What is ADHD?
ADHD is one of the most common neurodevelopmental disorders of childhood. It is usually first diagnosed in childhood and often lasts into adulthood. Children with ADHD may have trouble paying attention, controlling impulsive behaviors (may act without thinking about what the result will be), or be overly active.
Signs and Symptoms
It is normal for children to have trouble focusing and behaving at one time or another. However, children with ADHD do not just grow out of these behaviors. The symptoms continue, can be severe, and can cause difficulty at school, at home, or with friends.
A child with ADHD might:
- daydream a lot
- forget or lose things a lot
- squirm or fidget
- talk too much
- make careless mistakes or take unnecessary risks
- have a hard time resisting temptation
- have trouble taking turns
- have difficulty getting along with others
Types
There are three different ways ADHD presents itself, depending on which types of symptoms are strongest in the individual:
- Predominantly Inattentive Presentation: It is hard for the individual to organize or finish a task, to pay attention to details, or to follow instructions or conversations. The person is easily distracted or forgets details of daily routines.
- Predominantly Hyperactive-Impulsive Presentation: The person fidgets and talks a lot. It is hard to sit still for long (e.g., for a meal or while doing homework). Smaller children may run, jump or climb constantly. The individual feels restless and has trouble with impulsivity. Someone who is impulsive may interrupt others a lot, grab things from people, or speak at inappropriate times. It is hard for the person to wait their turn or listen to directions. A person with impulsiveness may have more accidents and injuries than others.
- Combined Presentation: Symptoms of the above two types are equally present in the person.
Because symptoms can change over time, the presentation may change over time as well.
Causes of ADHD
Scientists are studying cause(s) and risk factors in an effort to find better ways to manage and reduce the chances of a person having ADHD. The cause(s) and risk factors for ADHD are unknown, but current research shows that genetics plays an important role. Recent studies link genetic factors with ADHD.1
In addition to genetics, scientists are studying other possible causes and risk factors including:
- Brain injury
- Exposure to environmental risks (e.g., lead) during pregnancy or at a young age
- Alcohol and tobacco use during pregnancy
- Premature delivery
- Low birth weight
Research does not support the popularly held views that ADHD is caused by eating too much sugar, watching too much television, parenting, or social and environmental factors such as poverty or family chaos. Of course, many things, including these, might make symptoms worse, especially in certain people. But the evidence is not strong enough to conclude that they are the main causes of ADHD.
Diagnosis
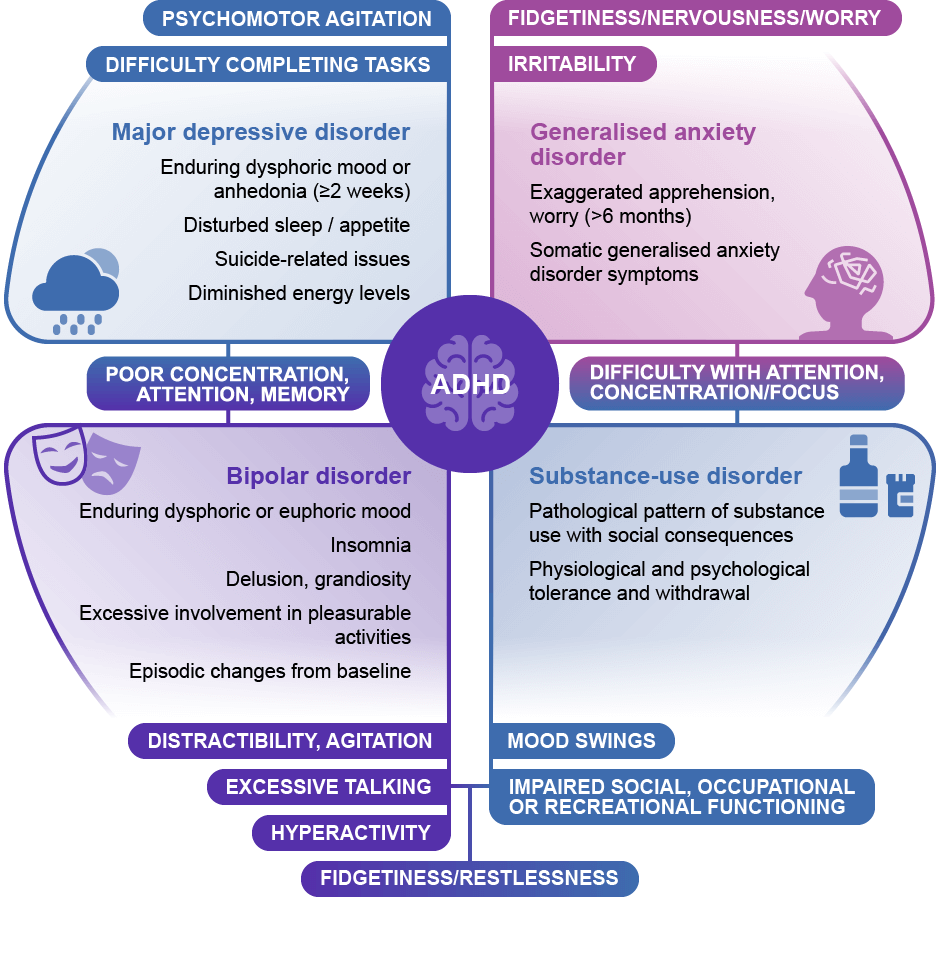
Deciding if a child has ADHD is a process with several steps. There is no single test to diagnose ADHD, and many other problems, like anxiety, depression, sleep problems, and certain types of learning disabilities, can have similar symptoms. One step of the process involves having a medical exam, including hearing and vision tests, to rule out other problems with symptoms like ADHD. Diagnosing ADHD usually includes a checklist for rating ADHD symptoms and taking a history of the child from parents, teachers, and sometimes, the child.
