About Cholesterol
Blood cholesterol is a waxy, fat-like substance made by your liver. Blood cholesterol is essential for good health. Your body needs it to perform important jobs, such as making hormones and digesting fatty foods. Your body makes all the blood cholesterol it needs, which is why experts recommend that people eat as little dietary cholesterol as possible while on a healthy eating plan.
| OPTIMAL CHOLESTEROL LEVELS1 | |
|---|---|
| Total cholesterol | About 150 mg/dL |
| LDL (“bad”) cholesterol | About 100 mg/dL |
| HDL (“good”) cholesterol | At least 40 mg/dL in men and 50 mg/dL in women |
| Triglycerides | Less than 150 mg/dL |
What are signs and symptoms of high cholesterol?
High blood cholesterol doesn’t have symptoms, which is why getting your cholesterol levels checked is so important.
Knowing your cholesterol status can help you stay in control of your health.
What causes high cholesterol?
Certain health conditions, such as type 2 diabetes and obesity, can raise your risk for high cholesterol. Lifestyle factors, such eating a diet high in saturated and trans fats and not getting enough activity, can also raise your risk for high cholesterol. Some people who have a family history of high cholesterol can also be at risk for high cholesterol. All these factors are called “risk factors.”
You can’t control some of these risk factors, such as your age or your family history. But you can
What problems does high cholesterol cause?
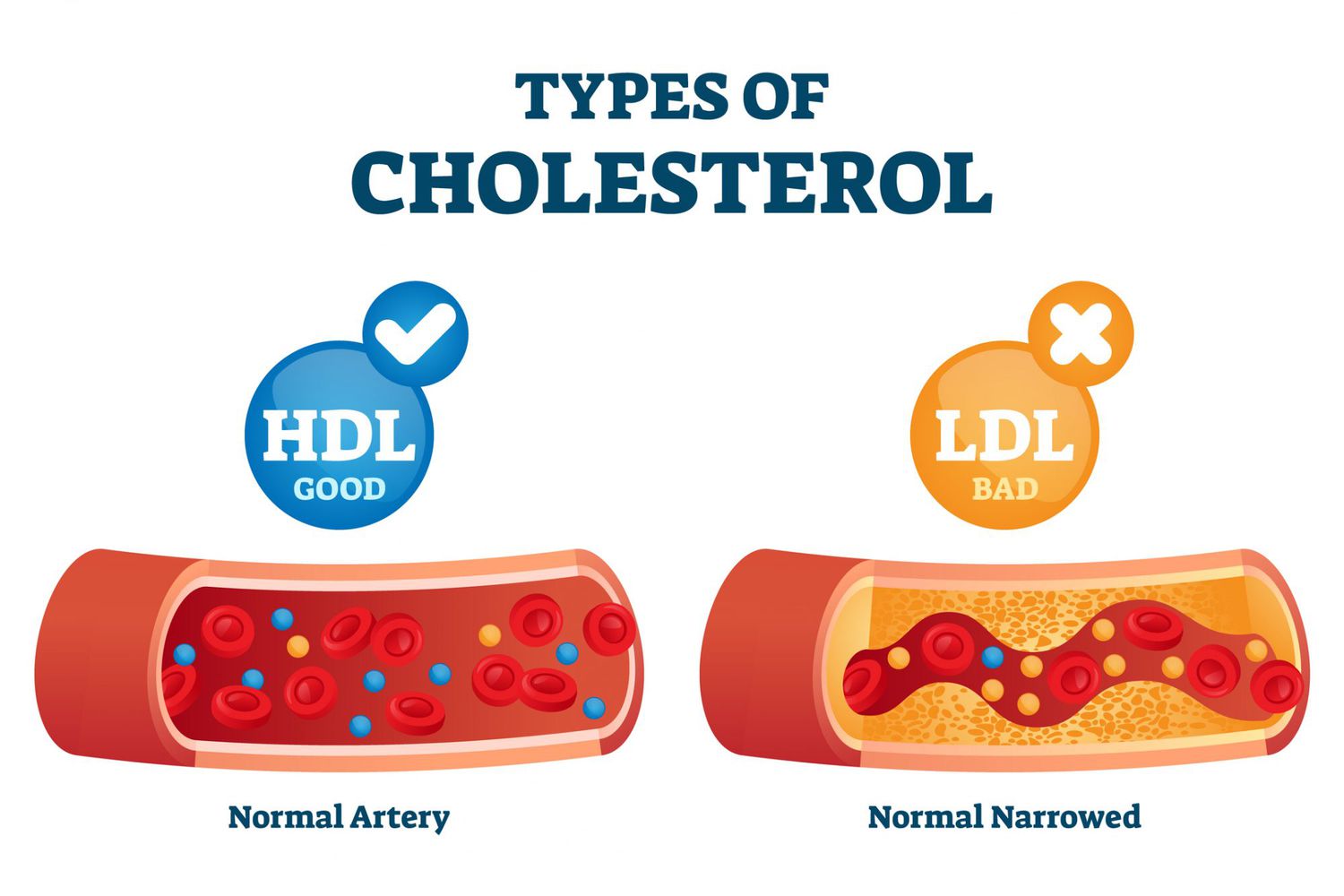
Having high blood cholesterol can lead to a buildup called “plaque” on the walls of your arteries (a type of blood vessel).
