What to know about eczema
Eczema is a condition in which patches of skin become inflamed, itchy, cracked, and rough. Some types can also cause blisters.
Different types and stages of eczema affect 31.6 million people in the United States, which equals more than 10% of the population.
Many people use the word eczema when referring to atopic dermatitis, which is the most common type. The term atopic refers to a collection of conditions that involve the immune system, including atopic dermatitis, asthma, and hay fever. The word dermatitis refers to inflammation of the skin.
Certain foods, such as nuts and dairy, can trigger symptoms of eczema. Environmental triggers can include smoke, pollen, soaps, and fragrances. Eczema is not contagious.
About a quarter of children in the U.S. have the condition, as well as 10% of African Americans, 13% of Asian Americans and Pacific Islanders, 13% of Native Americans, and 11% of people who are white.
Some people outgrow the condition, while others will continue to have it throughout adulthood. This article will explain what eczema is and discuss its symptoms, treatments, causes, and types.
Symptoms
The symptoms of atopic dermatitis can vary depending on a person’s age and the condition’s severity and can vary by individual.
People with the condition will often experience periods of time when their symptoms worsen, followed by periods of time when their symptoms will improve or clear up.
The following sections will outline some of the potential differences in symptoms in more detail.
General eczema symptoms
In most cases eczema symptoms are mild. The most common symptoms of atopic dermatitis include:
- dry, scaly skin
- skin flushing
- itching
- open, crusted, or weeping sores
People with severe eczema may need more intensive treatment to relieve their symptoms. Continuous rubbing and scratching can also lead to skin infections.
Eczema symptoms in People of Color
In People of Color, an eczema rash may appear gray or brown. This can make outbreaks harder to see.
However, People of Color who get eczema may also get dark or light skin patches even after eczema symptoms go away. These can last a long time. Doctors call these patches hyperpigmentation and depigmentation or hypopigmentation.
A dermatologist can evaluate these patches, which may respond to treatments like steroid creams.
Infant eczema symptoms
The following atopic dermatitis symptoms are common in babies under the age of 2:
- rashes on the scalp and cheeks
- rashes that bubble up before leaking fluid
- rashes that can cause extreme itchiness, which may interfere with sleeping
Childhood eczema symptoms
The following atopic dermatitis symptoms are common in children age 2 and above:
- rashes that appear behind the creases of elbows or knees
- rashes that appear on the neck, wrists, ankles, and the crease between the buttocks and legs
- bumpy rashes
- rashes that can become lighter or darker
- skin thickening, also known as lichenification, which can then develop into a permanent itch
Most people with the condition develop it before the age of 5 years. An estimated 60% of children will no longer show symptoms by adolescence.
African American and Hispanic children may have more severe eczema than children who are white.
Symptoms in adults
The following atopic dermatitis symptoms are common in adults:
- rashes that are more scaly than those occurring in children
- rashes that commonly appear in the creases of the elbows or knees or the nape of the neck
- rashes that cover much of the body
- very dry skin on the affected areas
- rashes that are permanently itchy
- skin infections
Adults who developed atopic dermatitis as children but no longer experience the condition may still have dry or easily irritated skin, hand eczema, and eczema on the eyelids.
The appearance of skin affected by atopic dermatitis will depend on how much a person scratches and whether the skin is infected. Scratching and rubbing can further irritate the skin, increase inflammation, and make the itching worse.
Treatments
There is currently no cure for eczema. Treatment for the condition aims to heal the affected skin and prevent flares of symptoms.
Doctors will suggest a treatment plan based on an individual’s age, symptoms, and current state of health.
For some people, eczema goes away over time. For others, however, it is a lifelong condition.
The sections below will list some treatment options.
Home care
There are several things that people with eczema can do to support skin health and alleviate symptoms.
They can try:
- taking lukewarm baths
- applying moisturizer within 3 minutes of bathing to “lock in” moisture
- moisturizing every day
- wearing cotton and soft fabrics
- avoiding rough, scratchy fibers and tight fitting clothing
- using a humidifier in dry or cold weather
- using a mild soap or a non-soap cleanser when washing
- taking extra precautions to prevent eczema flares in winter
- air drying or gently patting the skin dry with a towel, rather than rubbing the skin dry after bathing or taking a shower
- where possible, avoiding rapid changes of temperature and activities that cause sweating
- learning and avoiding individual eczema triggers
- keeping fingernails short to prevent scratching from breaking the skin
People can also try various natural remedies for eczema, including aloe vera, coconut oil, and apple cider vinegar.
Medications
Doctors can prescribe several medications to treat the symptoms of eczema, including:
- Topical corticosteroid creams and ointments: These are anti-inflammatory medications and should relieve the main symptoms of eczema, such as inflammation and itchiness. People can apply them directly to the skin. Some people may benefit from prescription-strength medications.
- Oral medications: If topical treatments are not effective, a doctor may prescribe oral medications like systemic corticosteroids or immunosuppresants. These are available as injections or oral tablets. People should only use them for short periods of time. Also, it is important to note that the symptoms may worsen upon stopping these drugs if the person is not already taking another medication for the condition.
- Antibiotics: Doctors prescribe antibiotics if eczema occurs alongside a bacterial skin infection.
- Antihistamines: These can reduce the risk of nighttime scratching, as they tend to cause drowsiness.
- Topical calcineurin inhibitors: This drug suppresses the activities of the immune system. It decreases inflammation and helps prevent flares.
- Barrier repair moisturizers: These reduce water loss and work to repair the skin.
- Phototherapy: This involves exposure to UVA or UVB waves. This method can treat moderate dermatitis. A doctor will monitor the skin closely throughout the treatment.
- Injected biologic drugs: These medications block proteins in the immune system to limit immune system response.
Even though the condition itself is not currently curable, each person should consult with a doctor to get a tailored treatment plan.
