Alcohol Use and Your Health
What is a standard drink?
In the United States, a standard drink contains 0.6 ounces (14.0 grams or 1.2 tablespoons) of pure alcohol. Generally, this amount of pure alcohol is found in
- 12-ounces of beer (5% alcohol content).
- 8-ounces of malt liquor (7% alcohol content).
- 5-ounces of wine (12% alcohol content).
- 1.5-ounces of 80-proof (40% alcohol content) distilled spirits or liquor (e.g., gin, rum, vodka, whiskey).
What is excessive drinking?
Excessive drinking includes binge drinking, heavy drinking, and any drinking by pregnant women or people younger than age 21.
- Binge drinking, the most common form of excessive drinking, is defined as consuming
- For women, 4 or more drinks during a single occasion.
- For men, 5 or more drinks during a single occasion.
- Heavy drinking is defined as consuming
- For women, 8 or more drinks per week.
- For men, 15 or more drinks per week.
Most people who drink excessively are not alcoholics or alcohol dependent.
What is moderate drinking?
The Dietary Guidelines for Americans recommends that adults of legal drinking age can choose not to drink, or to drink in moderation by limiting intake to 2 drinks or less in a day for men or 1 drink or less in a day for women, on days when alcohol is consumed.4 The Guidelines also do not recommend that individuals who do not drink alcohol start drinking for any reason and that if adults of legal drinking age choose to drink alcoholic beverages, drinking less is better for health than drinking more.
There are some people who should not drink any alcohol, including those who are:
- Younger than age 21.
- Pregnant or may be pregnant.
- Driving, planning to drive, or participating in other activities requiring skill, coordination, and alertness.
- Taking certain prescription or over-the-counter medications that can interact with alcohol.
- Suffering from certain medical conditions.
- Recovering from alcoholism or are unable to control the amount they drink.
By adhering to the Dietary Guidelines, you can reduce the risk of harm to yourself or others.
Short-Term Health Risks
Excessive alcohol use has immediate effects that increase the risk of many harmful health conditions. These are most often the result of binge drinking and include the following:
- Injuries, such as motor vehicle crashes, falls, drownings, and burns.
- Violence, including homicide, suicide, sexual assault, and intimate partner violence.
- Alcohol poisoning, a medical emergency that results from high blood alcohol levels.
- Risky sexual behaviors, including unprotected sex or sex with multiple partners. These behaviors can result in unintended pregnancy or sexually transmitted diseases, including HIV.
- Miscarriage and stillbirth or fetal alcohol spectrum disorders (FASDs) among pregnant women.
Long-Term Health Risks
Over time, excessive alcohol use can lead to the development of chronic diseases and other serious problems including:
- High blood pressure, heart disease, stroke, liver disease, and digestive problems.
- Cancer of the breast, mouth, throat, esophagus, voice box, liver, colon, and rectum.
- Weakening of the immune system, increasing the chances of getting sick.
- Learning and memory problems, including dementia and poor school performance.
- Mental health problems, including depression and anxiety.
- Social problems, including family problems, job-related problems, and unemployment.
- Alcohol use disorders, or alcohol dependence.
By not drinking too much, you can reduce the risk of these short- and long-term health risks.
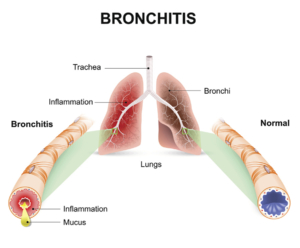
What is a chest cold (acute bronchitis)?
A chest cold, often called acute bronchitis, occurs when the airways of the lungs swell and produce mucus in the lungs. That’s what makes you cough. Acute bronchitis can last less than 3 weeks.
Causes
A virus usually causes acute bronchitis. Bacteria can sometimes cause acute bronchitis. But, even in these cases, taking antibiotics is NOT advised and will not help you get better.
Symptoms
Symptoms of acute bronchitis last less than 3 weeks and can include:
- Coughing with or without mucus
- Soreness in the chest
- Feeling tired (fatigue)
- Mild headache
- Mild body aches
- Sore throat
When to Seek Medical Care
Talk to a healthcare professional right away if your child is under 3 months old with a fever of 100.4 °F (38 °C) or higher.