Treatments
In most cases, ADHD is best treated with a combination of behavior therapy and medication. For preschool-aged children (4-5 years of age) with ADHD, behavior therapy, particularly training for parents, is recommended as the first line of treatment before medication is tried. What works best can depend on the child and family. Good treatment plans will include close monitoring, follow-ups, and making changes, if needed, along the way.
Managing Symptoms: Staying Healthy
Being healthy is important for all children and can be especially important for children with ADHD. In addition to behavioral therapy and medication, having a healthy lifestyle can make it easier for your child to deal with ADHD symptoms. Here are some healthy behaviors that may help:
- Developing healthy eating habits such as eating plenty of fruits, vegetables, and whole grains and choosing lean protein sources
- Participating in daily physical activity based on age
- Limiting the amount of daily screen time from TVs, computers, phones, and other electronics
- Getting the recommended amount of sleep each night based on age
Get Help!
If you or your doctor has concerns about ADHD, you can take your child to a specialist such as a child psychologist, child psychiatrist, or developmental pediatrician, or you can contact your local early intervention agency (for children under 3) or public school (for children 3 and older).
The Centers for Disease Control and Prevention (CDC) funds the National Resource Center on ADHD, a program of CHADD – Children and Adults with Attention-Deficit/Hyperactivity Disorder. Their website has links to information for people with ADHD and their families. The National Resource Center operates a call center (1-866-200-8098) with trained staff to answer questions about ADHD.
For more information on services for children with special needs, visit the Center for Parent Information and Resources. To find the Parent Center near you, you can visit this website.
ADHD in Adults
ADHD can last into adulthood. Some adults have ADHD but have never been diagnosed. The symptoms can cause difficulty at work, at home, or with relationships. Symptoms may look different at older ages, for example, hyperactivity may appear as extreme restlessness. Symptoms can become more severe when the demands of adulthood increase. For more information about diagnosis and treatment throughout the lifespan, please visit the websites of the National Resource Center on ADHD and the National Institutes of Mental Health.
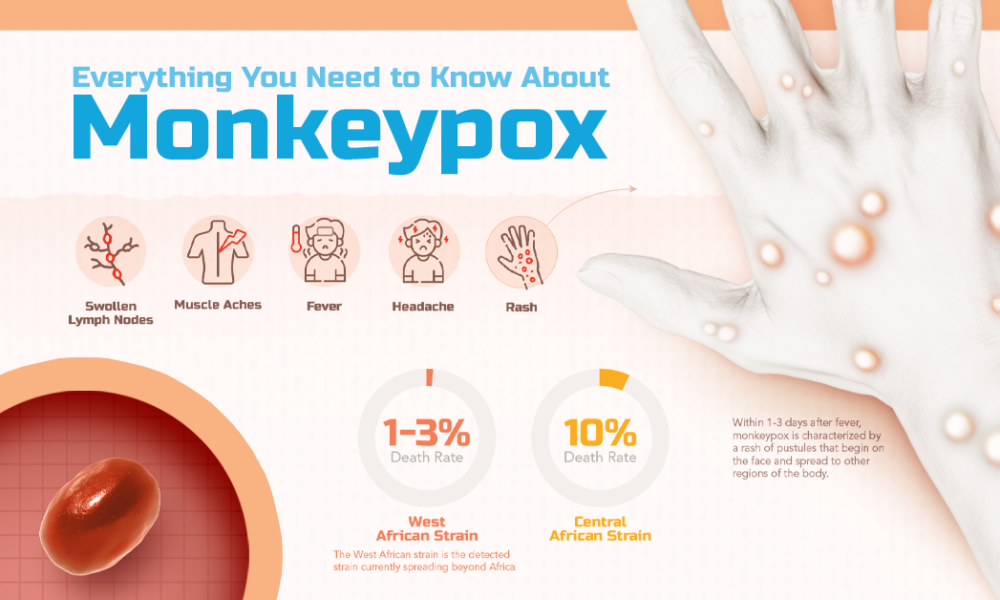
Monkeypox symptoms
People with monkeypox get a rash that may be located on or near the genitals (penis, testicles, labia, and vagina) or anus (butthole) and could be on other areas like the hands, feet, chest, face, or mouth.
- The rash will go through several stages, including scabs, before healing.
- The rash can initially look like pimples or blisters and may be painful or itchy.
