How to Advocate for Yourself and Your Baby During Delivery
Babies are unpredictable. Knowing your rights can help you better prepare for the unpredictable.
After 9 months of nausea, weight gain, back pain, and general discomfort, the day is finally here: delivery day. And, if you’re anything like me, you are more than ready.
I was trying to evict my daughter as soon as she turned 37 weeks.
But before you head to labor and delivery, you should know what your rights are (and aren’t). Because while you may have a well-written birth plan, things change, and it’s important that you know how to advocate for yourself and your baby.
The basics
You have the right to receive full and clear information about the benefits and risks of any medication, treatment, test, or procedure you may receive
Things move quickly in labor and delivery wards, and for good reason. Childbirth can be unpredictable, and most medical professionals act abruptly out of necessity. They simply want to ensure a safe and healthy delivery.
But before receiving any treatment, you can (and should) ask about the risks and results of procedures. It’s your legal right and duty to give permission for care.
You have the right to receive full and clear information about your healthcare professional’s background and qualifications
When it comes to your OB-GYN, transparency isn’t just important, it’s your right.
Ask about their medical training and degree. Inquire how many years of experience they have (and how many babies they’ve delivered), and request any other information which you deem necessary. For example, you can ask how many vaginal and Cesarean births they’ve attended.
You have the right to receive treatment that’s appropriate for your cultural and religious background
This includes refusing certain medical procedures and receiving written correspondence in a language of your choosing.
You have the right to accept or refuse any unnecessary medical test, intervention, or procedure, including continuous fetal monitoring or an episiotomy
While certain birthing situations require intervention — sometimes it’s medically necessary to perform a C-section or monitor your unborn babe — if you’re laboring naturally and there is no fetal or maternal distress, you have the right to accept or refuse any test or procedure.
You have the right to change your mind
If something doesn’t feel right or if you’re having second thoughts, speak up. Period.
The birth process
You have the right to know if you will be induced (and why)
Some pregnancy complications may require you to be induced. In fact, in certain cases, it may be the best way to keep you and your baby healthy.
However, many inductions are unnecessary, and in some cases, can increase your risk of complications.
You have the right to labor in whatever position you choose
Barring any unforeseen problems or medically restrictive devices (such as a catheter), you can — and should — be able to labor in any position.
Some hospitals have various policies in place when it comes to delivery. If you’re planning a hospital delivery, ask about their policies ahead of time.
Newborn care
You have the right to uninterrupted contact with your newborn
There are numerous benefits of skin-to-skin contact, both immediately following birth and in the days and weeks after. As long as you and your baby are healthy, you should be given (and are entitled to) relatively uninterrupted time to bond with your child.
You have the right to breastfeed or bottle feed
While the benefits of breast milk are well-researched and well-known, not everyone can or wants to. (I stopped breastfeeding to resume my regular mental health care regimen.)
Do what is best and right for you.
You have the right to deny unnecessary medical tests or procedures
After your child is born, medical professionals will likely perform a series of tests on your wee one. For example, your newborn will be measured, weighed, given an APGAR test, and blood will be drawn.
However, not all procedures need to be done immediately after birth (or in the hospital). Speak to your OB-GYN or pediatrician in advance to better understand what they recommend doing and when.
You are your own best advocate
You should speak up, ask questions, and remember this is your birth experience and your child.
If something doesn’t seem or feel right, or if you have questions, it’s your right to ask questions and receive answers.
Kimberly Zapata is a mother, writer, and mental health advocate. Her work has appeared on several sites, including the Washington Post, HuffPost, Oprah, Vice, Parents, Health, and Scary Mommy — to name a few. When her nose isn’t buried in work (or a good book), Kimberly spends her free time running Greater Than: Illness, a nonprofit organization that aims to empower children and young adults struggling with mental health conditions.
2 servings of avocado per week may cut heart disease risk by 16%
- Researchers examined the relationship between avocado consumption and cardiovascular events.
- They found that eating 2 or more servings of avocado per week is linked to 16% fewer cardiovascular events over a 30-year period. One serving is half an avocado, or 80 grams (g).
- The researchers conclude that replacing certain fat-containing foods with avocado could lower cardiovascular disease risk.