See a doctor if you have any of the following:
- Temperature of 100.4 °F or higher
- Cough with bloody mucus
- Shortness of breath or trouble breathing
- Symptoms that last more than 3 weeks
- Repeated episodes of bronchitis
This list is not all-inclusive. Please see a doctor for any symptom that is severe or concerning.
Treatment
Acute bronchitis usually gets better on its own—without antibiotics. Antibiotics won’t help you get better if you have acute bronchitis.
When antibiotics aren’t needed, they won’t help you, and their side effects could still cause harm. Side effects can range from mild reactions, like a rash, to more serious health problems. These problems can include severe allergic reactions, antibiotic-resistant infections and C. diff infection. C. diff causes diarrhea that can lead to severe colon damage and death.
Other illnesses like whooping cough (pertussis) or pneumonia can have similar symptoms to acute bronchitis. If you have whooping cough or pneumonia, your doctor will most likely prescribe antibiotics.
How to Feel Better
Below are some ways you can feel better while your body fights off acute bronchitis:
- Get plenty of rest.
- Drink plenty of fluids.
- Use a clean humidifier or cool mist vaporizer.
- Use saline nasal spray or drops to relieve a stuffy nose.
- For young children, use a rubber suction bulb to clear mucus.
- Breathe in steam from a bowl of hot water or shower.
- Suck on lozenges. Do not give lozenges to children younger than 4 years of age.
- Use honey to relieve cough for adults and children at least 1 year of age or older.
Ask your doctor or pharmacist about over-the-counter medicines that can help you feel better. Always use over-the-counter medicines as directed. Remember, over-the-counter medicines may provide temporary relief of symptoms, but they will not cure your illness.
Over-the-Counter Medicine and Children
Carefully read and follow instructions on over-the-counter medicine product labels before giving medicines to children. Some over-the-counter medicines are not recommended for children of certain ages.
- Pain relievers:
- Children younger than 6 months: only give acetaminophen.
- Children 6 months or older: it is OK to give acetaminophen or ibuprofen.
- Never give aspirin to children because it can cause Reye’s syndrome. Reye’s syndrome is a very serious, but rare illness that can harm the liver and brain.
- Cough and cold medicines:
- Children younger than 4 years old: do not use over-the-counter cough and cold medicines in young children unless a doctor specifically tells you to. Cough and cold medicines can result in serious and sometimes life-threatening side effects in young children.
- Children 4 years or older: discuss with your child’s doctor if over-the-counter cough and cold medicines are safe to give to your child.
Ask your doctor or pharmacist about the right dosage of over-the-counter medicines for your child’s age and size. Also, tell your child’s doctor and pharmacist about all prescription and over-the-counter medicines they are taking.
Prevention
You can help prevent acute bronchitis by doing your best to stay healthy and keep others healthy, including:
- Clean your hands.
- Get recommended vaccines, such as the flu vaccine.
- Don’t smoke and avoid secondhand smoke.
- Cover your mouth and nose when coughing or sneezing.
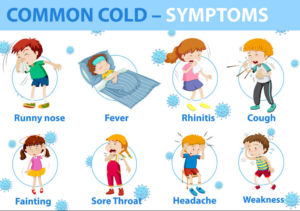
Common Colds
Sore throat and runny nose are usually the first signs of a cold, followed by coughing and sneezing. Most people recover in about 7-10 days. You can help reduce your risk of getting a cold: wash your hands often, avoid close contact with sick people, and don’t touch your face with unwashed hands.
Common colds are the main reason that children miss school and adults miss work. Each year in the United States, there are millions of cases of the common cold. Adults have an average of 2-3 colds per year, and children have even more.
Most people get colds in the winter and spring, but it is possible to get a cold any time of the year. Symptoms usually include:
- sore throat
- runny nose
- coughing
- sneezing
- headaches
- body aches
Most people recover within about 7-10 days. However, people with weakened immune systems, asthma, or respiratory conditions may develop serious illness, such as bronchitis or pneumonia.