Other symptoms of monkeypox can include:
- Fever
- Chills
- Swollen lymph nodes
- Exhaustion
- Muscle aches and backache
- Headache
- Respiratory symptoms (e.g. sore throat, nasal congestion, or cough)
You may experience all or only a few symptoms
- Sometimes, people have flu-like symptoms before the rash.
- Some people get a rash first, followed by other symptoms.
- Others only experience a rash.
How long do monkeypox symptoms last?
Monkeypox symptoms usually start within 3 weeks of exposure to the virus. If someone has flu-like symptoms, they will usually develop a rash 1-4 days later.
Monkeypox can be spread from the time symptoms start until the rash has healed, all scabs have fallen off, and a fresh layer of skin has formed. The illness typically lasts 2-4 weeks.
Avoid close contact, including sex or being intimate with anyone, until you have been checked out by a healthcare provider.
If you don’t have a provider or health insurance, visit a public health clinic near you.
When you see a healthcare provider, wear a mask, and remind them that this virus is circulating in the area.
What to Do If You Are Sick
There is no treatment specifically for monkeypox. Because the viruses that cause monkeypox and smallpox are closely related, drugs and vaccines developed to treat and protect against smallpox may be effective for monkeypox.
However, the type of treatment for a person with monkeypox will depend on how sick someone gets or whether they’re likely to get severely ill. Most people with monkeypox recover fully within 2 to 4 weeks without the need for medical treatment.
Some people, like those with a weakened immune system or genital or rectal rashes, may need treatment. Drugs used to treat monkeypox require a prescription and must be requested by a healthcare provider through the local or state health department.
Taking Care of Yourself
- Use gauze or bandages to cover the rash to limit spread to others and to the environment.
- Don’t lance (pop) or scratch lesions from the rash. This does not speed up recovery and can spread the virus to other parts of the body, increase the chance of spreading the virus to others, and possibly cause the open lesions to become infected by bacteria.
- Do not shave the area with the rash until the scabs have fallen off and a new layer of skin has formed. Shaving can spread the virus and cause more lesions.
- Keep skin lesions/rash clean and dry when not showering or bathing.
- Wash hands often with soap and water or use an alcohol-based hand sanitizer, especially after direct contact with the rash.
- If you have rash on your hands, be careful when washing or using sanitizer so as not to irritate the rash.
- If you have rash on your hands, wear gloves that are non-irritating when handling common objects or touching surfaces in shared spaces. If you can, use disposable gloves that can be discarded after each use (e.g., latex, polyurethane, or nitrile gloves). Reusable gloves should be washed with soap and water between use.
- Wear a well-fitting mask around other people until the rash and all other symptoms have resolved.
- Eat healthy and get plenty of rest to allow your body to heal.
Managing Your Symptoms
Medicines like ibuprofen (Advil, Motrin) and acetaminophen (Tylenol) can help you feel better. Your healthcare provider may prescribe stronger pain relievers as well.
For rash in the mouth, rinse with salt water at least four times a day. Prescription mouthwashes, sometimes called miracle or magic mouthwash, or local anesthetics like viscous lidocaine can be used to manage pain. Oral antiseptics like chlorhexidine mouthwash can be used to help keep the mouth clean.
Contact your healthcare provider if pain becomes severe and unmanageable at home.
Rash Relief
The most important thing is to try to not touch or scratch the rash. This can spread the rash to other parts of the body, increase the chance of spreading the virus to others, and possibly cause open lesions to become infected by bacteria. If you do accidentally touch the rash, wash your hands with soap and water and avoid touching sensitive areas like your eyes, nose, mouth, genitals and rectum (butthole).
Topical benzocaine/lidocaine gels can be used for temporary relief. Oral antihistamines such as Benadryl and topical creams such as calamine lotion or petroleum jelly may help with itching.
Soaking in a warm bath (using oatmeal or other over-the-counter bath products for itchy skin) may offer some relief to the dry, itchy sensations that can come with the rash.
People who have the rash in or around their anus (butthole) or genitals (penis, testicles, labia, vagina), or perineum (taint) may also benefit from a sitz-bath. A sitz bath is a round, shallow basin that can be purchased online or at a pharmacy. Most fit over the rim of a toilet but can also be placed in a bathtub. There is also the option to sit in a bathtub with shallow water. Your healthcare provider may prescribe medication like povidone-iodine or other products to be added to the water in a sitz bath. Adding Epsom salt, vinegar, or baking soda to the water can be soothing.
Healthy Weight
You may not get down to the number you saw on the scale 20 years ago, but you can still get to a weight that enhances your health and your life.
First, what does “healthy weight” mean to you? Is it the weight you think you should be? The same as you weighed 20 years ago? Ten pounds less than your sister-in-law? We can’t provide an exact number for you personally, but we can give you some pointers on how to get to a weight that’s healthy for you and stay there.
Two ways to get a ballpark idea if your weight is healthy or not: body mass index (BMI) and waist circumference.