Even after an area of skin has healed, it is important to keep looking after it, as it may easily become irritated again.
Causes
Researchers do not know the definitive cause of eczema, but many health professionals believe that it develops from a combination of genetic and environmental factors.
Children are more likely to develop eczema if a parent has it or another atopic condition. If both parents have an atopic condition, the risk is even higher.
Some environmental factors may also bring out the symptoms of eczema. These include:
- Irritants: These include soaps, detergents, shampoos, disinfectants, juices from fresh fruits, meats, and vegetables.
- Allergens: Dust mites, pets, pollens, and mold can all lead to eczema. This is known as allergic eczema.
- Microbes: These include bacteria such as Staphylococcus aureus, viruses, and certain fungi.
- Hot and cold temperatures: Very hot and very cold weather, high and low humidity, and perspiration from exercise can bring out eczema.
- Foods: Dairy products, eggs, nuts and seeds, soy products, and wheat can cause eczema flares.
- Stress: This is not a direct cause of eczema, but it can make the symptoms worse.
- Hormones: Females may experience increased eczema symptoms when their hormone levels are changing, such as during pregnancy and at certain points in the menstrual cycle.
Types
There are several types of eczema. Besides atopic dermatitis, other types include:
- Allergic contact dermatitis: This is a skin reaction that occurs following contact with a substance or allergen that the immune system recognizes as foreign.
- Dyshidrotic eczema: This refers to irritation of the skin on the palms of the hands and soles of the feet. It is characterized by blisters.
- Neurodermatitis: This leads to scaly patches of skin on the head, forearms, wrists, and lower legs. It occurs due to a localized itch, such as from an insect bite.
- Discoid eczema: Also known as nummular eczema, this type presents as circular patches of irritated skin that can be crusted, scaly, and itchy.
- Stasis dermatitis: This refers to skin irritation of the lower leg. It is usually related to circulatory problems.
Summary
Eczema is a common inflammatory skin condition. The most common type is called atopic dermatitis. Eczema is most common in children, but the majority of children will grow out of it by the time they reach adolescence.
Eczema can cause discomfort and can vary in severity. It can present differently depending on a person’s age. In people with darker skin tones, the symptoms may be harder to see.
Although there is currently no cure, people can treat and prevent eczema flares using home remedies, moisturizers, medications, and lifestyle changes.
Is fast food bad for you? All you need to know about its nutrition and impacts
The term “fast food” generally refers to food that people intend to consume quickly, either on- or off-site. There is plenty of well-researched evidence demonstrating the various negative health effects of eating and overeating fast food, in both the short- and long-term.
Many fast food establishments now list the number of calories each item contains. However, this is only part of the consideration of whether it is healthy or not.
Fast food is typically poor in terms of nutrition. According to a 2015 review, fast food tends to contain various substances that are generally unhealthy. It is high in sugar, salt, saturated or trans fats, and many processed preservatives and ingredients. It also lacks some beneficial nutrients.
However, not all fast food has negative impacts, and a person can make an informed choice by researching the nutritional content of particular fast food items. People can find this information on the websites of most major restaurants.
That said, even the more healthy fast food items are generally high in sugar, salt, saturated fats, and trans fats. The Office of Disease Prevention and Health Promotion
notes that the typical person in the United States consumes too much of these food components.
Short-term impacts
Fast food is typically high in sugar, salt, and saturated or trans fats. The body’s reaction to these nutrients results in a range of short-term impacts when a person eats fast food.
Spike in blood sugar
Fast food breaks down quickly, causing a rapid spike in blood sugar because of the refined carbohydrates and added sugar. In turn, this causes an abnormally large insulin surge, resulting in a drop in blood sugar. This can cause people to feel tired. Insulin promotes further hunger within a short time after the meal.
Blood pressure
A small 2016 study found that consuming high levels of salt could immediately impact the proper functioning of a person’s blood vessels. Excess sodium intake also has links to fluid retention.
Increased inflammation
A single serving of fast food could increase inflammation throughout the body. A 2015 study found that one fast food meal high in saturated fat increased airway inflammation in individuals with asthma. This inflammation acts as a trigger for asthma attacks.
Affects nutrient intake
Fast food does not typically contain fresh fruit and vegetables. If an individual eats fast food frequently, they may find it challenging to reach their recommended daily intake of at least 5 servings of fruit and vegetables. They may also have difficulties reaching their ideal fiber intake, which according to the Food and Drug Administration is 28 grams per day.
Binge eating
Fast food is highly palatable, meaning the body breaks it down quickly in the mouth, and it does not need much chewing. Therefore, it activates the reward centers in the brain rapidly.
This combination trains the palate to prefer these highly processed, highly stimulating foods and reduces someone’s desire for whole, fresh foods.
Research from 2018 and other previous studies have suggested a link between fast food consumption and the incidence of food addiction for these low-nutrient items.
A small 2017 study of 15 adults found that a single day of high-fat overeating damaged insulin sensitivity. This can then trigger a cycle of binge eating or binge eating disorders.
Long-term impacts
There is plenty of well-researched evidence showing that regularly eating fast food can harm a person’s health.
A 2015 study identified the sometimes irreparable effects of eating fast food. Such risks include obesity, insulin resistance, type 2 diabetes, and various cardiovascular conditions.
This is because most fast food is high in sugar, salt, saturated fat, trans fats, processed ingredients, and calories. It is also generally low in antioxidants, fiber, and many other nutrients.
Digestive system
Many fast food meals are extremely low in fiber. Doctors associate low-fiber diets with a higher risk of digestive conditions such as constipation and diverticular disease, as well as reductions in healthy gut bacteria.
Immunity and inflammation
A 2019 review examined the effects of a Western diet on a person’s immune system. This diet consists of high amounts of sugar, salt, and saturated fat from only a few sources.
The authors noted that a Western diet could lead to higher inflammation, lower control of infection, higher cancer rates, and a higher risk of allergic and autoinflammatory disease.
