age. It’s most common after age 50.
- Race. For reasons not yet determined, Black people have a greater risk of prostate cancer than do people of other races. In Black people, prostate cancer is also more likely to be aggressive or advanced.
- Family history. If a blood relative, such as a parent, sibling or child, has been diagnosed with prostate cancer, your risk may be increased. Also, if you have a family history of genes that increase the risk of breast cancer (BRCA1 or BRCA2) or a very strong family history of breast cancer, your risk of prostate cancer may be higher.
- Obesity. People who are obese may have a higher risk of prostate cancer compared with people considered to have a healthy weight, though studies have had mixed results. In obese people, the cancer is more likely to be more aggressive and more likely to return after initial treatment.
Complications
Complications of prostate cancer and its treatments include:
- Cancer that spreads (metastasizes). Prostate cancer can spread to nearby organs, such as your bladder, or travel through your bloodstream or lymphatic system to your bones or other organs. Prostate cancer that spreads to the bones can cause pain and broken bones. Once prostate cancer has spread to other areas of the body, it may still respond to treatment and may be controlled, but it’s unlikely to be cured.
- Incontinence. Both prostate cancer and its treatment can cause urinary incontinence. Treatment for incontinence depends on the type you have, how severe it is and the likelihood it will improve over time. Treatment options may include medications, catheters and surgery.
- Erectile dysfunction. Erectile dysfunction can result from prostate cancer or its treatment, including surgery, radiation or hormone treatments. Medications, vacuum devices that assist in achieving erection and surgery are available to treat erectile dysfunction.
Prevention
You can reduce your risk of prostate cancer if you:
- Choose a healthy diet full of fruits and vegetables. Eat a variety of fruits, vegetables and whole grains. Fruits and vegetables contain many vitamins and nutrients that can contribute to your health.
Whether you can prevent prostate cancer through diet has yet to be conclusively proved. But eating a healthy diet with a variety of fruits and vegetables can improve your overall health. - Choose healthy foods over supplements. No studies have shown that supplements play a role in reducing your risk of prostate cancer. Instead, choose foods that are rich in vitamins and minerals so that you can maintain healthy levels of vitamins in your body.
- Exercise most days of the week. Exercise improves your overall health, helps you maintain your weight and improves your mood. Try to exercise most days of the week. If you’re new to exercise, start slow and work your way up to more exercise time each day.
- Maintain a healthy weight. If your current weight is healthy, work to maintain it by choosing a healthy diet and exercising most days of the week. If you need to lose weight, add more exercise and reduce the number of calories you eat each day. Ask your doctor for help creating a plan for healthy weight loss.
- Talk to your doctor about increased risk of prostate cancer. If you have a very high risk of prostate cancer, you and your doctor may consider medications or other treatments to reduce the risk. Some studies suggest that taking 5-alpha reductase inhibitors, including finasteride (Propecia, Proscar) and dutasteride (Avodart), may reduce the overall risk of developing prostate cancer. These drugs are used to control prostate gland enlargement and hair loss.
However, some evidence indicates that people taking these medications may have an increased risk of getting a more serious form of prostate cancer (high-grade prostate cancer). If you’re concerned about your risk of developing prostate cancer, talk with your doctor.
10 tips to stay healthy
Staying healthy involves a combination of medical care and a good diet. Here are some tips:
1)Regular Check-ups: Schedule routine check-ups with your healthcare provider to monitor your health and catch any issues early.
2)Stay Active: Engage in regular physical activity to maintain a healthy weight, improve cardiovascular health, and boost mood.
3)Eat a Balanced Diet: Consume a variety of fruits, vegetables, lean proteins, whole grains, and healthy fats. Limit processed foods, sugar, and sodium.
4)Stay Hydrated: Drink plenty of water throughout the day to stay hydrated and support bodily functions.
5)Get Adequate Sleep: Aim for 7-9 hours of quality sleep each night to support overall health and well-being.
6)Manage Stress: Practice stress-reducing techniques such as meditation, deep breathing, or hobbies you enjoy.
7)Limit Alcohol and Avoid Tobacco: Drink alcohol in moderation, if at all, and avoid smoking or using tobacco products.
8)Practice Good Hygiene: Wash your hands frequently, brush and floss your teeth regularly, and maintain good hygiene habits to prevent illness and infection.
9)Stay Informed: Stay informed about health recommendations and guidelines from reliable sources such as healthcare professionals or reputable organizations.
10)Listen to Your Body: Pay attention to your body’s signals and seek medical attention if you experience any concerning symptoms or changes in health.