BMI measures your height compared to your weight. For example, a person who is 5’7” and weighs 170 pounds has a BMI of 26.6, which is in the overweight range:
But experts note that BMI doesn’t measure belly fat, and that’s important. Too much belly fat can increase your risk for type 2 diabetes, heart disease, and stroke. Waist circumference (waist size) takes belly fat into account and helps predict your risk of health problems from being overweight. Women whose waist measures more than 35 inches and men whose waist measures more than 40 inches are at higher risk. Losing weight can reduce belly fat and lower that risk!
To measure your waist correctly, stand and place a tape measure around your middle, just above your hipbones. Measure your waist just after you breathe out.
Read about these three people who were able to shed the pounds (and keep them off).
Getting Started
Losing weight doesn’t have to mean losing a lot of weight. Taking off just 5% to 10%—that’s 10 to 20 pounds for a 200-pound person—can improve your health and well-being. If you have diabetes, you may find your blood sugar levels are easier to manage and that you need less diabetes medicine after you lose weight. Many people who lose weight notice that they have more energy and sleep better too.
A healthy weight goal is one thing; dropping the pounds is quite another. If there were an easy way to lose weight and keep it off, everyone would be doing it. We’ve all known someone who follows a popular diet plan and loses weight fast but then gains it all back (and then some). After trying and failing over and over, it’s easy to see why people give up.
Food for Life
Instead, create an eating plan that you can follow for life. It just needs two key ingredients:
- It’s based on healthy food.
- You can keep doing it long term.
With that in mind, you may need to try different things to figure out what works best for you day to day. Some people cut back on sugar and eat more protein to stay fuller longer. Others focus on filling up with extra fruits and vegetables, which leaves less room for unhealthy food. Still others limit variety for most meals and stick with choices that they know are healthy and filling. The details will depend on what you like and what fits in best with your life. If you need ideas and support, talk to a registered dietitian or diabetes educator (your doctor can give you a referral).
Physical Activity
Physical activity can make you feel better, function better, and sleep better. You’re not likely to lose a lot of weight with physical activity alone, but combining it with your diet strategy can improve weight loss. Here are the basic guidelines:
- Every week: do at least 150 minutes of moderate physical activity, such as brisk walking, or 75 minutes of vigorous activity, such as jogging, or an equivalent combination of the two.
- Two or more days a week: do strength-training activities, such as lifting weights or using a resistance band, that involve all major muscle groups.
If you have diabetes, physical activity can help you manage the condition along with your weight. Being active makes you more sensitive to insulin (the hormone that allows cells in your body to use blood sugar for energy). Your body won’t need to make as much insulin or you won’t need to take as much. Lower insulin levels can help prevent fat storage and weight gain. Learn more about being active when you have diabetes here.
While how you lose weight will be highly personalized, these pointers have helped others reach their goal and could help you, too.
Willpower Isn’t Enough
Don’t get us wrong: willpower is great. It just isn’t enough. You can’t count on it to reach and maintain the healthier weight you want.
But don’t worry; there are other ways. Control your environment so temptation is out of the picture and healthy habits are in. Some ideas:
- Don’t bring home food you don’t want to eat. Make home a safe zone!
- Avoid buffet-style restaurants.
- Don’t let yourself get too hungry.
- Cook your own food so you can control the calories.
- Lay out your workout clothes before you go to sleep.
- Keep the dog’s leash and your walking shoes by the door.
Sleep Helps
Too little sleep makes dieting much harder because it increases your hunger and appetite, especially for high-calorie, high-carb foods. Too little sleep also triggers stress hormones, which tell your body to hang onto fat. Outsmart this problem by being physically active, which has been shown to help you fall asleep faster and sleep better. A relaxing nighttime routine can also help you get your zzz’s. And these tips are tried and true: no screens an hour before bedtime, avoid heavy meals and alcohol before bedtime, and keep your bedroom dark and cool.
Balancing Food and Activity
Try this interactive Body Weight Planner to calculate calories and activity needed to get to your goal weight and maintain it.
Write It When You Bite It
Writing down what you eat is the single best predictor of weight loss success. But most people don’t do it because they think it will be too time-consuming. Guess how long it takes (yes, studies have been done)? Less than 15 minutes a day on average. You don’t need to add lots of detail, but aim for at least 3 entries each day and do it consistently day after day for the best results. Use this handy food diary [PDF – 105 KB] to get started.
Find Your Motivation
People who keep the weight off tend to be motivated by more than just being thinner. For some, it might be a health scare. Others want more energy to play with their grandkids. Focus on a goal that’s meaningful to you, and you’ll be more likely to keep the pounds off too.
More Tips
- Eat higher-protein, lower-carb meals to control hunger and appetite. For people with diabetes who take insulin, eating fewer carbs like bread, pasta, rice, desserts, sugary beverages, and juice can lower how much insulin they need. Using less insulin can help prevent hunger, fat storage, and weight gain.
- Choose carbs that are higher in fiber and lower in added sugar. For example, say yes to beans and sweet potatoes; say no to sugary drinks and chips.
- Drink more water and fewer sweetened beverages. This one change can cut lots of calories and mean fewer blood sugar swings!
- Keep moving. Physical activity helps you stay motivated and keep the weight off.