Memory and learning
A 2020 paper suggests a link between unbalanced diets high in saturated fat and simple carbohydrates, typical of fast food, and a lower capacity for memory and learning. This sort of diet may also raise the risk of Alzheimer’s disease and Parkinson’s disease.
Allergies
In a 2018 review, the authors established a link between fast food consumption and an increase in asthma, rhinoconjunctivitis, and eczema.
Heart disease
The FDA suggests that a diet high in salt often increases a person’s blood pressure, making a person more prone to heart attacks, stroke, kidney disease, or heart disease.
The FDA also notes that a diet high in trans fats raises the amount of low-density lipoprotein or “bad” cholesterol and lowers the amount of high-density lipoprotein or “good” cholesterol. This means that a person is more likely to develop heart disease.
Obesity
The United States Department of Agriculture points out that typical fast food contains a very high number of calories. If a person eats more calories than they burn each day, they gain weight, which may lead to obesity.
According to the Centers for Disease Control and Prevention (CDC), obesity increases a person’s risk of developing a range of serious health conditions.
Education
Another consequence of younger people regularly eating fast food is their unintentional lack of understanding of basic meal preparation, cooking, and healthy eating.
Over time, this perpetuates dependence on fast food, and people may not learn how to prepare healthy, balanced food in the home. Consuming healthy meals can support a person’s long-term health throughout their lifespan.
Mental health impact
Eating lots of fast food could also impact an individual’s mental health and make them more prone to depression and anxiety.
A 2021 study compared data from 322 males and 322 females age 30 or older. They found an association between healthy food such as leafy greens, nuts, and fish and positive mood, while the opposite was true of fast food. In addition, women reported significantly more negative associations with fast food than men.
Summary
Fast food tends to be high in salt, sugar, saturated fats, trans fats, calories, and processed preservatives and ingredients. A wealth of well-conducted research has proven the negative health effects of consuming too much of these food components.
In the short term, fast food impacts blood sugar and blood pressure, increases inflammation, and may mean an individual does not eat enough necessary nutrients. In the long term, a diet rich in fast food could lead to issues with digestion, immunity, inflammation, heart health, obesity, and more.
Not all fast food is bad, however. Certain menu items might be lower in these substances than others, while some fast food outlets might focus on providing more healthy options.
To preserve health, a person should try to identify fast food items that contain less salt, fat, sugar, and total carbohydrates, and generally try to limit the amount of fast food they consume.
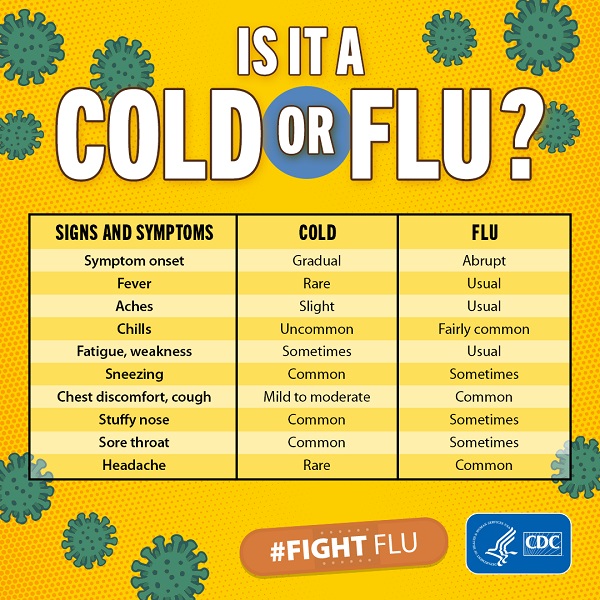
Cold Versus Flu
What is the difference between a cold and flu?
Influenza (flu) and the common cold are both contagious respiratory illnesses, but they are caused by different viruses. Flu is caused by influenza viruses only, whereas the common cold can be caused by a number of different viruses, including rhinoviruses, parainfluenza, and seasonal coronaviruses. Seasonal coronaviruses should not be confused with SARS-COV-2, the virus that causes COVID-19. Because flu and the common cold have similar symptoms, it can be difficult to tell the difference between them based on symptoms alone. In general, flu is worse than the common cold, and symptoms are typically more intense and begin more abruptly. Colds are usually milder than flu. People with colds are more likely to have a runny or stuffy nose than people who have flu. Colds generally do not result in serious health problems, such as pneumonia, bacterial infections, or hospitalizations. Flu can have serious associated complications.
How can you tell the difference between a cold and flu?

Because colds and flu share many symptoms, it can be difficult (or even impossible) to tell the difference between them based on symptoms alone. Special tests can tell if a person is sick with flu.
What are the symptoms of flu versus the symptoms of a cold?
The symptoms of flu can include fever or feeling feverish/chills, cough, sore throat, runny or stuffy nose, muscle or body aches, headaches, and fatigue (tiredness). Cold symptoms are usually milder than the symptoms of flu. People with colds are more likely to have a runny or stuffy nose. Colds generally do not result in serious health problems.
Back pain and remedies
Back pain is a common reason for absence from work and for seeking medical treatment. It can be uncomfortable and sometimes even debilitating.
Back pain can result from injury, activity, and some medical conditions. It can affect people of any age and for different reasons. As people get older, the likelihood of developing lower back pain increases due to factors such as previous occupation and degenerative disk disease.
Lower back pain may be relating to the bony lumbar spine, disks between the vertebrae, ligaments around the spine and disks, spinal cord and nerves, lower back muscles, abdominal and pelvic internal organs, or the skin around the lumbar area.
Pain in the upper back may be due to disorders of the aorta, tumors in the chest, or spine inflammation.
Causes
The human back consists of a complex structure of muscles, ligaments, tendons, disks, and bones that work together to support the body and enable movement.