- The note however that replacing plant oils with avocado is linked to a 45% higher stroke risk.
Cardiovascular disease (CVD) is the leading cause of death worldwide. However, it can be prevented through lifestyle factors like diet.
The American Heart Association (AHA) recommends limiting 5 to 6% of calories intake from saturated fatty acid (SFA), and replacing SFA and trans-fats with monounsaturated fats (MUFA) and polyunsaturated fats for better heart health.
Avocados are rich in MUFAs and polyunsaturated fats. Studies have found that their regular consumption reduces triglycerides, low-density lipoprotein (LDL) cholesterol, and total cholesterol level.
Most studies on avocado consumption have focused on cardiovascular risk factors. Studies investigating the link between avocado consumption and cardiovascular events could improve understanding of the fruit’s health benefits.
Recently, researchers have investigated the link between avocado consumption and cardiovascular events.
They found that higher consumption of avocados was linked to a lower risk of CVD and coronary heart disease (CHD).
“The […] results are significant and strengthen previous findings of avocados’ association with a lower risk of cardiovascular disease [as well as] reducing heart outcomes such as fatal and nonfatal myocardial infarction,” Bhanu Gupta, MD, cardiologist at The University of Kansas Health System, not involved in the study, told Medical News Today.
“Point to be noted: avocado consumption does not lower the risk of stroke in the study. Another point to be noted: avocado is not a replacement for healthy dietary fats such as olive oils, nuts, and other plant oils.”
– Dr. Gupta
The study was published in the Journal of the American Heart Association (JAHA)Trusted Source.
Data analysis
For the study, the researchers used data from the Health Professionals Follow-Up Study (HPFS) and the Nurses’ Health Studies (NHS). Both studies are ongoing and began in 1986 and 1976 to examine the effects of health and lifestyle on the incidence of serious illness in male and female healthcare professionals.
For the present study, the researchers included 62,225 females and 41,701 males who did not have a history of heart disease, stroke, or cancer.
The researchers examined their medical records for incidence of myocardial infarction and stroke, dietary surveys taken once every 4 years, and risk factors such as hypertension and type 2 diabetes from self-reports and physician diagnoses. Participants were tracked for 30 years.
By the end of the study period, the researchers noted 14,274 incident cases of CVD including 9,185 CHD events and 5,290 strokes.
The researchers noted that males and females with higher avocado intake tended to have higher total energy intake and a healthier diet with more fruits, vegetables, whole grains, nuts, and dairy products such as yogurt and cheese.
After adjusting for major dietary and lifestyle factors, the researchers found that having two or more servings of avocado per week was linked to a 16% lower CVD risk and 21% lower CHD risk compared to those who did not eat avocados.
They further found that replacing half a serving per day of mayonnaise, margarine, butter, egg, yogurt, cheese, or processed meats with the same amount of avocado was linked to a 19–31% lower risk of coronary heart disease.
They reported no significant association between stroke risk and avocado consumption. However, they noted that replacing half a serving per day of plant oils with an equivalent amount of avocado was linked to a 45% higher stroke risk.
Nutrient-rich food
When asked to explain what might account for the positive effects of avocado on CVD risk, study first author Lorena Pacheco, Ph.D., MPH, RDN, postdoctoral research fellow at Harvard T.H. Chan School of Public Health, told MNT:
“Avocados are a nutrient-rich food item with favorable food compounds including monounsaturated and polyunsaturated fats (healthy fats), vitamins, minerals, soluble fiber, vegetable proteins, phytosterols, and polyphenols. There are potential biological mechanisms by which avocados offer cardioprotective benefits.”
“The primary monounsaturated fatty acid present in avocados is oleic acid – healthy fat – and it is suggested that it helps in reducing hypertension, inflammation, and insulin sensitivity.”
“Additionally, they contain plant sterols that could have favorable effects on lipid profiles. [Also], the soluble fiber intake in avocados can also lead to a better lipid profile, meaning lower ‘bad cholesterol’ levels,” she explained.
“They also are a source of vegetable protein,” added Penny M. Kris-Etherton Ph.D., professor of nutritional science at Penn State College of Health and Human Development, not involved in the study. “Collectively, it is very likely that this ‘package’ of heart-health compounds accounts for the findings,” said Dr. Kris-Etherton.