Help reduce your risk of getting a cold by washing hands often with soap and water.
How to Protect Yourself
Viruses that cause colds can spread from infected people to others through the air and close personal contact. You can also get infected through contact with stool (poop) or respiratory secretions from an infected person. This can happen when you shake hands with someone who has a cold, or touch a surface, like a doorknob, that has respiratory viruses on it, then touch your eyes, mouth, or nose.
You can help reduce your risk of getting a cold:
- Wash your hands often with soap and water. Wash them for 20 seconds, and help young children do the same. If soap and water are not available, use an alcohol-based hand sanitizer. Viruses that cause colds can live on your hands, and regular handwashing can help protect you from getting sick.
- Avoid touching your eyes, nose, and mouth with unwashed hands. Viruses that cause colds can enter your body this way and make you sick.
- Stay away from people who are sick. Sick people can spread viruses that cause the common cold through close contact with others.
Practice good cough and sneeze etiquette: always cough and sneeze into a tissue or your upper shirt sleeve, completely covering your mouth and nose.
How to Protect Others
If you have a cold, you should follow these tips to help prevent spreading it to other people:
- Stay at home while you are sick and keep children out of school or daycare while they are sick.
- Avoid close contact with others, such as hugging, kissing, or shaking hands.
- Move away from people before coughing or sneezing.
- Cough and sneeze into a tissue then throw it away, or cough and sneeze into your upper shirt sleeve, completely covering your mouth and nose.
- Wash your hands after coughing, sneezing, or blowing your nose.
- Disinfect frequently touched surfaces and objects, such as toys, doorknobs, and mobile devices.
There is no vaccine to protect you against the common cold.
How to Feel Better
There is no cure for a cold. To feel better, you should get lots of rest and drink plenty of fluids. Over-the-counter medicines may help ease symptoms but will not make your cold go away any faster. Always read the label and use medications as directed. Talk to your doctor before giving your child nonprescription cold medicines, since some medicines contain ingredients that are not recommended for children. Learn more about symptom relief of upper respiratory infections, including colds.
Antibiotics will not help you recover from a cold caused by a respiratory virus. They do not work against viruses, and they may make it harder for your body to fight future bacterial infections if you take them unnecessarily.
When to See a Doctor
You should call your doctor if you or your child has one or more of these conditions:
- symptoms that last more than 10 days
- symptoms that are severe or unusual
- if your child is younger than 3 months of age and has a fever or is lethargic
You should also call your doctor right away if you are at high risk for serious flu complications and get flu symptoms such as fever, chills, and muscle or body aches. People at high risk for flu complications include young children (younger than 5 years old), adults 65 years and older, pregnant women, and people with certain medical conditions such as asthma, diabetes, and heart disease.
Your doctor can determine if you or your child has a cold or the flu and can recommend treatment to help with symptoms.
Causes of the Common Cold
Many different respiratory viruses can cause the common cold, but rhinoviruses are the most common. Rhinoviruses can also trigger asthma attacks and have been linked to sinus and ear infections. Other viruses that can cause colds include respiratory syncytial virus, human parainfluenza viruses, adenovirus, common human coronaviruses, and human metapneumovirus.
Know the Difference between Common Cold and Flu
The flu, which is caused by influenza viruses, also spreads and causes illness around the same time as the common cold. Because these two illnesses have similar symptoms, it can be difficult (or even impossible) to tell the difference between them based on symptoms alone. In general, flu symptoms are worse than the common cold and can include fever or feeling feverish/chills, cough, sore throat, runny or stuffy nose, muscle or body aches, headaches and fatigue (tiredness). Flu can also have very serious complications. CDC recommends a yearly flu vaccination as the first and best way to prevent the flu. If you get the flu, antiviral drugs may be a treatment option.