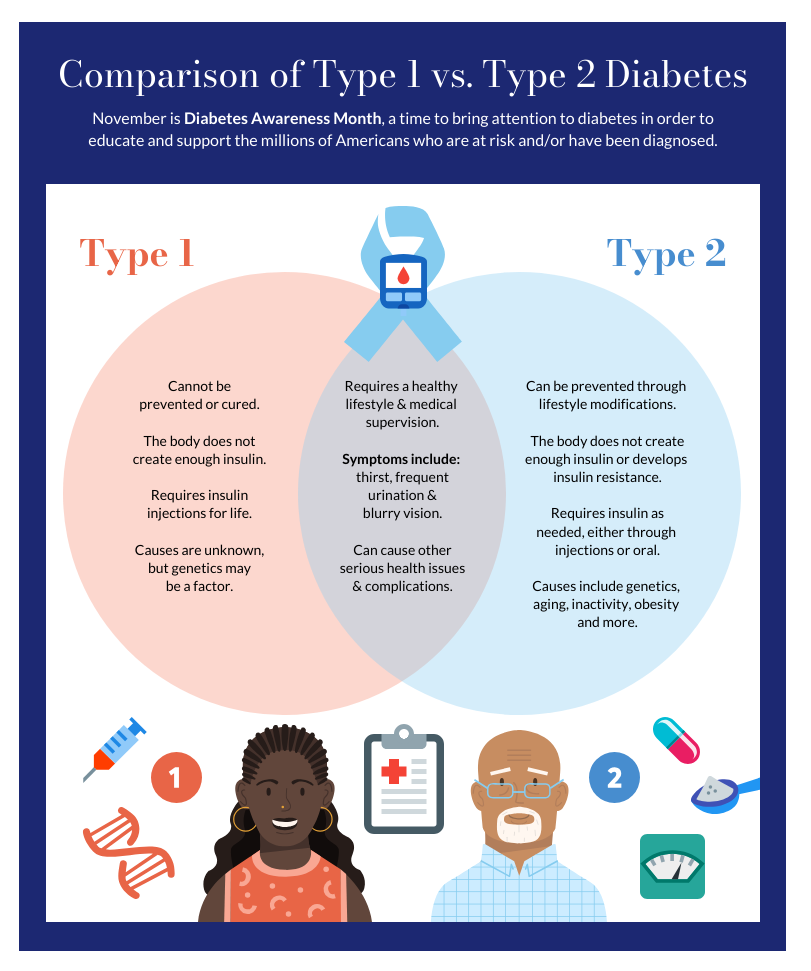
Type 1 diabetes
What is type 1 diabetes?
Learn more about type 1 diabetes.
Type 1 diabetes, once known as juvenile diabetes or insulin-dependent diabetes, is a chronic condition. In this condition, the pancreas makes little or no insulin. Insulin is a hormone the body uses to allow sugar (glucose) to enter cells to produce energy.
Different factors, such as genetics and some viruses, may cause type 1 diabetes. Although type 1 diabetes usually appears during childhood or adolescence, it can develop in adults.
Even after a lot of research, type 1 diabetes has no cure. Treatment is directed toward managing the amount of sugar in the blood using insulin, diet and lifestyle to prevent complications.
Symptoms
Type 1 diabetes symptoms can appear suddenly and may include:
- Feeling more thirsty than usual
- Urinating a lot
- Bed-wetting in children who have never wet the bed during the night
- Feeling very hungry
- Losing weight without trying
- Feeling irritable or having other mood changes
- Feeling tired and weak
- Having blurry vision
When to see a doctor
Talk to your health care provider if you notice any of the above symptoms in you or your child.
Causes
The exact cause of type 1 diabetes is unknown. Usually, the body’s own immune system — which normally fights harmful bacteria and viruses — destroys the insulin-producing (islet) cells in the pancreas. Other possible causes include:
- Genetics
- Exposure to viruses and other environmental factors
The role of insulin
Once a large number of islet cells are destroyed, the body will produce little or no insulin. Insulin is a hormone that comes from a gland behind and below the stomach (pancreas).
- The pancreas puts insulin into the bloodstream.
- Insulin travels through the body, allowing sugar to enter the cells.
- Insulin lowers the amount of sugar in the bloodstream.
- As the blood sugar level drops, the pancreas puts less insulin into the bloodstream.
The role of glucose
Glucose — a sugar — is a main source of energy for the cells that make up muscles and other tissues.
- Glucose comes from two major sources: food and the liver.
- Sugar is absorbed into the bloodstream, where it enters cells with the help of insulin.