The researchers concluded that replacing certain fat-containing foods with avocado could lower CVD risk.
Study limitations
The authors noted some limitations to their findings. As their study was observational, they could not establish causation.
Shannon Hoos-Thompson, MD, a cardiologist at The University of Kansas Health System, not involved in the study, explained for MNT:
“To put the findings in perspective, eating less cardiovascular unhealthy food may be the explanation [rather] than the result being specific to avocado consumption.”
The authors also noted that their study population was primarily non-Hispanic white nurses and health professionals, so their results may not be generalized to wider demographics.
“The dietary data were self-reported and have some measurement error,” added Dr. Kris-Etherton. “However, the authors used a repeated measurements dietary assessment method and collected intake data over time, which reduces random measurement error.”
Taking Care of Your Mental Health
Sadness, fear, worry, or other emotions can affect us during or after tough situations, like dealing with the COVID-19 pandemic, the loss of a family member or friend, or experiences related to racism. Dealing with these challenges can weigh heavily on your mental health, and recent data suggest this is the case for many who have sought professional help with their mental health since the pandemic started.
Increases in mental health-related ED visits
Recent research suggests that some racial and ethnic minority groups have been more affected by mental health challenges related to the pandemic. According to a new study published in JAMA Psychiatry, these groups had significant increases in emergency department (ED) visits for new and existing mental disorders during and after a COVID-19 case surge.
- Asian adults had increases in the number of visits for most of the mental disorders that the study looked at, including a 21% increase in ED visits with depression during a COVID-19 surge.
- American Indian and Alaska Native adults had increases in the number of ED visits for multiple mental disorders after a COVID-19 surge, including a 42% increase in trauma and stressor-related visits.
- There was a 24% increase in ED visits for bipolar disorder among Hispanic adults and a 14% increase in trauma and stressor disorder-related visits among Black adults after a surge.
Mental Health Impact of Stress
It’s natural to feel stress, anxiety, grief, and worry during challenging times. Feeling strong emotions or being stressed can have negative effects on your health. Stress can cause the following:
- Feelings of fear, anger, sadness, worry, numbness, or frustration.
- Changes in appetite, energy, desires, or interests.
- Problems concentrating or making decisions.
- Nightmares or problems sleeping.
- Physical reactions, such as headaches, body pains, stomach problems, or skin rashes.
- Worsening of chronic diseases and mental health conditions.
- Overeating or not eating enough.
- Increased use of alcohol, illegal drugs (like heroin, cocaine, methamphetamine), and misuse of prescription drugs (like opioids).
Healthy Ways to Cope with Stress
Learning to cope with stress in a healthy way will help you, the people you care about, and those around you become more resilient. You can help yourself, others, and your community manage stress in the following ways.
- Take breaks from news stories, including those on social media. It’s good to be informed, but constant discouraging information can be upsetting. Consider limiting news to just a couple of times a day and disconnecting from your phone, TV, and computer screens for a while.
Take care of your body:
- Get vaccinated and stay up to date on your COVID-19 vaccines.
- Eat plenty of fruits and vegetables, lean protein, whole grains, and fat-free or low-fat milk and dairy products. Eating well also means limiting saturated fats, cholesterol, salt, and added sugars.
- Going to bed at the same time each night and getting up at the same time each morning, including on the weekends, can help you sleep better (adults need 7 or more hours per night).
- Move more and sit less. Every little bit of physical activity helps. You can start small and build up to 150 minutes a week that can be broken down to smaller amounts such as 20 to 30 minutes a day.
- Take deep breaths, stretch, or meditate.
- Limit alcohol intake. Choose not to drink, or drink in moderation (one drink a day for women, two for men) on days that alcohol is consumed.
- Avoid using prescription drugs in ways other than prescribed, taking someone else’s prescription, or using illegal drugs. Treatment is available and recovery starts with asking for help.
- Avoid smoking and the use of other tobacco products. People can and do quit smoking for good.
- Continue with regular health appointments, testing, and screening, especially those for cancer.