As plaque builds up over time, the insides of your arteries narrow. This narrowing blocks blood flow to and from your heart and other organs. When blood flow to the heart is blocked, it can cause chest pain (also called angina) or a heart attack (also called myocardial infarction).
High cholesterol also increases your risk for heart disease and stroke, two leading causes of death in the United States.
How do I know if I have high cholesterol?
The only way to know whether you have high cholesterol is to get your cholesterol checked by your health care team. Talk with your health care team about how often you should have your cholesterol screened.
What can I do to prevent or manage high cholesterol?
Strong evidence shows that eating patterns that include less dietary cholesterol are associated with reduced risk of cardiovascular disease.
Your overall risk for high cholesterol depends on many factors.
Walking 8,000 steps just 1-2 days a week linked to significant health benefits
A study found hitting the 8,000-step goal just one to two days per week is still associated with a significant reduction in all-cause and cardiovascular mortality. Third Eye Images/Getty Images
- Current research suggests that walking 8,000 brisk steps or more per day may be the sweet spot for receiving the health benefits walking provides.
- People who have trouble finding time to walk each day of the week will be encouraged by a new study that demonstrates walking just one to two days is still associated with a significant reduction in all-cause and cardiovascular mortality.
- The study’s authors found that each additional day walked confers greater benefits.
Briskly walking 8,000 or more steps each day of the week is associated with a significant decrease in all-cause and cardiovascular mortality. A new study finds, however, that people taking just 8,000 steps one or two days a week are also less likely to die over a 10-year follow-up period.
The study published in JAMA Network Open found that over a decade of follow-up, people 20 years or older who took 8,000 or more steps on one or two days a week were 14.9% less likely to die compared to people who were sedentary.
The risk of death dropped as the number of days involved increased. For example, exercising from three to seven days a week was associated with a 16.5% reduction in all-cause and cardiovascular deaths.
The same pattern held true for people meeting step goals of 6,000 to 10,000 steps.
Previous research found that mortality risk decreases up to 10,000 steps per day for people younger than 60 and 8,000 for people older than 60.
‘Weekend warrior’ style of exercising
The study’s findings pertain to both “weekend warriors,” people who confine their exercise to non-work days, and to people who steal a few hours to walk during the week.
The study cites recent data showing the average American takes just 4,800 steps a day, too few to provide much of a health benefit.
“Brisk walking” is defined as walking three miles an hour. If you can speak song lyrics but not sing them, you are walking briskly.
The current study compared data from the U.S. 2005 and 2006 National Health and Nutrition Examination Survey with the National Death Index up to the year 2019. It incorporated accelerometer data from 3,101 participants 20 years or older and was a nationally representative sample. It included a similar number of women and men, and 50.9% were White, 21.5% Black, 23.7% Hispanic, and 3.9% other race and ethnicity.
The participants most likely to walk 8,000 or more steps every day were more likely to be young, male, Hispanic, insured, and married. They were also typically never-smokers and were less likely to be obese or have comorbidities.
A daily challenge of walking 8,000 steps
For many people, walking 8,000 steps each day requires a significant commitment of time. 8,000 steps are about four miles, which, walking at three miles per hour, comes to a total of about an hour and 20 minutes every day. Steps can be taken simultaneously or in shorter periods of brisk walking.
The study was led by Dr. Kosuke Inoue of Kyoto University in Japan, collaborating with researchers from UCLA in California. Dr. Inoue explained why the study was undertaken:
“We started this study to answer the question one of my patients asked during an outpatient clinic: ‘It is hard for me to keep sufficient steps every day. Is it okay to focus on walking only during the weekend?’”
Steps studies often consider the value of a week’s worth of various step goals, and Dr. Inoue saw a lack of evidence regarding the possible benefits of walking just a few days a week.
“Given that a lack of time is one of the major barriers to exercise in modern society,” said Dr. Inoue, “our findings provide useful information to recommend walking even for a couple of days per week to reduce mortality risk.”