- The liver stores glucose in the form of glycogen.
- When glucose levels are low, such as when you haven’t eaten in a while, the liver breaks down the stored glycogen into glucose. This keeps glucose levels within a typical range.
In type 1 diabetes, there’s no insulin to let glucose into the cells. Because of this, sugar builds up in the bloodstream. This can cause life-threatening complications.
Risk factors
Some factors that can raise your risk for type 1 diabetes include:
- Family history. Anyone with a parent or sibling with type 1 diabetes has a slightly higher risk of developing the condition.
- Genetics. Having certain genes increases the risk of developing type 1 diabetes.
- Geography. The number of people who have type 1 diabetes tends to be higher as you travel away from the equator.
- Age. Type 1 diabetes can appear at any age, but it appears at two noticeable peaks. The first peak occurs in children between 4 and 7 years old. The second is in children between 10 and 14 years old.
Complications
Over time, type 1 diabetes complications can affect major organs in the body. These organs include the heart, blood vessels, nerves, eyes and kidneys. Having a normal blood sugar level can lower the risk of many complications.
Diabetes complications can lead to disabilities or even threaten your life.
- Heart and blood vessel disease. Diabetes increases the risk of some problems with the heart and blood vessels. These include coronary artery disease with chest pain (angina), heart attack, stroke, narrowing of the arteries (atherosclerosis) and high blood pressure.
-
Nerve damage (neuropathy). Too much sugar in the blood can injure the walls of the tiny blood vessels (capillaries) that feed the nerves. This is especially true in the legs. This can cause tingling, numbness, burning or pain. This usually begins at the tips of the toes or fingers and spreads upward. Poorly controlled blood sugar could cause you to lose all sense of feeling in the affected limbs over time.
Damage to the nerves that affect the digestive system can cause problems with nausea, vomiting, diarrhea or constipation. For men, erectile dysfunction may be an issue.
- Kidney damage (nephropathy). The kidneys have millions of tiny blood vessels that keep waste from entering the blood. Diabetes can damage this system. Severe damage can lead to kidney failure or end-stage kidney disease that can’t be reversed. End-stage kidney disease needs to be treated with mechanical filtering of the kidneys (dialysis) or a kidney transplant.
- Eye damage. Diabetes can damage the blood vessels in the retina (part of the eye that senses light) (diabetic retinopathy). This could cause blindness. Diabetes also increases the risk of other serious vision conditions, such as cataracts and glaucoma.
- Foot damage. Nerve damage in the feet or poor blood flow to the feet increases the risk of some foot complications. Left untreated, cuts and blisters can become serious infections. These infections may need to be treated with toe, foot or leg removal (amputation).
- Skin and mouth conditions. Diabetes may leave you more prone to infections of the skin and mouth. These include bacterial and fungal infections. Gum disease and dry mouth also are more likely.
- Pregnancy complications. High blood sugar levels can be dangerous for both the parent and the baby. The risk of miscarriage, stillbirth and birth defects increases when diabetes isn’t well-controlled. For the parent, diabetes increases the risk of diabetic ketoacidosis, diabetic eye problems (retinopathy), pregnancy-induced high blood pressure and preeclampsia.
Prevention
There’s no known way to prevent type 1 diabetes. But researchers are working on preventing the disease or further damage of the islet cells in people who are newly diagnosed.
Ask your provider if you might be eligible for one of these clinical trials. It is important to carefully weigh the risks and benefits of any treatment available in a trial.
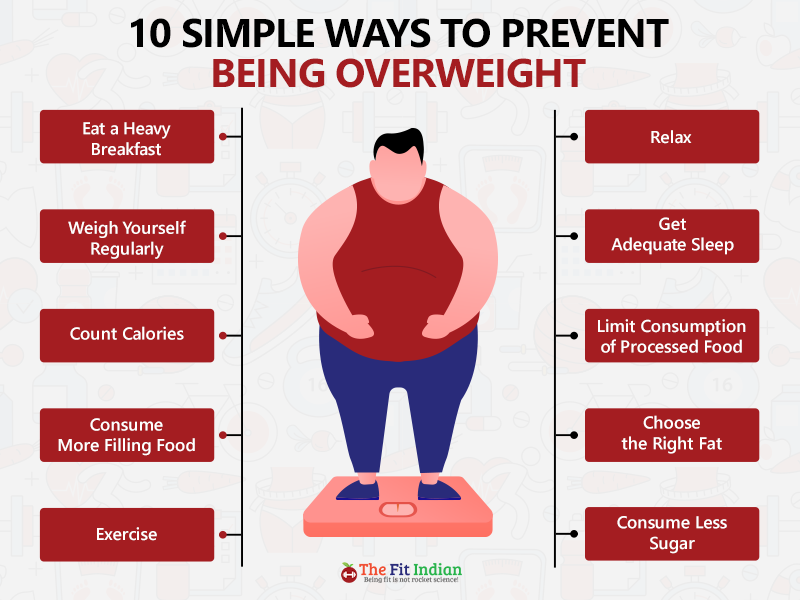
What is Obesity? How to prevent Obesity?