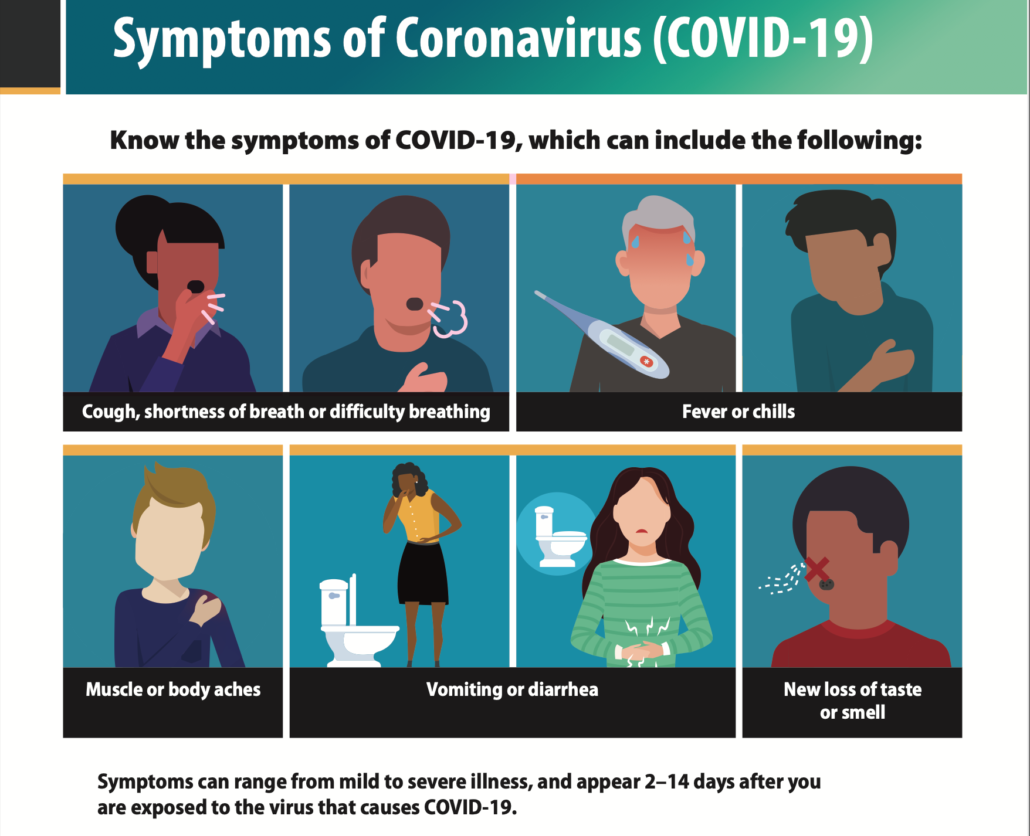
Watch for symptoms of COVID-19
People with COVID-19 have had a wide range of symptoms reported – ranging from mild symptoms to severe illness. Symptoms may appear 2-14 days after exposure to the virus. Anyone can have mild to severe symptoms. People with these symptoms may have COVID-19:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
This list does not include all possible symptoms. CDC will continue to update this list as we learn more about COVID-19. Older adults and people who have severe underlying medical conditions like heart or lung disease or diabetes seem to be at higher risk for developing more serious complications from COVID-19 illness.
When to Seek Emergency Medical Attention
Look for emergency warning signs* for COVID-19. If someone is showing any of these signs, seek emergency medical care immediately:
- Trouble breathing
- Persistent pain or pressure in the chest
- New confusion
- Inability to wake or stay awake
- Pale, gray, or blue-colored skin, lips, or nail beds, depending on skin tone
*This list is not all possible symptoms. Please call your medical provider for any other symptoms that are severe or concerning to you.
Call 911 or call ahead to your local emergency facility: Notify the operator that you are seeking care for someone who has or may have COVID-19.
If You Are Sick
- Check symptoms with Coronavirus Self-Checker
- Get tested
- What to do if you are sick
- Isolate if you are sick
- When to quarantine
- How to care for someone who is sick
Difference between COVID-19 & Flu
Influenza (Flu) and COVID-19 are both contagious respiratory illnesses, but they are caused by different viruses. COVID-19 is caused by infection with a new coronavirus (called SARS-CoV-2), and flu is caused by infection with influenza viruses.