“This is one of the first studies to use direct measures of daily steps using a wearable accelerometer over a 10-year followup period,” said Dr. Paul Arciero, a professor in the Health and Human Physiological Sciences Department at Skidmore College, who was not involved in the study.
How walking benefits overall health
Walking is viewed as a simple, low impact means of making a person’s life less sedentary. A sedentary lifestyle has been linked to an increased risk of all-cause and cardiovascular mortality.
“Further, a sedentary lifestyle drastically increases the risk of cardiometabolic disease such as abdominal obesity, hypertension (high blood pressure), type 2 diabetes, stroke, heart disease, and certain inflammatory conditions and cancers,” said Dr. Arciero.
According to Harvard Medical School, taking one’s steps has additional, less-obvious benefits. Walking offsets the effect of weight-promoting genes, reduces breast cancer risk, and boosts one’s immune system. It can also lessen arthritis-based joint pain, and even a 15-minute walk can curb a craving for chocolate, both generally and in response to stress.
Dealing with limited time for walking
The study’s findings should provide valuable information for clinicians and health professionals, said Dr. Inoue. He suggested a reader’s takeaway should be that for people who have difficulties engaging in regular exercise, “achieving recommended daily steps only a couple of days per week can have meaningful health benefits.”
Describing the study’s conclusions as “encouraging,” Dr. Arciero suggested the study may help people who don’t have enough time to walk 8,000 steps a day overcome feelings that walking less is pointless.
“We now have scientific evidence that proves this mindset is not true, and even a couple of days is beneficial!” said Dr. Arciero.
He said the study underscores the value of increasing one’s daily step count:
“Always a good reminder that any amount of walking, even one to two days per week, is still better than no walking.”
Understanding and Recognizing Pre-Migraine Symptoms
Migraine is more than headaches. It’s a neurological condition that impacts more than 36 million Americans, according to the American Migraine Foundation. Migraine can cause severe pain and interrupt your daily activities.
Pre-migraine is one of the four stages of a migraine attack. Pre-migraine symptoms may occur before a migraine attack begins. You may be able to take steps to avoid a painful migraine attack if you can recognize the pre-migraine stage.
What are pre-migraine symptoms?
Migraine has four distinct states. Pre-migraine, called the prodrome stage, consists of a symptom or group of symptoms which let you know that a migraine attack is coming. It can begin anywhere from a few hours to several days before a migraine attack occurs.
The prodrome stage, sometimes also called the pre-headache or premonitory phase, doesn’t occur before every migraine attack, but learning to recognize pre-migraine symptoms can help you take preventative action. It’s also important to know that not everyone who has a prodrome stage will experience the exact same symptoms.
Pre-migraine symptoms may include:
- Mood changes. You might feel depressed, anxious, or irritable without a pinpointable cause.
- Muscle pain. Stiffness and cramping in your neck and shoulders is a common pre migraine symptom.
- Food cravings. You can have strong cravings, especially for sweet foods, before a migraine attack.
- Difficulty concentrating. You might have trouble focusing and feel foggy or confused.
- Fatigue. Even if you had a good night’s sleep, you can feel extra tired leading up to a migraine attack.
- Excessive yawning. Finding yourself yawning frequently throughout the day can be a migraine attack symptom.
- Digestion trouble. You might experience constipation or diarrhea before a migraine attack begins.
- Increased urinary frequency. Needing to visit the bathroom more often than normal is a common prodrome symptom.
- Sensitivity to light and sound. You might have a low tolerance for bright lights and loud sounds before and during a migraine attack.
What to do if you have pre-migraine symptoms
You can start to take action if you recognize pre-migraine symptoms. If you’re being treated by a doctor for migraine, they can help you come up with a pre-migraine management plan that could prevent a full migraine attack from occurring. Try these common steps that can help during the prodrome stage:
- Take pain-relieving medication. It can help to take pain-relieving medication before a migraine attack begins. You can use over-the-counter (OTC) options such as Excedrin, or prescription options. Follow the doctor’s instructions carefully when taking prescription medication for migraine.
- Take any prevention medications. Be careful to not skip a dose of any prevention medications you’ve been prescribed if you’re having prodrome symptoms.
- Avoid any known migraine triggers. It’s always a good idea to avoid anything that triggers your migraine, but taking extra care to avoid triggers when you notice pre migraine symptoms can help prevent a full migraine attack.
- Rest and relax. Taking time to rest and relax can help you prevent a full migraine attack. If you can, try taking a nap or going to bed early. Meditation or other relaxation techniques can be especially useful.