The segments of the spine are cushioned with cartilage-like pads called disks.
Problems with any of these components can lead to back pain. In some cases of back pain, however, the cause remains unclear.
Damage can result from strain, medical conditions, or poor posture, among other things.
Back pain commonly stems from strain, tension, or injury. Frequent causes of back pain are:
- strained muscles or ligaments
- a muscle spasm
- muscle tension
- damaged disks
- injuries, fractures, or falls
Strain
Activities that can lead to strains or spasms include:
- lifting something improperly
- lifting something that is too heavy
- making an abrupt, awkward movement
Structural problems
A number of structural problems may also result in back pain:
- Ruptured disks: Each vertebra in the spine is cushioned by disks. If the disk ruptures, there will be more pressure on a nerve, resulting in back pain.
- Bulging disks: Much in the same way as ruptured disks, a bulging disk can lead to more pressure on a nerve.
- Sciatica: A sharp and shooting pain travels through the buttock and down the back of the leg. This may occur when a bulging or herniated disk presses on a nerve or when a muscle pushes specifically on the sciatic nerve.
- Arthritis: Osteoarthritis can cause problems with the joints in the hips, lower back, and other areas in the body. In some cases, the space around the spinal cord narrows. Health experts call this spinal stenosis.
- Unusual curvature of the spine: If the spine curves in an unusual way, back pain can occur. An example of this is scoliosis, in which the spine curves to the side.
- Osteoporosis: Bones, including the vertebrae of the spine, become brittle and porous, making compression fractures more likely.
- Kidney problems: Kidney stones or kidney infection can cause back pain.
Movement and posture
Adopting a hunched sitting position when using a computer can lead to increased back and shoulder problems over time.
Back pain can also result from some everyday activities or poor posture.
Examples include:
- twisting
- coughing or sneezing
- overstretching
- bending awkwardly or for long periods
- pushing, pulling, lifting, or carrying something
- standing or sitting for long periods
- straining the neck forward, such as when driving or using a computer
- driving for lengthy periods without taking a break, even when not hunched
- sleeping on a mattress that does not support the body or keep the spine straight
Other causes
Some medical conditions can lead to back pain:
- Cauda equina syndrome: The cauda equina is a bundle of spinal nerve roots that arise from the lower end of the spinal cord. Symptoms of this syndrome include a dull pain in the lower back and upper buttocks, as well as numbness in the buttocks, genitalia, and thighs. Sometimes, bowel and bladder function disturbances occur.
- Cancer of the spine: A tumor on the spine may press against a nerve, resulting in back pain. The structural damage to the bone itself can also be painful when there are tumors or metastasis to the bone.
- Infection of the spine: A fever and a tender, warm area on the back could be due to an infection of the spine.
- Other infections: Pelvic inflammatory disease and kidney or bladder infection may also lead to back pain.
- Sleep disorders: Individuals with sleep disorders are more likely to experience back pain than others.
- Shingles: An infection that can affect the nerves may lead to back pain. This depends on which nerves have become affected. A rash will follow the back pain.
Symptoms
The main symptom of back pain is an ache anywhere in the back and sometimes all the way down to the buttocks and legs.
Some back issues can cause pain in other parts of the body, depending on the nerves affected.
The pain often goes away without treatment. However, if it occurs with any of the following, a person should contact a doctor:
- unexplained weight loss
- fever
- inflammation or swelling on the back
- persistent back pain where lying down or resting does not help
- pain down the legs
- pain that reaches below the knees
- a recent injury, blow, or trauma to the back
- urinary incontinence
- difficulty urinating
- fecal incontinence, or loss of control over bowel movements
- numbness around the genitals
- numbness around the anus
- numbness around the buttocks
When to contact a specialist
A person should seek medical help if they experience any numbness or tingling or if they have back pain:
- that does not improve with rest
- after an injury or fall
- with numbness in the legs
- with weakness
- with fever
- with unexplained weight loss
Treatment
Back pain usually resolves with rest and home remedies, but sometimes, medical treatment is necessary.
Home treatments
Over-the-counter (OTC) pain relief medication — usually, nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen — can relieve discomfort. Applying a hot compress or an ice pack to the painful area may also reduce pain.
Resting from strenuous activity can help, but moving around will ease stiffness, alleviate pain, and prevent muscles from weakening.
Medical treatment
If home treatments do not relieve back pain, a doctor may recommend the following medication, physical therapy, or both:
Medication
Back pain that does not respond well to OTC pain relief medication may require a prescription NSAID.
Codeine or hydrocodone, which are narcotics, may be prescribed for short periods. These require close monitoring by a doctor. In some cases, doctors may also recommend muscle relaxants.
Antidepressants, such as amitriptyline, may be prescribed, but research into their effectiveness is ongoing, and the existing evidence is conflicting.
Physical therapy
Applying heat, ice, ultrasound, and electrical stimulation, as well as some muscle release techniques, to the back muscles and soft tissues may help alleviate pain.
As the pain improves, a physical therapist may introduce some flexibility and strength exercises for the back and abdominal muscles. Techniques for improving posture may also help.
It is advisable to practice the techniques regularly, even after the pain has gone, to prevent back pain recurrence.
Cortisone injections
If other options are not effective, these may be injected into the epidural space, around the spinal cord.
Cortisone is an anti-inflammatory drug. It helps reduce inflammation around the nerve roots. Injections may also be used to numb areas thought to be causing the pain.
Botox
According to research, botox reduces pain by paralyzing sprained muscles in spasm. These injections are effective for about 3–4 months.
Traction
Pulleys and weights are used to stretch the back. This may result in a herniated disk moving back into position. It can also relieve pain but only while traction is applied.
Cognitive behavioral therapy
Cognitive behavioral therapy (CBT) can help manage chronic back pain by encouraging new ways of thinking. It may include relaxation techniques and ways of maintaining a positive attitude.