COVID-19 seems to spread more easily than flu and causes more serious illnesses in some people. It can also take longer before people show symptoms and people can be contagious for longer. More information about differences between flu and COVID-19 is available in the different sections below.
Because some of the symptoms of flu and COVID-19 are similar, it may be hard to tell the difference between them based on symptoms alone, and testing may be needed to help confirm a diagnosis.
While more is learned every day about COVID-19 and the virus that causes it, there is still a lot that is unknown . This page compares COVID-19 and flu, given the best available information to date.
If you or your family member are at high risk for severe illness, wear a mask or respirator with greater protection in public indoor spaces if you are in an area with a high COVID-19 Community Level. Talk with your healthcare provider about wearing a mask in a medium COVID-19 Community Level.
If you test positive for COVID-19 and have one or more health conditions that increase your risk of becoming very sick, treatment may be available. Contact a health professional right away after a positive test to determine if you may be eligible, even if your symptoms are mild right now. Don’t delay: Treatment must be started within the first few days to be effective.
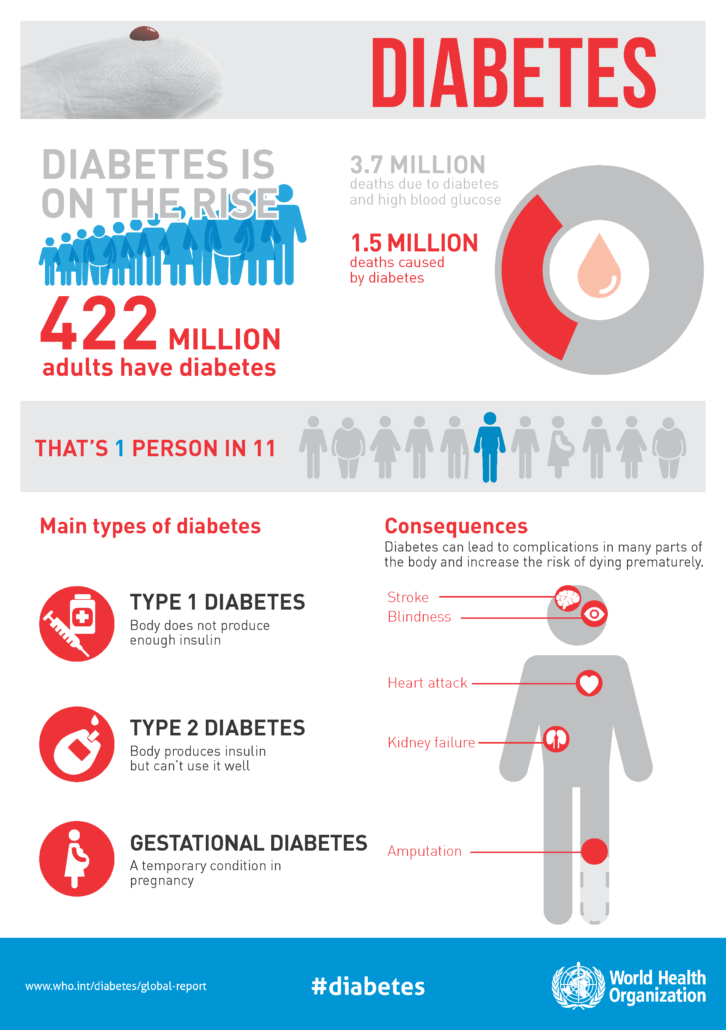
Type 2 Diabetes

More than 37 million Americans have diabetes (about 1 in 10), and approximately 90-95% of them have type 2 diabetes. Type 2 diabetes most often develops in people over age 45, but more and more children, teens, and young adults are also developing it.
Insulin is a hormone made by your pancreas that acts like a key to let blood sugar into the cells in your body for use as energy. If you have type 2 diabetes, cells don’t respond normally to insulin; this is called insulin resistance. Your pancreas makes more insulin to try to get cells to respond. Eventually your pancreas can’t keep up, and your blood sugar rises, setting the stage for prediabetes and type 2 diabetes. High blood sugar is damaging to the body and can cause other serious health problems, such as heart disease, vision loss, and kidney disease.