- Find a dark room. It’s best to avoid loud, bright, and stressful situations when pre migraine symptoms occur. Relaxing in a dark and quiet room can help prevent a migraine attack.
- Take a hot shower or bath. A hot shower or bath can help relax your muscles. You can also try warm compresses.
- Try ice packs. Ice packs are a good way to numb your pain and help you rest.
- Drink a caffeinated beverage. Small amounts of caffeine can help relieve pain and can enhance the effects of some OTC pain relief medications. It’s a good idea to stick to a small amount, such as a single cup of coffee or can of soda. Too much caffeine can lead to withdrawal headaches and make it difficult to sleep.
What are the other stages of migraine?
There are three other migraine stages. Not everyone will have every stage during every migraine attack. The migraine stages are:
- Aura stage. For individuals who have an aura with migraine, they usually occur about an hour before a migraine attack. Auras symptoms can vary but often include blurry vision, seeing flashing lights, visual hallucinations, vision loss, numbness, dizziness, and changes in hearing and speech. About one-third of people with migraine experience aura.
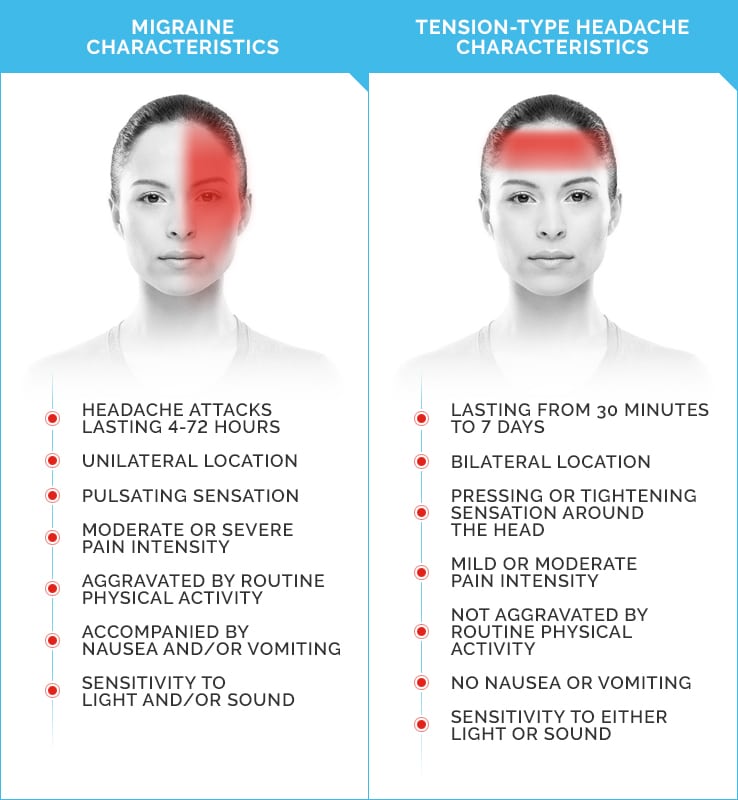
- Headache or attack stage. The headache stage is when moderate-to-severe head pain that’s normally concentrated on one side of your head occurs. Pain is often throbbing and can become more severe when you move. The attack stage can last anywhere from a few hours to 3 days and also includes migraine symptoms such as nausea, vomiting, trouble sleeping, and sensitivity to light, sound, and smells.
- Postdrome or resolution stage. This stage occurs once the migraine attack has faded and can last for a few hours to a few days. Symptoms at this stage often include feeling drained, fatigued, dizzy, and achy. It’s best to continue to avoid triggers and rest as much as you need during this stage.
The takeaway
The pre-migraine stage can start anywhere from a few days to a few hours before you have a migraine attack. Symptoms can vary, but often include:
- confusion
- fatigue
- urinary frequency
- sensitivity to light and sound
- mood changes
- neck pain
- food cravings
Learning to recognize pre-migraine symptoms you experience can help you manage migraine and avoid an attack. Talk with a doctor if you’re having migraine attacks frequently. They can help identify your pre-migraine symptoms and the steps you can take during pre-migraine to avoid an attack.
A natural peptide could help tackle obesity and diabetes
- Peptides are smaller versions of proteins that have a range of purposes, such as the potential to reduce the signs of aging, relieve inflammation, or promote muscle growth.
- In 2015, researchers discovered a type of peptide called PEPITEM, and recognized its function in the adiponectin-PEPITEM pathway, which regulates the onset and severity of autoimmune or chronic inflammatory conditions.
- Now, new research in animal models reveals that this peptide has the potential to offer a groundbreaking solution for many diseases.