Studies have found that people receiving CBT tend to become more active and do exercise, which lowers the risk of back pain recurrence.
Surgery
Surgery for back pain is very rare. If an individual has a herniated disk, surgery may be an option, especially if there is persistent pain and nerve compression, which can lead to muscle weakness.
Examples of surgical procedures include:
- Fusion: A surgeon joins two vertebrae and inserts a bone graft between them. The vertebrae are splinted together with metal plates, screws, or cages. There is a significantly greater risk of arthritis to subsequently develop in the adjoining vertebrae.
- Artificial disk: A surgeon inserts an artificial disk that replaces the cushion between two vertebrae.
- Diskectomy: Surgeons may remove a portion of a disk if it is irritating or pressing against a nerve.
- Partially removing a vertebra: A surgeon may remove a small section of a vertebra if it is pinching the spinal cord or nerves.
Injecting cells to regenerate spinal disks: Scientists from Duke University in Durham, NC, developed new biomaterials that can deliver a booster shot of reparative cells to the nucleus pulposus, effectively eliminating pain resulting from degenerative disk disease.
Complementary therapies
Complementary therapies may be used alongside conventional therapies or on their own.
Chiropractic, osteopathy, shiatsu, and acupuncture may help relieve back pain and encourage a person to feel relaxed.
- An osteopath is a physician who specializes in treating the skeleton and muscles.
- A chiropractor treats joint, muscle, and bone problems. The main focus is the spine.
- Shiatsu, or finger pressure therapy, is a type of massage where pressure is applied along energy lines in the body. The shiatsu therapist applies pressure with the fingers, thumbs, and elbows.
- Acupuncture, which originated in China, involves inserting fine needles into specific points in the body. Acupuncture can help the body release its natural pain relievers — endorphins — and stimulate nerve and muscle tissue.
- Yoga involves specific physical poses, movements, and breathing exercises. Some of these may help strengthen the back muscles and improve posture. Care must be taken that exercises do not make back pain worse.
Studies on complementary therapies have given mixed results. Some people have experienced significant benefits, while others have not. When considering alternative therapies, it is important to seek guidance from a qualified and registered therapist.
Transcutaneous electrical nerve stimulation (TENS) is a popular therapy for individuals with chronic back pain. The TENS machine delivers small electric pulses into the body through electrodes placed on the skin.
Experts believe TENS encourages the body to produce endorphins and may block pain signals returning to the brain. Studies on TENS have provided mixed results. Some showed no benefits, while others indicate that it could be helpful for some people.
A TENS machine should be used under the direction of a healthcare professional.
A person should avoid TENS if they:
- are pregnant
- have a history of epilepsy
- have a pacemaker
TENS is considered “safe, noninvasive, inexpensive, and patient friendly,” and it appears to reduce pain. However, more evidence is necessary to confirm its effectiveness in improving activity levels.
Risk factors
The following factors are linked to a higher risk of developing low back pain:
- occupational activities
- pregnancy
- a sedentary lifestyle
- not enough exercise
- older age
- obesity
- smoking
- strenuous physical exercise or work, especially if done incorrectly
- genetic factors
- medical conditions, such as arthritis and cancer
Lower back pain also tends to be more common in females than in males, possibly due to hormonal factors. Additionally, health experts associate back pain with stress, anxiety, and mood disorders.
Diagnosis
A doctor will usually be able to diagnose back pain after asking about symptoms and carrying out a physical examination.
An imaging scan and other tests may be necessary if:
- back pain appears to result from an injury
- there is an underlying cause that requires treatment
- the pain persists over a long period
An X-ray, an MRI scan, or a CT scan can give information about the state of the soft tissues in the back:
- X-rays can show the alignment of the bones and reveal signs of arthritis or broken bones, but they cannot reveal damage in the muscles, spinal cord, nerves, or disks.
- MRI or CT scans can reveal herniated disks or problems with tissue, tendons, nerves, ligaments, blood vessels, muscles, and bones.
- Bone scans can detect bone tumors or compression fractures resulting from osteoporosis. A radioactive substance, or tracer, is injected into a vein. The tracer collects in the bones and helps the doctor detect bone problems with the aid of a special camera. Doctors use these for bone conditions and difficult-to-detect fractures.
- Electromyography measures the electrical impulses produced by nerves in response to muscles. This can confirm nerve compression, which may occur with a herniated disk or spinal stenosis.
A doctor may also order a blood test if they suspect an infection.
Other types of diagnosis
- A chiropractor will diagnose through touch, or palpation, and a visual examination. Chiropractic is known as a direct approach, with a strong focus on adjusting the spinal joints. A chiropractor may also want to see the results of imaging scans and any blood and urine tests.
- An osteopath also diagnoses through palpation and visual inspection. Osteopathy involves slow and rhythmic stretching, known as mobilization, pressure or indirect techniques, and manipulation of joints and muscles.
- A physical therapist focuses on diagnosing problems in the joints and soft tissues of the body.
Chronic or acute pain?
Health experts distinguish two types of back pain: acute and chronic.
Acute pain starts suddenly and lasts for up to 6 weeks.
Chronic, or long-term, pain develops over a longer period, lasts for over 3 months, and causes ongoing problems.
If a person has both occasional bouts of more intense pain and fairly continuous mild back pain, it can be hard for a doctor to determine whether they have acute or chronic back pain.
Prevention
Steps to lower the risk of developing back pain consist mainly of addressing some of the risk factors.
Exercise
Regular exercise helps build strength and manage body weight. Guided, low impact aerobic activities can boost heart health without straining or jerking the back.
Before starting any exercise program, a person should consult a healthcare professional.
There are two main types of exercise that people can do to reduce the risk of back pain:
- Core-strengthening exercises work the abdominal and back muscles, helping strengthen muscles that protect the back.
- Flexibility training aims at improving core flexibility, including the spine, hips, and upper legs.