- Learn from a bad day. Everyone slips up from time to time; figure out what went wrong and plan for it next time. You’re only human, and humans are great learners.
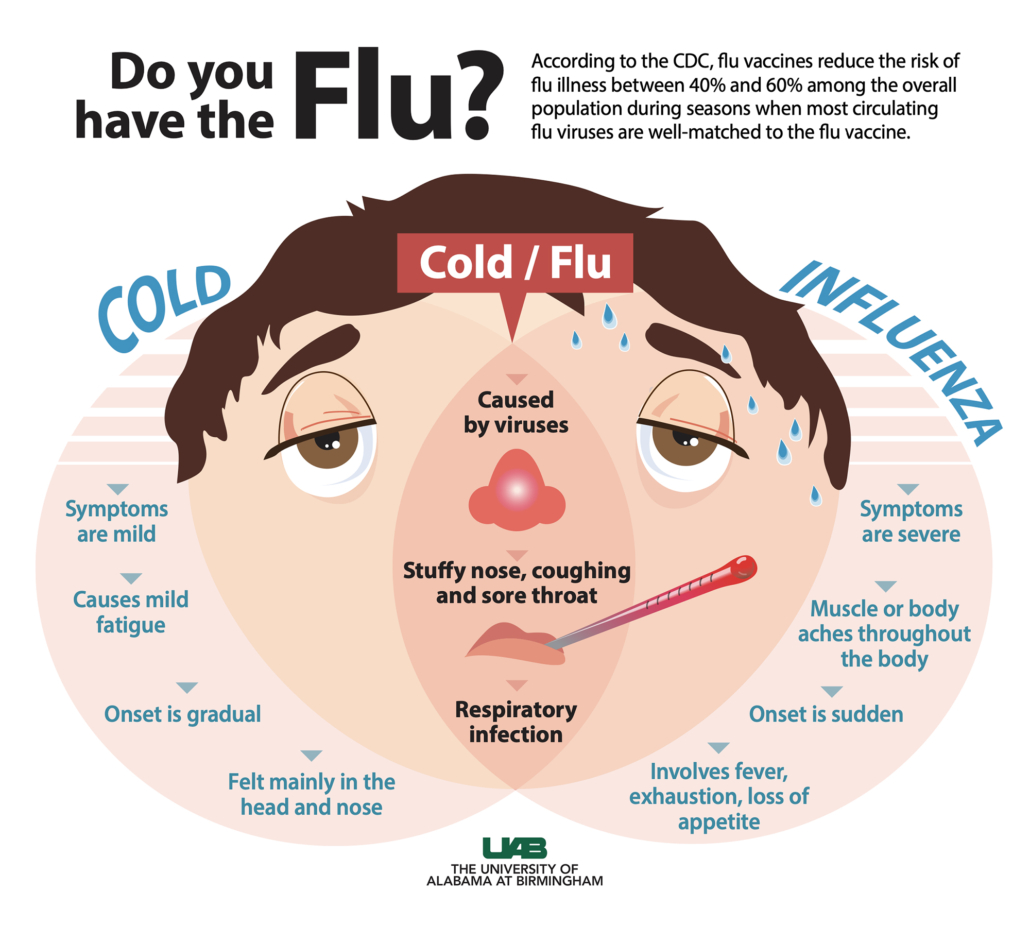
About Flu
Influenza (flu) is a contagious respiratory illness caused by influenza viruses that infect the nose, throat, and lungs. Some people, such as older people, young children, and people with certain health conditions, are at higher risk of serious flu complications. There are two main types of influenza (flu) viruses: Types A and B. The influenza A and B viruses that routinely spread in people (human influenza viruses) are responsible for seasonal flu epidemics each year.
The best way to reduce the risk of flu and its potentially serious complications is by getting vaccinated each year.
Preventive Steps
Take time to get a flu vaccine.
- CDC recommends a yearly flu vaccine as the first and most important step in protecting against flu viruses.
- Flu vaccines help to reduce the burden of flu illnesses, hospitalizations and deaths on the health care system each year. (Read more about flu vaccine benefits.)
- This season, all flu vaccines will be designed to protect against the four flu viruses that research indicates will be most common. (Visit Vaccine Virus Selection for this season’s vaccine composition.)
- Everyone 6 months and older should get an annual flu vaccine, ideally by the end of October. Learn more about vaccine timing.
- Vaccination of people at higher risk of developing serious flu complications is especially important to decrease their risk of severe flu illness.
- People at higher risk of serious flu complications include young children, pregnant people, people with certain chronic health conditions like asthma, diabetes or heart and lung disease, and people 65 years and older.
- Vaccination also is important for health care workers, and other people who live with or care for people at higher risk to keep from spreading flu to them. This is especially true for people who work in long-term care facilities, which are home to many of the people most vulnerable to flu.
- Children younger than 6 months are at higher risk of serious flu illness but are too young to be vaccinated. People who care for infants should be vaccinated instead.
Take everyday preventive actions to stop the spread of germs.
- Take everyday preventive actions that are recommended to reduce the spread of flu.