- The peptide may decrease the chances of developing type 2 diabetes and other conditions associated with obesity, such as fatty liver disease, the study indicates.
Obesity leads to significant changes in adipose (fat) tissue metabolism, harms the pancreas, impairs insulin sensitivity, and eventually causes hyperglycemia (high blood sugar), which is the foundation of type 2 diabetes.
Additionally, it triggers a low-grade inflammatory reaction throughout the body, which promotes the infiltration of white blood cells into numerous tissues, including fat deposits located deep within the body that surround organs, such as the liver and gut — called visceral adipose tissue — and the peritoneal cavity, a delicate membrane that encloses the gut.
According to a new study, published in Clinical and Experimental Immunology, the adiponectin-PEPITEM pathway provides a link between obesity, the accompanying low-grade inflammatory response, and modifications in the pancreas that occur prior to the onset of diabetes.
Using a mouse model of obesity, the researchers administered the peptide PEPITEM using a slow-release pump, to see if it could prevent or perhaps even reverse the impacts of a high-fat diet on the pancreas.
The researchers found that administering PEPITEM to mice that were following a high-fat diet resulted in a significant reduction in the enlargement of insulin-producing cells in the pancreas and the number of white blood cells in the visceral adipose tissue and peritoneal cavity when compared to the control group.
Scale of problem in diabetes
Diabetes is a non-communicable disease (NCD) where the amount of glucose in the blood is too high. Type 1 diabetes is an autoimmune disease whereby the body is unable to produce any insulin, and Type 2 diabetes develops when the body stops producing enough insulin or the body’s cells stop reacting to insulin produced.
Type 2 diabetes is associated with lifestyle factors – being overweight or obese is the major modifiable risk factor for Type 2 diabetes. The onset of Type 2 diabetes can be delayed or prevented through support to change behaviour around lifestyle choices. Type 1 diabetes is not related to lifestyle issues, and at this point cannot be prevented.
Risk factors for Type 2 diabetes
The obesogenic environment and associated lifestyle risk factors
The increasingly obesogenic environment we live in makes it harder for individuals to avoid unhealthy lifestyle choices. The obesogenic environment can be considered to be at the root of the prevention challenge in Type 2 diabetes.
From childhood, people are exposed to ultra-processed, energy-dense, nutrient-poor foods, which are cheap and readily available. Opportunities for physical activity, both in and out of school and the workplace, have been reduced and more time is spent on screen-based and sedentary leisure activities. As a result, high proportions of children and adults have increasingly been defaulting to unhealthy lifestyle choices including unhealthy diets, low levels of physical activity, and sedentary behaviour. These all give rise to higher risk of Type 2 diabetes:
- overweight or obesity with a body mass index (BMI) of 25 or more
- a large waist circumference – more than 80cm or 31.5 inches in women and 94cm or 37 inches in men
Breast Cancer
Breast cancer
Overview
Breast cancer is cancer that forms in the cells of the breasts.
After skin cancer, breast cancer is the most common cancer diagnosed in women in the United States. Breast cancer can occur in both men and women, but it’s far more common in women.
Substantial support for breast cancer awareness and research funding has helped create advances in the diagnosis and treatment of breast cancer. Breast cancer survival rates have increased, and the number of deaths associated with this disease is steadily declining, largely due to factors such as earlier detection, a new personalized approach to treatment and a better understanding of the disease.