Diet
A person’s diet should include sufficient amounts of calcium and vitamin D, as these are crucial for bone health.
A balanced diet also helps manage body weight.
Smoking
A significantly higher percentage of people who smoke have back pain incidences, compared with individuals who do not smoke and who are of the same age, height, and weight.
Body weight
The weight people carry and where they carry it affects the risk of developing back pain.
People with obesity are at considerably higher risk of experiencing back pain than those with a moderate body weight.
Moreover, people who carry excessive weight in the abdominal area rather than in the buttocks and hip area are also at greater risk.
Posture when standing
Make sure you have a neutral pelvic position. Stand upright, with the head facing forward and a straight back, and balance your weight evenly on both feet. Keep your legs straight and your neck in line with the rest of the spine.
Posture when sitting
A good seat for working should have good back support, arm rests, and a swivel base.
When sitting, try to keep your knees and hips level and keep your feet flat on the floor or use a footstool. You should be able to sit upright with support in the small of your back.
If you are using a keyboard, make sure that there is a 90-degree angle between the upper arm and forearm.
Lifting
When lifting things, use your legs, not your back, to do the lifting.
Maintain a long spine and keep your feet apart, with one leg slightly forward so that you can maintain balance. Bend only at the knees, hold the weight close to your body, and straighten the legs while changing the position of your back as little as possible.
Bending your back initially is unavoidable, but when you bend your back, try not to stoop and be sure to draw your low belly in so that your pelvis stays neutral and supported. Most importantly, do not straighten your legs before lifting, or you will be using your back for most of the work.
Avoid lifting and twisting at the same time
If something is particularly heavy, see whether you can lift it with someone else. While you are lifting it, keep looking straight ahead, not up or down, so that the neck is in alignment with the rest of the spine.
Moving things
It is safer for the back to push, not pull, things across the floor, as that way, you will be using your leg strength.
Shoes
Shoes with a low heel place less of a strain on the back. However, some flat shoes with minimal support, such as flip-flops, can also contribute to back pain.
Driving
It is important to have proper support for your back when driving.
Make sure the wing mirrors are properly positioned so that you do not need to twist. The pedals should be squarely in front of your feet.
If you are driving for a long time, have many breaks. Get out of the car and walk around.
Bed
You should use a mattress that keeps the spine properly aligned and supports the weight of the shoulders and buttocks. Also, use a pillow that does not force your neck into a steep angle.
What to know about cancer
Cancer causes cells to divide uncontrollably. This can result in tumors, damage to the immune system, and other impairment that can be fatal.
In the United States, an estimated 15.5 million people with a history of cancer were living as of January 1, 2016, according to a 2018 report from the American Cancer Society.
In this article, we examine types of cancer, how the disease develops, and the many treatments that help improve the quality of life and survival rates.
What is cancer?
Cancer is a broad term. It describes the disease that results when cellular changes cause the uncontrolled growth and division of cells.
Some types of cancer cause rapid cell growth, while others cause cells to grow and divide at a slower rate.
Certain forms of cancer result in visible growths called tumors, while others, such as leukemia, do not.
Most of the body’s cells have specific functions and fixed lifespans. While it may sound like a bad thing, cell death is part of a natural and beneficial phenomenon called apoptosis.
A cell receives instructions to die so that the body can replace it with a newer cell that functions better. Cancerous cells lack the components that instruct them to stop dividing and to die.
As a result, they build up in the body, using oxygen and nutrients that would usually nourish other cells. Cancerous cells can form tumors, impair the immune system and cause other changes that prevent the body from functioning regularly.
Cancerous cells may appear in one area, then spread via the lymph nodes. These are clusters of immune cells located throughout the body.
Causes
There are many causes of cancer, and some are preventable.
For example, over 480,000 peopleTrusted Source die in the U.S. each year from smoking cigarettes, according to data reported in 2014.
In addition to smoking, risk factors for cancer include:
- heavy alcohol consumption
- excess body weight
- physical inactivity
- poor nutrition
Other causes of cancer are not preventable. Currently, the most significant unpreventable risk factor is age. According to the American Cancer Society, doctors in the U.S. diagnose 87 percent of cancer cases in people ages 50 years or older.
Is cancer genetic?
Genetic factors can contribute to the development of cancer.
A person’s genetic code tells their cells when to divide and expire. Changes in the genes can lead to faulty instructions, and cancer can result.
Genes also influence the cells’ production of proteins, and proteins carry many of the instructions for cellular growth and division.
Some genes change proteins that would usually repair damaged cells. This can lead to cancer. If a parent has these genes, they may pass on the altered instructions to their offspring.
Some genetic changes occur after birth, and factors such as smoking and sun exposure can increase the risk.
Other changes that can result in cancer take place in the chemical signals that determine how the body deploys, or “expresses” specific genes.
Finally, a person can inherit a predisposition for a type of cancer. A doctor may refer to this as having a hereditary cancer syndrome. Inherited genetic mutations significantly contribute to the development of 5–10 percent of cancer cases.
Treatments
The side effects of chemotherapy include hair loss. However, advances in treatment are improving the outlook for people with cancer.
Innovative research has fueled the development of new medications and treatment technologies.
Doctors usually prescribe treatments based on the type of cancer, its stage at diagnosis, and the person’s overall health.
Below are examples of approaches to cancer treatment:
- Chemotherapy aims to kill cancerous cells with medications that target rapidly dividing cells. The drugs can also help shrink tumors, but the side effects can be severe.
- Hormone therapy involves taking medications that change how certain hormones work or interfere with the body’s ability to produce them. When hormones play a significant role, as with prostate and breast cancers, this is a common approach.
- Immunotherapy uses medications and other treatments to boost the immune system and encourage it to fight cancerous cells. Two examples of these treatments are checkpoint inhibitors and adoptive cell transfer.