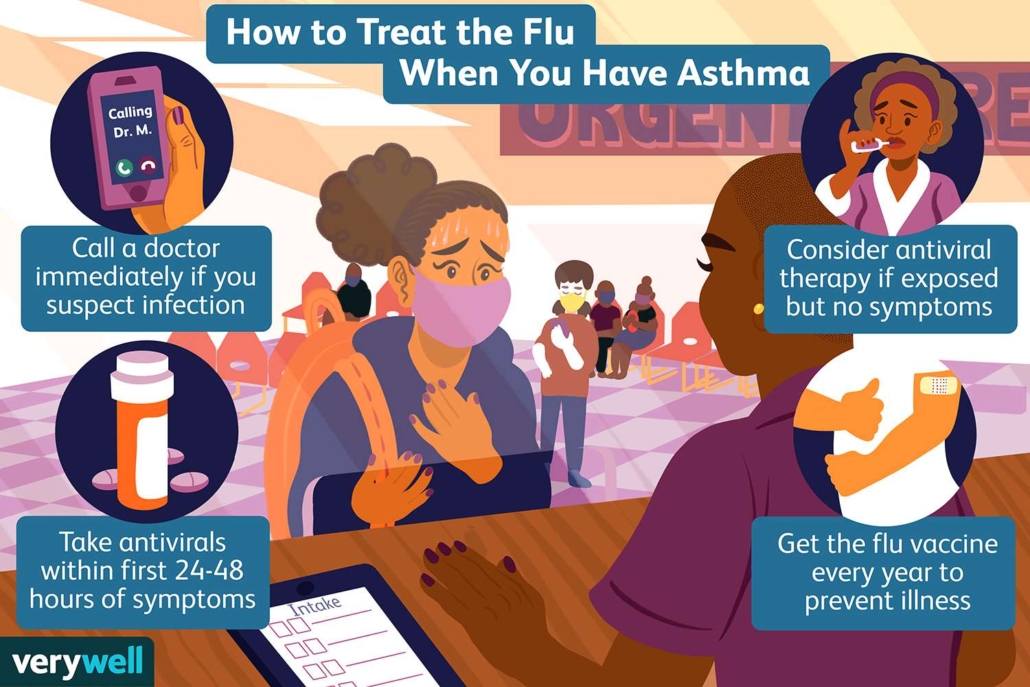
Flu & People with Asthma
Asthma is a lung disease that is caused by chronic inflammation (swelling) of the airways. It is one of the most common long-term diseases among children, but adults can have asthma, too. Asthma attacks occur when the lung airways become swollen and tighten due to airway inflammation. Asthma attacks can be caused by “triggers” such as airway infections, allergy particles, chemical irritants, and air pollution. During an asthma attack, a person with asthma can experience symptoms such as wheezing, breathlessness, chest tightness, and nighttime or early morning coughing. Often, asthma attacks can be prevented by limiting one’s exposure to triggers and by properly using asthma medications.More
A Flu Shot is the Best Protection Against Flu
Flu vaccination is especially important for people with asthma because they are at higher risk of developing serious flu complications. Flu vaccines are reviewed each year and updated as needed to keep up with changing viruses. Also, protection from vaccination decreases over time, so annual flu vaccination is needed to ensure the best possible protection against flu. A flu vaccine protects against the four flu viruses that research indicates will be most common during the upcoming season. Flu vaccines have been updated for the 2022-2023 season. More information on why flu vaccines are updated annually is available at Vaccine Virus Selection.
Immunity from flu vaccination sets in after about two weeks after getting vaccinated. In addition to reducing risk of flu, flu vaccination has been shown in several studies to reduce severity of illness in people who get vaccinated but still get sick with flu:
- Flu vaccination has been shown to reduce the risk of getting sick with flu as well as reduce the risk of having a serious flu outcome like a stay in the hospital or even being admitted to the intensive care unit (ICU).
- More information is available at What are the benefits of flu vaccination? | CDC.
CDC recommends that everyone 6 months and older get a seasonal flu vaccine each year, ideally by the end of October.
Chest Cold (Acute Bronchitis)
Cough keeping you up at night? Soreness in your chest and feeling tired? You could have a chest cold.
Antibiotics will not help you get better if you have a chest cold (acute bronchitis).
If you’re healthy without heart or lung problems or a weakened immune system, this information is for you.
What is a chest cold (acute bronchitis)?