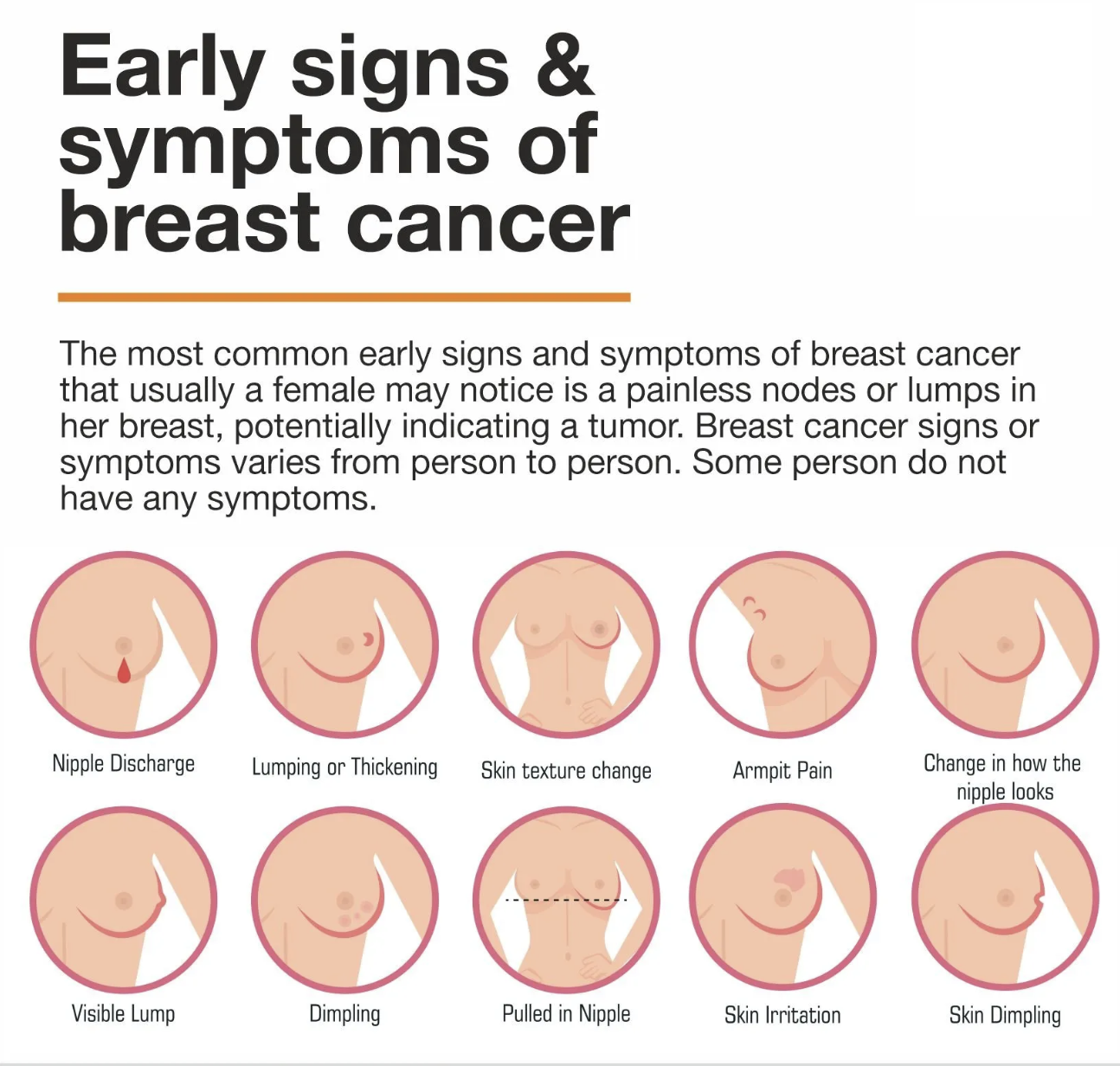
Symptoms
Signs and symptoms of breast cancer may include:
- A breast lump or thickening that feels different from the surrounding tissue
- Change in the size, shape or appearance of a breast
- Changes to the skin over the breast, such as dimpling
- A newly inverted nipple
- Peeling, scaling, crusting or flaking of the pigmented area of skin surrounding the nipple (areola) or breast skin
- Redness or pitting of the skin over your breast, like the skin of an orange
When to see a doctor
If you find a lump or other change in your breast — even if a recent mammogram was normal — make an appointment with your doctor for prompt evaluation.
Causes
Doctors know that breast cancer occurs when some breast cells begin to grow abnormally. These cells divide more rapidly than healthy cells do and continue to accumulate, forming a lump or mass. Cells may spread (metastasize) through your breast to your lymph nodes or to other parts of your body.
Breast cancer most often begins with cells in the milk-producing ducts (invasive ductal carcinoma). Breast cancer may also begin in the glandular tissue called lobules (invasive lobular carcinoma) or in other cells or tissue within the breast.
Researchers have identified hormonal, lifestyle and environmental factors that may increase your risk of breast cancer. But it’s not clear why some people who have no risk factors develop cancer, yet other people with risk factors never do. It’s likely that breast cancer is caused by a complex interaction of your genetic makeup and your environment.
Inherited breast cancer
Doctors estimate that about 5 to 10 percent of breast cancers are linked to gene mutations passed through generations of a family.
A number of inherited mutated genes that can increase the likelihood of breast cancer have been identified. The most well-known are breast cancer gene 1 (BRCA1) and breast cancer gene 2 (BRCA2), both of which significantly increase the risk of both breast and ovarian cancer.
If you have a strong family history of breast cancer or other cancers, your doctor may recommend a blood test to help identify specific mutations in BRCA or other genes that are being passed through your family.