- Precision medicine, or personalized medicine, is a newer, developing approach. It involves using genetic testing to determine the best treatments for a person’s particular presentation of cancer. Researchers have yet to show that it can effectively treat all types of cancer, however.
- Radiation therapy uses high-dose radiation to kill cancerous cells. Also, a doctor may recommend using radiation to shrink a tumor before surgery or reduce tumor-related symptoms.
- Stem cell transplant can be especially beneficial for people with blood-related cancers, such as leukemia or lymphoma. It involves removing cells, such as red or white blood cells, that chemotherapy or radiation has destroyed. Lab technicians then strengthen the cells and put them back into the body.
- Surgery is often a part of a treatment plan when a person has a cancerous tumor. Also, a surgeon may remove lymph nodes to reduce or prevent the disease’s spread.
- Targeted therapies perform functions within cancerous cells to prevent them from multiplying. They can also boost the immune system. Two examples of these therapies are small-molecule drugs and monoclonal antibodies.
Doctors will often employ more than one type of treatment to maximize effectiveness.
Types
The most common type of cancer in the U.S. is breast cancer, followed by lung and prostate cancers, according to the National Cancer Institute, which excluded nonmelanoma skin cancers from these findings.
Each year, more than 40,000 people in the country receive a diagnosis of one of the following types of cancer:
- bladder
- colon and rectal
- endometrial
- kidney
- leukemia
- liver
- melanoma
- non-Hodgkin’s lymphoma
- pancreatic
- thyroid
Other forms are less common. According to the National Cancer Institute, there are over 100 types of cancer.
Cancer development and cell division
Doctors classify cancer by:
- its location in the body
- the tissues that it forms in
For example, sarcomas develop in bones or soft tissues, while carcinomas form in cells that cover internal or external surfaces in the body. Basal cell carcinomas develop in the skin, while adenocarcinomas can form in the breast.
When cancerous cells spread to other parts of the body, the medical term for this is metastasis.
A person can also have more than one type of cancer at a time.
Outlook
Improvements in cancer detection, increased awareness of the risks of smoking, and a drop in tobacco use have all contributed to a year-on-year decrease in the number of cancer diagnoses and deaths.
According to the American Cancer Society, the overall cancer death rate declined by 26 percent between 1991 and 2015.
When a person has cancer, the outlook will depend on whether the disease has spread and on its type, severity, and location.
Takeaway
Cancer causes cells to divide uncontrollably. It also prevents them from dying at the natural point in their life cycle.
Genetic factors and lifestyle choices, such as smoking, can contribute to the development of the disease. Several elements affect the ways that DNA communicates with cells and directs their division and death.
After nonmelanoma skin cancer, breast cancer is the most common type in the U.S. However, lung cancer is the leading cause of cancer-related death.
Treatments are constantly improving. Examples of current methods include chemotherapy, radiation therapy, and surgery. Some people benefit from newer options, such as stem cell transplantation and precision medicine.
The diagnosis and death rates of cancer are dropping yearly.
COVID-19 vaccines for children: What are the side effects?
Vaccines undergo particularly rigorous safety tests before receiving approval for use in the general population. However, no drug is guaranteed to be free from side effects, so what are the side effects that children receiving the COVID-19 vaccine may face?
The Food and Drug Administration (FDA) approved the Pfizer vaccine for children aged 5–11 years on October 29, 2021. According to a recent survey by KFF COVID-19 Vaccine Monitor, just over one-quarter of parents of children in this age group are eager for their child to be vaccinated as soon as possible.
Although this may be surprising, other survey findings shed some light on the reasons behind this hesitancy: a fear of side effects.
Two-thirds of parents of children of this age said that they were worried that the COVID-19 vaccine would affect their children’s future fertility. So significant are these concerns that the American Academy of Pediatrics recently put out a video disputing any potential impact of the vaccine on puberty or fertility.
Vaccine hesitancy is not just over fears of an impact on fertility, however. Over three-quarters of parents reported that they were “very” or “somewhat” concerned that their child might experience serious side effects or that not enough is known about long-term effects from the COVID-19 vaccine.
So, what are the possible side effects?
What are children going to get?
In the same way that pharmaceutical companies raced to get the vaccine approved for adults, those companies have carried out trials to see if their vaccines are safe and effective in adolescents and children.
Speaking at an Independent SAGE briefing on November 5, 2021, Prof. Deenan Pillay — a professor of virology at University College London (UCL) in the United Kingdom — said:
“There have been a number of trials. We are always concerned about the untoward effect of all medicines in children, and, of course, we can’t just extrapolate from data that [come] from adults to children. We have got to wait to ensure there is safety in children. And now that has happened.”
So far, mRNA vaccines from Pfizer and Moderna have received approval in the U.S. for children over 12 years of age, with the Pfizer vaccine approved for 5–12-year-olds at the end of October 2021.
The European Medicines Agency announced that it would start investigating the safety of the vaccine in that age group on October 18, 2021.
Most countries offering vaccination to those over 12 years of age are offering the Pfizer or Moderna vaccine, Reuters recently reported. A single dose of the Pfizer vaccine is available for those over 12 years old in the U.K., where the Moderna vaccine also has approval for this age group.
Pfizer has plans to trial the vaccine in children aged 6 months to 5 years, and Moderna has ongoing trials to test the safety and efficacy of vaccines in children under 12 years old.
Novavax is about to start a study of up to 3,000 adolescents aged 12–17 years across up to 75 sites in the United States. Johnson & Johnson has enrolled children as young as 12 years into existing trials, and AstraZeneca is planning on conducting trials of its vaccine in children as young as 6 years.
The vaccine with the most evidence to support its use so far is Pfizer’s mRNA vaccine against SARS-CoV-2, which is the virus that causes COVID-19.
However, the vaccine doses given to children over the age of 12 years and those under the age of 12 years differ. Pfizer released data from its phase 2 and 3 trials at the end of September 2021. The data suggest that the vaccine was safe in children aged 5–11 years.