- Avoid close contact with people who are sick.
- If you are sick, limit contact with others as much as possible to keep from infecting them.
- Cover coughs and sneezes.
- Cover your nose and mouth with a tissue when you cough or sneeze. Throw the tissue in the trash after you use it.
- Wash your hands often with soap and water. If soap and water are not available, use an alcohol-based hand rub.
- Avoid touching your eyes, nose, and mouth. Germs spread this way.
- Clean and disinfect surfaces and objects that may be contaminated with viruses that cause flu.
- For flu, CDC recommends that people stay home for at least 24 hours after their fever is gone except to get medical care or other necessities. Fever should be gone without the need to use a fever-reducing medicine. Note that the stay-at-home guidance for COVID-19 may be different. Learn about some of the similarities and differences between flu and COVID-19.
- In the context of the COVID-19 pandemic, local governments or public health departments may recommend additional precautions be taken in your community. Follow those instructions.
Take flu antiviral drugs if your doctor prescribes them.
- If you are sick with flu, antiviral drugs can be used to treat your illness.
- Antiviral drugs are different from antibiotics. They are prescription medicines (pills, liquid or an inhaled powder) and are not available over-the-counter.
- Antiviral drugs can make flu illness milder and shorten the time you are sick. They may also prevent serious flu complications. For people with higher risk factors [308 KB, 2 Pages], treatment with an antiviral drug can mean the difference between having a milder illness versus a very serious illness that could result in a hospital stay.
- Studies show that flu antiviral drugs work best for treatment when they are started within 2 days of getting sick, but starting them later can still be helpful, especially if the sick person has a higher risk factor or is very sick from flu.
- If you are at higher risk from flu and get flu symptoms, call your health care provider early so you can be treated with flu antivirals if needed. Follow your doctor’s instructions for taking this drug.
Flu symptoms include fever, cough, sore throat, runny or stuffy nose, body aches, headache, chills and fatigue. Some people also may have vomiting and diarrhea. People may be infected with flu and have respiratory symptoms without a fever. Visit CDC’s website to find out what to do if you get sick with flu. Learn about some of the similarities and differences between flu and COVID-19, and the difference between flu and the common cold.
Planning for Pregnancy
Pregnant? Don’t Smoke!
Smoking during pregnancy can cause babies to be born too small or too early (preterm birth), certain birth defects, and stillbirth. Quitting smoking can be hard, but it is one of the best ways a woman can protect herself and her developing baby. For free help, call 1-800-QUIT-NOW (1-800-784-8669).
Many people know that smoking causes cancer, heart disease, and stroke. But women who smoke during pregnancy put themselves and their developing babies at risk for other health problems. Even being around tobacco smoke puts a woman and her developing baby at risk for health problems.
Smoking during Pregnancy Affects Your Developing Baby’s Health
Smoking during pregnancy can cause babies to be born too small or too early. Women who smoke during pregnancy are more likely to have a baby with a birth defect of the mouth and lip called an orofacial cleft.
Babies who breathe in other people’s tobacco smoke are more likely to have ear infections and lung infections, like bronchitis and pneumonia; if they have asthma, breathing in other people’s tobacco smoke can trigger asthma attacks. These babies are also more likely to die from Sudden Infant Death Syndrome (SIDS), a sudden and unexpected infant death that has no immediately obvious cause after investigation.
It Is Never “Too Late” to Quit Smoking During Pregnancy!
Quitting smoking before getting pregnant is best. But for women who are already pregnant, quitting as early as possible can still help protect against some health problems for their developing babies, such as being born too small or too early. It is never too late to quit smoking.
It is important to quit smoking for good. A women might think it is safe to start smoking again after her baby is born. But babies of mothers who smoke may breathe in the secondhand tobacco smoke that can harm their health. Although quitting for good can be hard, the benefits are worth it—a healthy baby and many more years of good health to enjoy with him or her.
If you or someone you know wants to quit smoking, talk to your healthcare provider about strategies. For support in quitting, including free quit coaching, a free quit plan, free educational materials, and referrals to local resources, please call 1-800-QUIT-NOW (1-800-784-8669); TTY 1-800-332-8615.
Planning for Pregnancy
If you are trying to have a baby or are just thinking about it, it is not too early to start getting ready for pregnancy. Preconception health and health care focus on things you can do before and between pregnancies to increase the chances of having a healthy baby. For some women, getting their body ready for pregnancy takes a few months. For other women, it might take longer. Whether this is your first, second, or sixth baby, the following are important steps to help you get ready for the healthiest pregnancy possible.
1. Make a Plan and Take Action
Whether or not you’ve written them down, you’ve probably thought about your goals for having or not having children, and how to achieve those goals. For example, when you didn’t want to have a baby, you used effective birth control methods to achieve your goals. Now that you’re thinking about getting pregnant, it’s really important to take steps to achieve your goal [PDF – 764 KB]—getting pregnant and having a healthy baby!