Consider asking your doctor for a referral to a genetic counselor, who can review your family health history. A genetic counselor can also discuss the benefits, risks and limitations of genetic testing to assist you with shared decision-making.
Risk factors
A breast cancer risk factor is anything that makes it more likely you’ll get breast cancer. But having one or even several breast cancer risk factors doesn’t necessarily mean you’ll develop breast cancer. Many women who develop breast cancer have no known risk factors other than simply being women.
Factors that are associated with an increased risk of breast cancer include:
- Being female. Women are much more likely than men are to develop breast cancer.
- Increasing age. Your risk of breast cancer increases as you age.
- A personal history of breast conditions. If you’ve had a breast biopsy that found lobular carcinoma in situ (LCIS) or atypical hyperplasia of the breast, you have an increased risk of breast cancer.
- A personal history of breast cancer. If you’ve had breast cancer in one breast, you have an increased risk of developing cancer in the other breast.
- A family history of breast cancer. If your mother, sister or daughter was diagnosed with breast cancer, particularly at a young age, your risk of breast cancer is increased. Still, the majority of people diagnosed with breast cancer have no family history of the disease.
- Inherited genes that increase cancer risk. Certain gene mutations that increase the risk of breast cancer can be passed from parents to children. The most well-known gene mutations are referred to as BRCA1 and BRCA2. These genes can greatly increase your risk of breast cancer and other cancers, but they don’t make cancer inevitable.
- Radiation exposure. If you received radiation treatments to your chest as a child or young adult, your risk of breast cancer is increased.
- Obesity. Being obese increases your risk of breast cancer.
- Beginning your period at a younger age. Beginning your period before age 12 increases your risk of breast cancer.
- Beginning menopause at an older age. If you began menopause at an older age, you’re more likely to develop breast cancer.
- Having your first child at an older age. Women who give birth to their first child after age 30 may have an increased risk of breast cancer.
- Having never been pregnant. Women who have never been pregnant have a greater risk of breast cancer than do women who have had one or more pregnancies.
- Postmenopausal hormone therapy. Women who take hormone therapy medications that combine estrogen and progesterone to treat the signs and symptoms of menopause have an increased risk of breast cancer. The risk of breast cancer decreases when women stop taking these medications.
- Drinking alcohol. Drinking alcohol increases the risk of breast cancer.
Prevention
Breast cancer risk reduction for women with an average risk
Making changes in your daily life may help reduce your risk of breast cancer. Try to:
- Ask your doctor about breast cancer screening. Discuss with your doctor when to begin breast cancer screening exams and tests, such as clinical breast exams and mammograms.
Talk to your doctor about the benefits and risks of screening. Together, you can decide what breast cancer screening strategies are right for you. - Become familiar with your breasts through breast self-exam for breast awareness. Women may choose to become familiar with their breasts by occasionally inspecting their breasts during a breast self-exam for breast awareness. If there is a new change, lumps or other unusual signs in your breasts, talk to your doctor promptly.
Breast awareness can’t prevent breast cancer, but it may help you to better understand the normal changes that your breasts undergo and identify any unusual signs and symptoms. - Drink alcohol in moderation, if at all. Limit the amount of alcohol you drink to no more than one drink a day, if you choose to drink.
- Exercise most days of the week. Aim for at least 30 minutes of exercise on most days of the week. If you haven’t been active lately, ask your doctor whether it’s OK and start slowly.
- Limit postmenopausal hormone therapy. Combination hormone therapy may increase the risk of breast cancer. Talk with your doctor about the benefits and risks of hormone therapy.
Some women experience bothersome signs and symptoms during menopause and, for these women, the increased risk of breast cancer may be acceptable in order to relieve menopause signs and symptoms.
To reduce the risk of breast cancer, use the lowest dose of hormone therapy possible for the shortest amount of time. - Maintain a healthy weight. If your weight is healthy, work to maintain that weight. If you need to lose weight, ask your doctor about healthy strategies to accomplish this. Reduce the number of calories you eat each day and slowly increase the amount of exercise.
- Choose a healthy diet. Women who eat a Mediterranean diet supplemented with extra-virgin olive oil and mixed nuts may have a reduced risk of breast cancer. The Mediterranean diet focuses mostly on plant-based foods, such as fruits and vegetables, whole grains, legumes, and nuts. People who follow the Mediterranean diet choose healthy fats, such as olive oil, over butter and fish instead of red meat.
Breast cancer risk reduction for women with a high risk
If your doctor has assessed your family history and determined that you have other factors, such as a precancerous breast condition, that increase your risk of breast cancer, you may discuss options to reduce your risk, such as:
- Preventive medications (chemoprevention). Estrogen-blocking medications, such as selective estrogen receptor modulators and aromatase inhibitors, reduce the risk of breast cancer in women with a high risk of the disease.