Children under the age of 12 years will be offered 10 micrograms (mcg) of the vaccine. This is compared with 30 mcg of the vaccine, which is the amount given to children over the age of 12 years and adults. Experts hope that this lower dose could result in fewer side effects, as lower doses generally should.
Minor adverse reactions
Senior vice president of Pfizer Vaccine Clinical Research and Development, Dr. Bill Gruber, broke down the drug company’s data from its phase 2 and 3 trials at the FDA’s Vaccines and Related Biological Products Advisory Committee Meeting on October 26, 2021.
He revealed that there were very few serious adverse events and no deaths during the phase 2 and 3 trials of children aged 5–12 years. He also explained that the side effects were similar to those that adults experience.
The most common side effects in children after their second dose of the vaccine — first dose reactions were less frequent — were fatigue and headache, with 39.4% and 28% of 5–12-year-olds experiencing those symptoms, respectively.
This is compared with 65.6% and 60.9% of adults. Of note were data showing that fever and chills experienced after the vaccine were lower among 5–12-year-olds than among 12–65-year-olds.
Just 6.5% of children aged 5–12 years experienced fever after vaccination, compared with 17.2% of those over 12 years. Also, just 9.8% of those aged 5–12 years experienced chills, compared with 40% of those over 12 years.
Due to existing concerns about the risk of myocarditis and pericarditis among adolescent and young adult males, the scientists took specific precautions during this trial, Dr. Gruber explained to the committee.
He said: “To enhance possible detection of the rare events of myocarditis in adolescents and young adults, should [they] occur, specific instructions were provided to be vigilant with symptoms and signs of myocarditis […]. No anaphylaxis, no myocarditis, and no appendicitis were reported.”
Myocarditis
The Centers for Disease Control and Prevention (CDC) and others are currently monitoring rates of myocarditis, which is inflammation of the heart muscle. This comes following reports in July 2021 that some teenage boys had received diagnoses of this condition after receiving the Pfizer vaccine, which those over 12 years of age have been able to receive since May 2021.
The CDC reports that males aged 12–29 years are most at risk of developing myocarditis.
It also states that although 687 cases of myocarditis following vaccination had been reported in under-30s in the U.S. between December 29, 2020, and June 11, 2021, healthcare professionals had given more than 52 million doses of the vaccine to people aged 12–30 years in total. So, this represents a very small risk.
However, there was still a discussion to be had over whether or not the risks of the vaccine, which were very small, outweighed the risks of developing COVID-19, which were also smaller for this section of the population than older adults.
One study, which has not yet undergone peer review, claimed that the risk of experiencing an adverse cardiac event following mRNA vaccination in males aged 16–17 years without any comorbidities was actually 3.5 times higher than the risk of hospitalization due to COVID-19. This was widely reported in August 2021.
Conversely, a study in the New England Journal of Medicine from October 6, 2021, reported findings from the Israeli Ministry of Health surveillance of the issue that seemed to prove a link between receipt of the Pfizer vaccine and myocarditis.
Data collected between December 20, 2020, and May 31, 2021, confirmed 136 cases of myocarditis after receipt of the Pfizer vaccine out of 5.12 million Israelis who had received two doses. Analysis suggests that the risk is highest after the second dose in male recipients aged 16–19 years, with a risk ratio of 1 in 6,637.
Study co-author Prof. Manfred Green, from the Department of Epidemiology at the University of Haifa in Israel, told Medical News Today in an interview:
“Myocarditis is more common in males and females, [and] there are all kinds of theories why […]. [In the study, we found that] it generally was a mild illness, a mild infection and a minor event requiring hospitalization, as people with myocarditis are almost always hospitalized for observation. They required […] very basic anti-inflammatory treatment to treat the inflammation. All were fine, they recovered well.”
Dr. Green sits on the committee due to decide whether or not to proceed with licensing vaccines for 5–12-year-olds in Israel on November 10, 2021. He pointed out that as the dose given to 5–12-year-olds is one-third that of the dose given to older children and adults, “it is expected [that] there will be [fewer] side effects and [fewer] adverse events.”
Medically vulnerable children
Much of the concern voiced about side effects from COVID-19 vaccines is over the risk they may pose to healthy children.
Meanwhile, children who have some preexisting conditions will be particularly vulnerable to COVID-19 and will benefit more from vaccination. So, what about them?
There have been few studies into these children, as children in these groups are few in number. However, one study that appears in the journal Archives of Disease in Childhood found no problematic side effects in a group of 20 adolescents aged 12–15 years with neurological conditions.
Risk-benefit analysis
When evaluating the risks posed by possible side effects of the COVID-19 vaccine, it is impossible to do so without considering the possible benefits — though these may be hard to discern for the individual.
An analysis that appeared in the Journal of the Royal Society of Medicine on November 1, 2021, suggests that the vaccination of 12–17-year-olds is most beneficial while infection rates remain high — which, of course, they do in many parts of the world.
The analysis suggests that if SARS-CoV-2 infections are as high as 1,000 per 100,000 people per week over 16 weeks, vaccination could avert 4,430 hospital admissions and 36 deaths over 16 weeks. It also suggests that thousands of cases of long COVID could be avoided, even if the rate of long COVID was as low as 4% in teenagers.
Speaking at an Independent SAGE briefing on November 5, 2021, author Prof. Christina Pagel — a professor of operational research at UCL — said:
“It became really clear that if you got to really high case rates, then it is massively beneficial, and so even though children of 5–11 are less likely than adolescents to get really sick at the current rates of infection, with 6% [with the infection] at the end of October [in the U.K.], it is almost certain to be beneficial… I would be really surprised if there [weren’t] a benefit to vaccinating 5–11-year-olds, and I am a bit concerned that some members of [Joint Committee on Vaccination and Immunisation] are already saying ‘it’s too soon.’”