2. See Your Doctor
Before getting pregnant, talk to your doctor about preconception health care. Your doctor will want to discuss your health history and any medical conditions you currently have that could affect a pregnancy. He or she also will discuss any previous pregnancy problems, medicines that you currently are taking, vaccinations that you might need, and steps you can take before pregnancy to prevent certain birth defects.
If your doctor has not talked with you about this type of care―ask about it! Take a list of talking points so you don’t forget anything!
Be sure to talk to your doctor about:
Medical Conditions
If you currently have any medical conditions, be sure they are under control and being treated. Some of these conditions include: sexually transmitted diseases (STDs), diabetes, thyroid disease, high blood pressure, and other chronic diseases.
Lifestyle and Behaviors
Talk with your doctor or another health professional if you smoke, drink alcohol, or use certain drugs; live in a stressful or abusive environment; or work with or live around toxic substances. Health care professionals can help you with counseling, treatment, and other support services.
Medications
Taking certain medicines during pregnancy can cause serious birth defects. These include some prescription and over-the-counter medications and dietary or herbal supplements. If you are planning a pregnancy, you should discuss the need for any medication with your doctor before becoming pregnant and make sure you are taking only those medications that are necessary.
People may use opioids as prescribed, may misuse prescription opioids, may use illicit opioids such as heroin, or may use opioids as part of medication-assisted treatment for opioid use disorder. If a woman is pregnant or planning to become pregnant, the first thing she should do is talk to a healthcare provider. Some women need to take an opioid medication during pregnancy to manage pain or to treat opioid use disorder. Creating a treatment plan for opioid use disorder, as well as other co-occurring health conditions, before pregnancy can help a woman increase her chances of a healthy pregnancy. If you are struggling with an opioid use disorder, take a look at CDC’s and partner resources.
Vaccinations (shots)
Some vaccinations are recommended before you become pregnant, during pregnancy, or right after delivery. Having the right vaccinations at the right time can help keep you healthy and help keep your baby from getting very sick or having lifelong health problems.
3. Take 400 Micrograms of Folic Acid Every Day
Folic acid is a B vitamin. If a woman has enough folic acid in her body at least 1 month before and during pregnancy, it can help prevent major birth defects of the baby’s brain and spine.
4. Stop Drinking Alcohol, Smoking, and Using Certain Drugs
Smoking, drinking alcohol, and using certain drugs can cause many problems during pregnancy for a woman and her baby, such as premature birth, birth defects, and infant death.
If you are trying to get pregnant and cannot stop drinking, smoking, or using drugs―get help! Contact your doctor or local treatment center.
Alcohol and Drug Resources
Substance Abuse Treatment Facility Locator
The Substance Abuse and Mental Health Services Administration (SAMHSA) has a treatment facility locator. This locator helps people find drug and alcohol treatment programs in their area.
Alcoholics Anonymous (A.A.)
Alcoholics Anonymous® is a fellowship of men and women who share their experiences, strengths, and hopes with each other so that they can solve their common problem and help others to recover from alcoholism. Locate an A.A. program near you.
Learn more about alcohol and pregnancy »
Smoking Resources
1-800-QUIT-NOW (1-800-784-8669)
Learn more about smoking during pregnancy »
5. Avoid Toxic Substances and Environmental Contaminants
Avoid harmful chemicals, environmental contaminants, and other toxic substances such as synthetic chemicals, metals, fertilizer, bug spray, and cat or rodent feces around the home and in the workplace. These substances can hurt the reproductive systems of men and women. They can make it more difficult to get pregnant. Exposure to even small amounts during pregnancy, infancy, childhood, or puberty can lead to diseases. Learn how to protect yourself and your loved ones from toxic substances at work and at home.
Learn about the effects of toxic substances on reproductive health »
Learn how CDC tracks Children’s Environmental Health »
6. Reach and Maintain a Healthy Weight
People who are overweight or obese have a higher risk for many serious conditions, including complications during pregnancy, heart disease, type 2 diabetes, and certain cancers (endometrial, breast, and colon).1 People who are underweight are also at risk for serious health problems.2
The key to achieving and maintaining a healthy weight isn’t about short-term dietary changes. It’s about a lifestyle that includes healthy eating and regular physical activity.
If you are underweight, overweight, or obese, talk with your doctor about ways to reach and maintain a healthy weight before you get pregnant.
Learn more about healthy weight »
7. Get Help for Violence
Violence can lead to injury and death among women at any stage of life, including during pregnancy. The number of violent deaths experienced by women tells only part of the story. Many more survive violence and are left with lifelong physical and emotional scars.
If someone is violent toward you or you are violent toward your loved ones―get help. Violence destroys relationships and families.
Learn about violence prevention »
8. Learn Your Family History
Collecting your family’s health history can be important for your child’s health. You might not realize that your sister’s heart defect or your cousin’s sickle cell disease could affect your child, but sharing this family history information with your doctor can be important.
Other reasons people go for genetic counseling include having had several miscarriages, infant deaths, trouble getting pregnant (infertility), or a genetic condition or birth defect that occurred during a previous pregnancy.