Symptoms and Risk Factors
Type 2 diabetes symptoms often develop over several years and can go on for a long time without being noticed (sometimes there aren’t any noticeable symptoms at all). Because symptoms can be hard to spot, it’s important to know the risk factors and to see your doctor to get your blood sugar tested if you have any of them.
Testing for Type 2 Diabetes
A simple blood test will let you know if you have diabetes. If you’ve gotten your blood sugar tested at a health fair or pharmacy, follow up at a clinic or doctor’s office to make sure the results are accurate.
Managing Diabetes
Unlike many health conditions, diabetes is managed mostly by you, with support from your health care team (including your primary care doctor, foot doctor, dentist, eye doctor, registered dietitian nutritionist, diabetes educator, and pharmacist), family, and other important people in your life. Managing diabetes can be challenging, but everything you do to improve your health is worth it!
You may be able to manage your diabetes with healthy eating and being active, or your doctor may prescribe insulin, other injectable medications, or oral diabetes medicines to help manage your blood sugar and avoid complications. You’ll still need to eat healthy and be active if you take insulin or other medicines. It’s also important to keep your blood pressure and cholesterol close to the targets your doctor sets for you and get necessary screening tests.
You’ll need to check your blood sugar regularly. Ask your doctor how often you should check it and what your target blood sugar levels should be. Keeping your blood sugar levels as close to target as possible will help you prevent or delay diabetes-related complications.
Stress is a part of life, but it can make managing diabetes harder, including managing your blood sugar levels and dealing with daily diabetes care. Regular physical activity, getting enough sleep, and relaxation exercises can help. Talk to your doctor and diabetes educator about these and other ways you can manage stress.
Make regular appointments with your health care team to be sure you’re on track with your treatment plan and to get help with new ideas and strategies if needed.
Whether you were just diagnosed with diabetes or have had it for some time, meeting with a diabetes educator is a great way to get support and guidance, including how to:
- Develop a healthy eating and activity plan
- Test your blood sugar and keep a record of the results
- Recognize the signs of high or low blood sugar and what to do about it
- If needed, give yourself insulin by syringe, pen, or pump
- Monitor your feet, skin, and eyes to catch problems early
- Buy diabetes supplies and store them properly
- Manage stress and deal with daily diabetes care
Ask your doctor about diabetes self-management education and support services and to recommend a diabetes educator, or search the Association of Diabetes Care & Education Specialists’ (ADCES) nationwide directory for a list of programs in your community.
Type 2 Diabetes in Children and Teens
Childhood obesity rates are rising, and so are the rates of type 2 diabetes in youth. More than 75% of children with type 2 diabetes have a close relative who has it, too. But it’s not always because family members are related; it can also be because they share certain habits that can increase their risk. Parents can help prevent or delay type 2 diabetes by developing a plan for the whole family:
- Drinking more water and fewer sugary drinks
- Eating more fruits and vegetables
- Making favorite foods healthier
- Making physical activity more fun
Healthy changes become habits more easily when everyone makes them together. Find out how to take charge family style with these healthy tips.
Get Support
Tap into online diabetes communities for encouragement, insights, and support. The American Diabetes Association’s Community page and ADCES’s Peer Support Resources are great ways to connect with others who share your experience.
Food Poisoning Symptoms
Food poisoning symptoms can be anywhere from mild to very serious. Your symptoms may be different depending on the germ you swallowed. The most common symptoms of food poisoning are:
- Upset stomach
- Stomach cramps
- Nausea
- Vomiting
- Diarrhea
- Fever
After you swallow an unsafe (contaminated) food or drink, it may take hours or days to develop symptoms. If you have symptoms of food poisoning, such as diarrhea or vomiting, drink plenty of fluids to prevent dehydration (not having enough water in your body).