A chest cold, often called acute bronchitis, occurs when the airways of the lungs swell and produce mucus in the lungs. That’s what makes you cough. Acute bronchitis can last less than 3 weeks.
Causes
A virus usually causes acute bronchitis. Bacteria can sometimes cause acute bronchitis. But, even in these cases, taking antibiotics is NOT advised and will not help you get better.
Symptoms
Symptoms of acute bronchitis last less than 3 weeks and can include:
- Coughing with or without mucus
- Soreness in the chest
- Feeling tired (fatigue)
- Mild headache
- Mild body aches
- Sore throat
When to Seek Medical Care
Talk to a healthcare professional right away if your child is under 3 months old with a fever of 100.4 °F (38 °C) or higher.
See a doctor if you have any of the following:
- Temperature of 100.4 °F or higher
- Cough with bloody mucus
- Shortness of breath or trouble breathing
- Symptoms that last more than 3 weeks
- Repeated episodes of bronchitis
This list is not all-inclusive. Please see a doctor for any symptom that is severe or concerning.
Treatment
Acute bronchitis usually gets better on its own—without antibiotics. Antibiotics won’t help you get better if you have acute bronchitis.
When antibiotics aren’t needed, they won’t help you, and their side effects could still cause harm. Side effects can range from mild reactions, like a rash, to more serious health problems. These problems can include severe allergic reactions, antibiotic-resistant infections and C. diff infection. C. diff causes diarrhea that can lead to severe colon damage and death.
Other illnesses like whooping cough (pertussis) or pneumonia can have similar symptoms to acute bronchitis. If you have whooping cough or pneumonia, your doctor will most likely prescribe antibiotics.
How to Feel Better
Below are some ways you can feel better while your body fights off acute bronchitis:
- Get plenty of rest.
- Drink plenty of fluids.
- Use a clean humidifier or cool mist vaporizer.
- Use saline nasal spray or drops to relieve a stuffy nose.
- For young children, use a rubber suction bulb to clear mucus.
- Breathe in steam from a bowl of hot water or shower.
- Suck on lozenges. Do not give lozenges to children younger than 4 years of age.
- Use honey to relieve cough for adults and children at least 1 year of age or older.
Ask your doctor or pharmacist about over-the-counter medicines that can help you feel better. Always use over-the-counter medicines as directed. Remember, over-the-counter medicines may provide temporary relief of symptoms, but they will not cure your illness.
Over-the-Counter Medicine and Children
Carefully read and follow instructions on over-the-counter medicine product labels before giving medicines to children. Some over-the-counter medicines are not recommended for children of certain ages.
- Pain relievers:
- Children younger than 6 months: only give acetaminophen.
- Children 6 months or older: it is OK to give acetaminophen or ibuprofen.
- Never give aspirin to children because it can cause Reye’s syndrome. Reye’s syndrome is a very serious, but rare illness that can harm the liver and brain.
- Cough and cold medicines:
- Children younger than 4 years old: do not use over-the-counter cough and cold medicines in young children unless a doctor specifically tells you to. Cough and cold medicines can result in serious and sometimes life-threatening side effects in young children.
- Children 4 years or older: discuss with your child’s doctor if over-the-counter cough and cold medicines are safe to give to your child.
Ask your doctor or pharmacist about the right dosage of over-the-counter medicines for your child’s age and size. Also, tell your child’s doctor and pharmacist about all prescription and over-the-counter medicines they are taking.
Prevention
You can help prevent acute bronchitis by doing your best to stay healthy and keep others healthy, including:
- Clean your hands.
- Get recommended vaccines, such as the flu vaccine.
- Don’t smoke and avoid secondhand smoke.
- Cover your mouth and nose when coughing or sneezing.
Know Your Risk for High Blood Pressure

Risk factors that can increase your risk of high blood pressure include health conditions, your lifestyle, and your family history.
Some of the risk factors for high blood pressure cannot be controlled, such as your age or family history. But you can take steps to lower your risk by changing the factors you can control.
Some medical conditions can raise your risk for high blood pressure. If you have one of these conditions, you can take steps to manage it and lower your risk for high blood pressure.