Learn more about family history »
Learn more about genetic counseling »
9. Get Mentally Healthy
Mental health is how we think, feel, and act as we cope with life. To be at your best, you need to feel good about your life and value yourself. Everyone feels worried, anxious, sad, or stressed sometimes. However, if these feelings do not go away and they interfere with your daily life, get help. Talk with your doctor or another health professional about your feelings and treatment options.
10. Have a Healthy Pregnancy!
Once you are pregnant, be sure to keep up all of your new healthy habits and see your doctor regularly throughout pregnancy for prenatal care.
Learn how to have a healthy pregnancy »
References
- NIH, NHLBI Obesity Education Initiative. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. Available online:
http://www.nhlbi.nih.gov/guidelines/obesity/ob_gdlns.pdf (PDF-1.25Mb) - Moos, Merry-K, et al. Healthier women, healthier reproductive outcomes: recommendations for the routine care of all women of reproductive age. AJOG Volume 199, Issue 6, Supplement B , Pages S280-S289, December 2008.
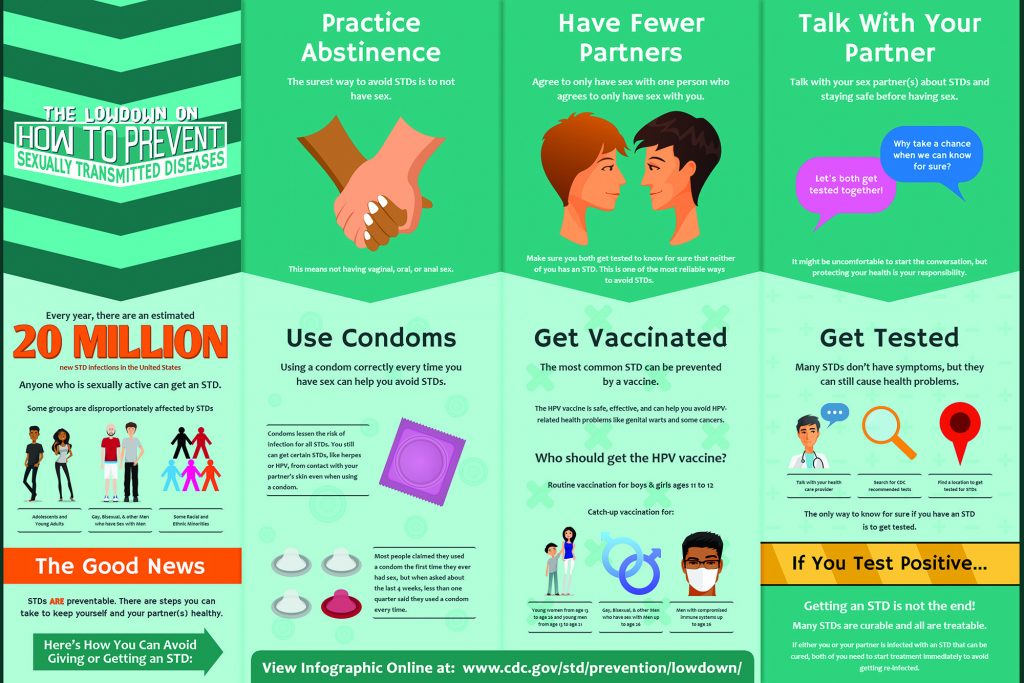
Sexually Transmitted Disease Surveillance, 2020 serves as a reminder that STDs remain a significant public health concern, even in the face of a pandemic. In 2020, COVID-19 significantly affected STD surveillance and prevention efforts. This report reflects the realities of a strained public health infrastructure, while simultaneously providing the most current data on reported cases of STDs in the United States. Trends presented in this report should be interpreted cautiously.
Chlamydia
In 2020, a total of 1,579,885 cases of Chlamydia trachomatis infection were reported to the CDC, making it the most common notifiable sexually transmitted infection in the United States for that year. This case count corresponds to a rate of 481.3 cases per 100,000 population, a decrease of 13% compared with the rate in 2019. During 2019–2020, rates of reported chlamydia decreased among both males and females, in all regions of the United States, and, except for rates among non-Hispanic persons of multiple races, among all racial/Hispanic ethnicity groups.
Decreases in rates of reported chlamydia in 2020 are unlikely due to a reduction in new infections. As chlamydial infections are usually asymptomatic, case rates are heavily influenced by screening coverage. During the COVID-19 pandemic, many health care clinics limited in-person visits to patients with symptoms or closed entirely, and it is likely that preventive health care visits where STD screening usually happens, such as annual reproductive health visits for young women, decreased. During the initial shelter-in-place orders in March and April of 2020, the number of chlamydia cases decreased substantially when compared to the number of cases reported in 2019 and the deficit persisted throughout the year.
Rates of reported chlamydia are highest among adolescents and young adults. In 2020, almost two-thirds (61%) of all reported chlamydia cases were among persons aged 15–24 years. Decreases in rates of diagnosed and reported chlamydia during 2020 were most noticeable among females aged 15–24 years, one of the populations targeted for chlamydia screening. Although still high, rates of reported chlamydia decreased 15% among 15–19-year-old females and decreased 10% among 20–24-year-old females during 2019–2020.