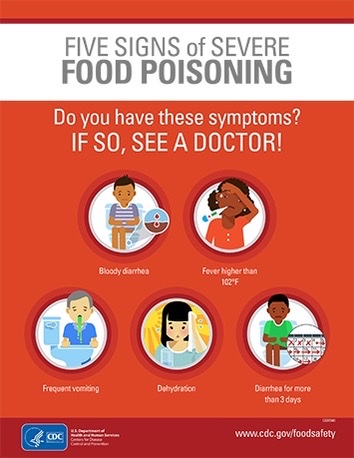
When to See a Doctor for Food Poisoning
See your doctor or healthcare provider if you have symptoms that are severe, including:
- Bloody diarrhea
- High fever (temperature over 102°F, measured in your mouth)
- Frequent vomiting that prevents keeping liquids down (which can lead to dehydration)
- Signs of dehydration, including little or no urination, a very dry mouth and throat, or feeling dizzy when standing up
- Diarrhea that lasts more than 3 days
Serious Health Problems and Long-Term Effects From Food Poisoning
Most people have only mild illnesses, lasting a few hours to several days. However, some people need to be hospitalized, and some illnesses cause long-term health problems or even death. Infections spread by food can lead to:
- Chronic arthritis
- Brain and nerve damage
- Kidney failure caused by hemolytic uremic syndrome (HUS)
Symptoms and Sources of Common Food Poisoning Germs
Some germs make you sick within a few hours after you swallow them. Others may take a few days to make you sick. This list provides the symptoms, when symptoms begin, and common food sources for germs that cause food poisoning. The germs are listed in order of how quickly symptoms begin.
- Symptoms begin 30 minutes to 8 hours after exposure: Nausea, vomiting, stomach cramps. Most people also have diarrhea. Common food sources: Foods that are not cooked after handling, such as sliced meats, puddings, pastries, and sandwiches
- Symptoms begin 2 to 48 hours after exposure: Watery diarrhea, nausea, stomach cramps, vomiting, fever, chills Common food sources: Raw or undercooked shellfish, particularly oysters
- Symptoms begin 6 to 24 hours after exposure: Diarrhea, stomach cramps. Usually begins suddenly and lasts for less than 24 hours. Vomiting and fever are not common. Common food sources: Beef or poultry, especially large roasts; gravies; dried or precooked foods
- Symptoms begin 6 hours to 6 days after exposure: Diarrhea, fever, stomach cramps, vomiting Common food sources: Raw or undercooked chicken, turkey, and meat; eggs; unpasteurized (raw) milk and juice; raw fruits and vegetables
- Other sources: Many animals, including backyard poultry, reptiles and amphibians, and rodents (pocket pets)
- Symptoms begin 12 to 48 hours after exposure: Diarrhea, nausea/stomach pain, vomiting Common food sources: Leafy greens, fresh fruits, shellfish (such as oysters), or unsafe water
- Other sources: Infected person; touching surfaces that have the virus on them
Clostridium botulinum (Botulism)
- Symptoms begin 18 to 36 hours after exposure: Double or blurred vision, drooping eyelids, slurred speech. Difficulty swallowing and breathing, dry mouth. Muscle weakness and paralysis. Symptoms start in the head and move down as the illness gets worse. Common food sources: Improperly canned or fermented foods, usually homemade. Prison-made illicit alcohol (pruno).
- Symptoms begin 2 to 5 days after exposure: Diarrhea (often bloody), stomach cramps/pain, fever Common food sources: Raw or undercooked poultry, raw (unpasteurized) milk, and contaminated water
- Symptoms begin 3 to 4 days after exposure: Severe stomach cramps, diarrhea (often bloody), and vomiting. Around 5–10% of people diagnosed with E. coli develop a life-threatening health problem. Common food sources: Raw or undercooked ground beef, raw (unpasteurized) milk and juice, raw vegetables (such as lettuce), raw sprouts, unsafe water
- Symptoms begin 1 week after exposure: Watery diarrhea, loss of appetite, and weight loss. Stomach cramps/pain, bloating, increased gas, nausea, and fatigue. Common food sources: Raw fruits or vegetables and herbs
- Symptoms begin 1 to 4 weeks after exposure: Pregnant women usually have a fever and other flu-like symptoms, such as fatigue and muscle aches. Infections during pregnancy can lead to serious illness or even death in newborns.
- Other people (most often older adults): headache, stiff neck, confusion, loss of balance, and convulsions in addition to fever and muscle aches. Common food sources: Queso fresco and other soft cheeses, raw sprouts, melons, hot dogs, pâtés, deli meats, smoked seafood, and raw (unpasteurized) milk