Elevated Blood Pressure
Elevated blood pressure is blood pressure that is slightly higher than normal. High blood pressure usually develops over time. Having blood pressure that is slightly higher than normal increases your risk for developing chronic, or long-lasting, high blood pressure in the future.
If your blood pressure is between 120/80 mmHg and 129/80 mmHg, you have elevated blood pressure. Learn more about how blood pressure is measured.
You can take steps to manage your blood pressure and keep it in a healthy range.
Diabetes
About 6 out of 10 of people who have diabetes also have high blood pressure.1Diabetes causes sugars to build up in the blood and also increases the risk for heart disease.
Talk with your doctor about ways to manage diabetes and control other risk factors.
What behaviors increase risk for high blood pressure?
Your lifestyle choices can increase your risk for high blood pressure. To reduce your risk, your doctor may recommend changes to your lifestyle.
The good news is that healthy behaviors can lower your risk for high blood pressure.
Unhealthy Diet
A diet that is too high in sodium and too low in potassium puts you at risk for high blood pressure.
Eating too much sodium—an element in table salt—increases blood pressure. Most of the sodium we eat comes from processed and restaurant foods. Learn more about sodium and high blood pressure.
Not eating enough potassium—a mineral that your body needs to work properly—also can increase blood pressure. Potassium is found in many foods; bananas, potatoes, beans, and yogurt have high levels of potassium.
Physical Inactivity
Getting regular physical activity helps your heart and blood vessels stay strong and healthy, which may help lower your blood pressure. Regular physical activity can also help you keep a healthy weight, which may also help lower your blood pressure.
Obesity
Having obesity is having excess body fat. Having obesity or overweight also means your heart must work harder to pump blood and oxygen around your body. Over time, this can add stress to your heart and blood vessels.
Obesity is linked to higher “bad” cholesterol and triglyceride levels and to lower “good” cholesterol levels. Learn more about cholesterol.
In addition to high blood pressure, having obesity can also lead to heart disease and diabetes. Talk to your health care team about a plan to reduce your weight to a healthy level.
Too Much Alcohol
Drinking too much alcohol can raise your blood pressure.
- Women should have no more than one drink a day.
- Men should have no more than two drinks a day.
Tobacco Use
Tobacco use increases your risk for high blood pressure. Smoking can damage the heart and blood vessels. Nicotine raises blood pressure, and breathing in carbon monoxide—which is produced from smoking tobacco—reduces the amount of oxygen that your blood can carry.
What other factors increase my risk for high blood pressure?
Family members share genes, behaviors, lifestyles, and environments that can influence their health and their risk for disease. High blood pressure can run in a family, and your risk for high blood pressure can increase based on your age and your race or ethnicity.
Genetics and Family History
When members of a family pass traits from one generation to another through genes, that process is called heredity.
Genes likely play some role in high blood pressure, heart disease, and other related conditions. However, it is also likely that people with a family history of high blood pressure share common environments and other potential factors that increase their risk.
The risk for high blood pressure can increase even more when heredity combines with unhealthy lifestyle choices, such as smoking and eating an unhealthy diet.
Find out more about genetics and disease on CDC’s Office of Public Health Genomics website.
Family health history is a record of the diseases and health conditions people in your family have had. Family health history is a useful tool for understanding health risks and preventing disease. To help people collect and organize information on their family history, CDC’s Office of Public Health Genomics collaborated with the Surgeon General and other federal agencies to develop a Web-based tool called My Family Health Portrait.
Other Characteristics
Both men and women can have high blood pressure. Some other characteristics that you cannot control—such as your age, race, or ethnicity—can affect your risk for high blood pressure.
- Age. Because your blood pressure tends to rise as you get older, your risk for high blood pressure increases with age. About 9 out of 10 Americans will develop high blood pressure during their lifetime.2
- Sex. Women are about as likely as men to develop high blood pressure at some point during their lives.
- Race or ethnicity. Black people develop high blood pressure more often than white people, Hispanics, Asians, Pacific Islanders, American Indians, or Alaska Natives do. Compared with white people, black people also develop high blood pressure earlier in life.