Obesity is a medical condition characterized by an excess amount of body fat, which presents a risk to health. It is typically defined and measured by the Body Mass Index (BMI), which is a calculation based on height and weight. A BMI of 30 or higher is considered obese. Obesity increases the likelihood of developing various health issues, such as heart disease, type 2 diabetes, stroke, certain types of cancer, and osteoarthritis. It’s caused by a combination of factors, including genetics, dietary habits, physical activity levels, and environmental and psychological factors. Managing and preventing obesity involves a holistic approach, including dietary changes, increased physical activity, and sometimes medical intervention.
Preventing obesity involves a multifaceted approach focusing on diet, physical activity, and behavioral changes. Here are some key strategies:
1. **Healthy Eating Habits:**
– **Eat Balanced Meals:** Focus on a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
– **Control Portions:** Pay attention to portion sizes to avoid consuming too many calories.
– **Limit Sugar and Processed Foods:** Reduce intake of foods high in added sugars and processed foods that are high in calories and low in nutrients.
2. **Regular Physical Activity:**
– **Stay Active:** Aim for at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity each week, along with muscle-strengthening exercises on two or more days a week.
– **Incorporate Activity into Daily Life:** Take the stairs, walk or bike instead of driving, and stand up regularly if you have a sedentary job.
3. **Behavioral Changes:**
– **Mindful Eating:** Pay attention to what and when you eat. Try to eat slowly and only when you’re actually hungry.
– **Sleep Well:** Ensure adequate sleep as lack of sleep can affect hormones that regulate hunger and appetite.
– **Stress Management:** Find healthy ways to manage stress, such as through exercise, meditation, or hobbies, rather than eating.
4. **Preventive Healthcare:**
– **Regular Check-ups:** Regular visits to a healthcare provider can help monitor your health status and prevent the onset of obesity-related conditions.
– **Health Education:** Understanding the risks of obesity and being informed about healthy lifestyles can empower individuals to make healthier choices.
5. **Community and Environment:**
– **Supportive Environments:** Advocate for environments that support healthy living, such as safe parks for physical activity and access to healthy foods.
– **Policy and Public Health Initiatives:** Support policies that promote nutritional education, physical activity, and equitable access to healthy food options.