These medications carry a risk of side effects, so doctors reserve these medications for women who have a very high risk of breast cancer. Discuss the benefits and risks with your doctor. - Preventive surgery. Women with a very high risk of breast cancer may choose to have their healthy breasts surgically removed (prophylactic mastectomy). They may also choose to have their healthy ovaries removed (prophylactic oophorectomy) to reduce the risk of both breast cancer and ovarian cancer.
Diagnosing Flu
How do I know if I have flu?
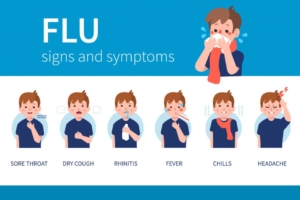
Your respiratory illness might be influenza (flu) if you have fever, cough, sore throat, runny or stuffy nose, body aches, headache, chills and/or fatigue. Some people may have vomiting and diarrhea, though this is more common in children. People may be sick with flu and have respiratory symptoms without a fever. Flu viruses usually cause the most illness during the colder months of the year. However, flu can also occur outside of the typical flu season. In addition, other viruses can also cause respiratory illness similar to flu. So, it is impossible to tell for sure if you have flu based on symptoms alone. If your doctor needs to know for sure whether you are sick with flu, there are laboratory tests that can be done.
What kinds of flu tests are there?
A number of tests are available to detect flu viruses in respiratory specimens. The most common are called “rapid influenza diagnostic tests (RIDTs).” RIDTs work by detecting the parts of the virus (antigens) that stimulate an immune response. These tests can provide results within approximately 10-15 minutes but may not be as accurate as other flu tests. Therefore, you could still have flu, even though your rapid test result is negative. Other flu tests called “rapid molecular assays” detect genetic material of the flu virus. Rapid molecular assays produce results in 15-20 minutes and are more accurate than RIDTs.
In addition to RIDTs and rapid molecular assays, there are several more accurate flu tests available that must be performed in specialized laboratories, such as hospital and public health laboratories. These tests include reverse transcription polymerase chain reaction (RT-PCR), viral culture, and immunofluorescence assays. All of these tests require that a health care provider swipe the inside of your nose or the back of your throat with a swab and then send the swab for testing. Results may take one to several hours.
How well can rapid tests detect flu?
During a flu outbreak, a positive rapid flu test is likely to indicate flu virus infection. However, rapid tests vary in their ability to detect flu viruses, depending on the type of rapid test used, and on the type of flu viruses circulating. Also, rapid tests appear to be better at detecting flu in children than in adults. This variation in ability to detect viruses can result in some people who are infected with flu having a negative rapid test result. This situation is called a false negative test result. Despite a negative rapid test result, your health care provider may diagnose you with flu based on your symptoms and their clinical judgment.
Will my health care provider test me for flu if I have flu-like symptoms?
While your doctor may test you for flu, not everyone who goes to the doctor with flu-like symptoms will be tested. After evaluating you, your doctor may choose to diagnose you with flu without the need for testing based on your symptoms and his or her own clinical judgement.
Difference Between Flu and COVID-19
Influenza (Flu) and COVID-19 are both contagious respiratory illnesses, but they are caused by different viruses. COVID-19 is caused by infection with a coronavirus named SARS-CoV-2, and flu is caused by infection with influenza viruses. You cannot tell the difference between flu and COVID-19 by symptoms alone because some of the symptoms are the same. Some PCR tests can differentiate between flu and COVID-19 at the same time. If one of these tests is not available, many testing locations provide flu and COVID-19 tests separately. Talk to a healthcare provider about getting tested for both flu and COVID-19 if you have symptoms.
Can I have flu and COVID-19 at the same time?
Yes. It is possible to have flu as well as other respiratory illnesses including COVID-19 at the same time. Health experts are still studying how common this can be.
Is there a test that can detect both flu and COVID-19?
Yes. There is a test that will check for seasonal flu type A and B viruses and SARS-CoV-2, the virus that causes COVID-19. This test is being used by U.S. public health laboratories for surveillance purposes. Testing for these viruses at the same time will give public health officials important information about how flu and COVID-19 are spreading and what prevention steps should be taken. The test will also help public health laboratories save time and testing materials, and possibly to return test results faster.
The Food and Drug Administration (FDA) has given CDC an Emergency Use Authorization for this new test. Initial test kits were sent to public health laboratories in early August 2020. CDC will continue to manufacture and distribute these kits.