Combating obesity is not just about individual actions; it also requires support from communities and policymakers to create environments that facilitate healthy choices and lifestyles.
Heart Disease
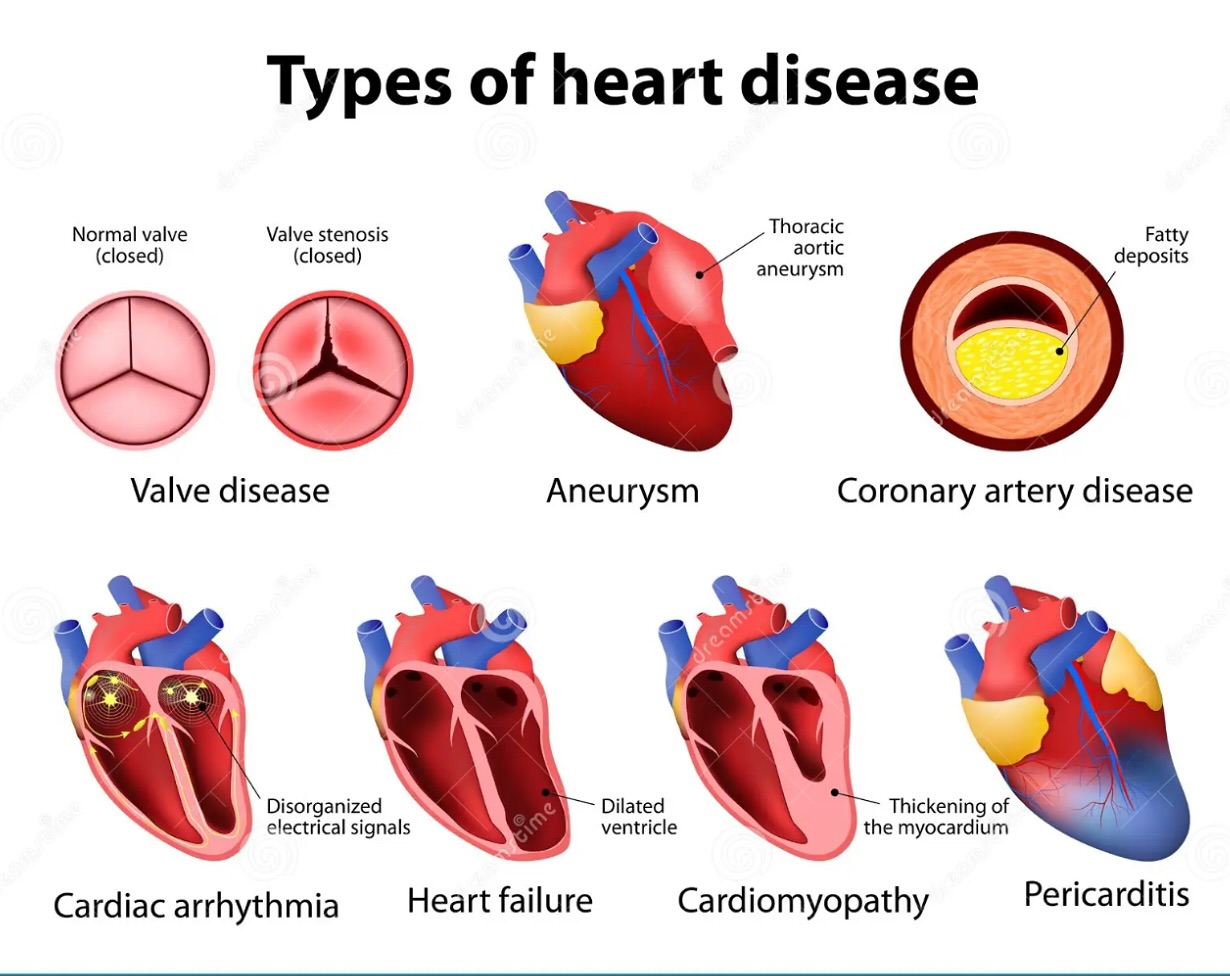
Heart disease refers to a range of conditions that affect the heart’s structure and function. These conditions include coronary artery disease, arrhythmias (heart rhythm problems), heart valve disease, heart infections, and congenital heart defects (heart problems present at birth). Below are key points about heart disease:
### Types of Heart Disease
1. **Coronary Artery Disease (CAD):** The most common type, caused by the buildup of plaque in the heart’s arteries, which can lead to heart attacks.
2. **Arrhythmias:** Abnormal heart rhythms that can cause the heart to beat too fast, too slow, or irregularly.
3. **Heart Failure:** A condition in which the heart can’t pump blood effectively to meet the body’s needs.
4. **Valvular Heart Disease:** Involves dysfunction of one or more of the heart valves that regulate blood flow through the heart.
5. **Congenital Heart Defects:** Heart abnormalities present at birth.
6. **Cardiomyopathies:** Diseases of the heart muscle that make it harder for the heart to pump blood to the body.
### Causes and Risk Factors
– **Lifestyle Factors:** Poor diet, lack of exercise, smoking, and excessive alcohol consumption.
– **Medical Conditions:** High blood pressure, high cholesterol, diabetes, obesity, and chronic kidney disease.
– **Genetics:** Family history of heart disease.
– **Age:** The risk increases with age.
– **Sex:** Men are generally at higher risk at a younger age, but the risk for women increases and can surpass that of men after menopause.
### Symptoms
Symptoms vary depending on the type of heart disease but may include chest pain, shortness of breath, palpitations, lightheadedness, dizziness, fainting, and swelling in the legs (edema).
### Prevention and Treatment
Prevention focuses on lifestyle changes such as maintaining a healthy diet, regular exercise, quitting smoking, controlling blood pressure, cholesterol, and diabetes, and managing stress. Treatment options depend on the type and severity of heart disease and can range from lifestyle changes and medications to invasive procedures like angioplasty or surgery, including heart bypass or valve repair/replacement.
### Importance of Regular Check-ups
Regular medical check-ups can help detect heart disease early. Health professionals can recommend preventive measures and treatments to manage risk factors effectively.
Heart disease remains a leading cause of death globally, but many forms of heart disease can be prevented or treated with healthy lifestyle choices and medical interventions.