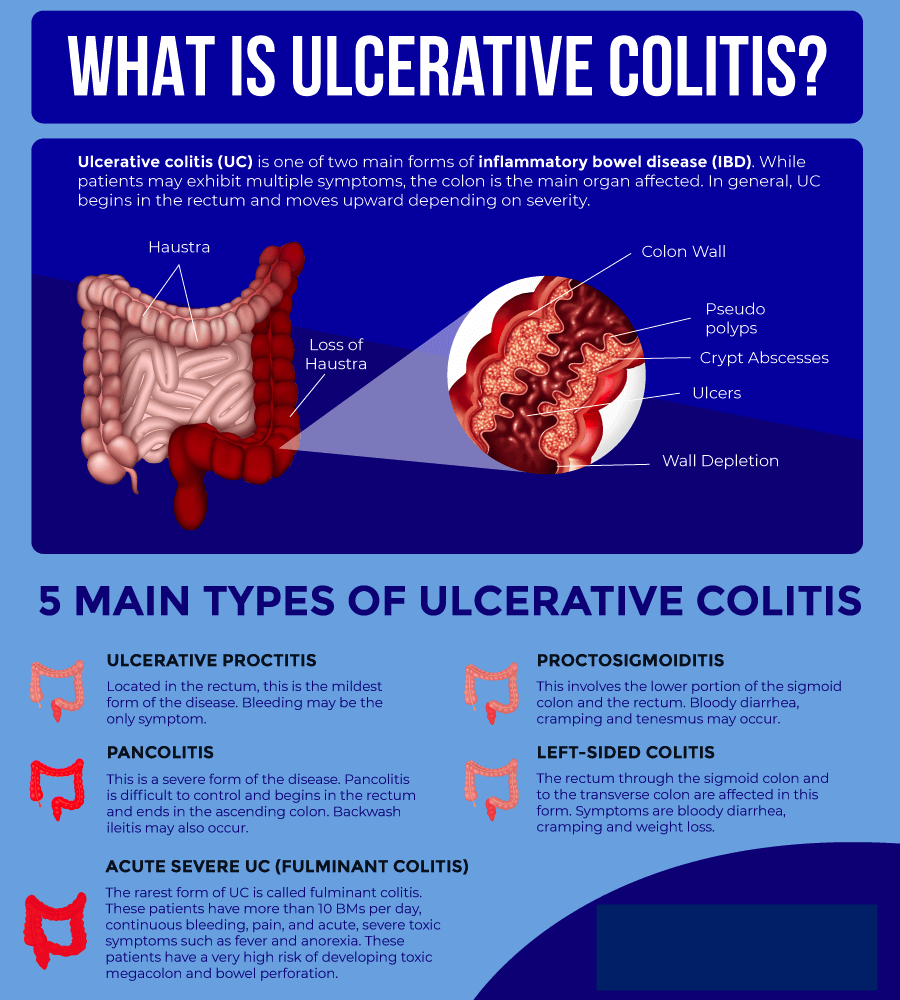
Ulcerative colitis is a relatively common long-term condition that causes inflammation in the colon. It is a form of inflammatory bowel disease (IBD) that is similar to Crohn’s disease.
The colon removes nutrients from undigested food and eliminates waste products through the rectum and anus as feces.
In severe cases, ulcers form on the lining of the colon. These ulcers may bleed, which produces pus and mucus.
Various medication options are available, and doctors can tailor treatment to meet individual needs.
Symptoms
The first symptom of ulcerative colitis is usually diarrhea.
Stools become progressively looser, and some people may experience abdominal pain with cramps and a severe urge to go to the bathroom.
Diarrhea may begin slowly or suddenly. Symptoms depend on the extent and spread of inflammation.
The most common symptoms of ulcerative colitis include:
- abdominal pain
- bloody diarrhea with mucus
Some people may also experience:
- fatigue or tiredness
- weight loss
- loss of appetite
- anemia
- elevated temperature
- dehydration
- a constant urge to pass stools
Symptoms are often worse early in the morning.
Symptoms may be mild or absent for months or years at a time. However, they will usually return without treatment and vary depending on the affected part of the colon.
What causes red diarrhea?
Types
Symptoms may vary depending on the area of inflammation.
The sections below discuss the various types of ulcerative colitis, many of which affect different parts of the colon:
Ulcerative proctitis
This type affects only the end of the colon, or the rectum. Symptoms tend to include:
- rectal bleeding, which may be the only symptom
- rectal pain
- an inability to pass stools despite frequent urges
Ulcerative proctitis is usually the mildest type of ulcerative colitis.
Proctosigmoiditis
This involves the rectum and the sigmoid colon, which is the lower end of the colon.
Symptoms include:
- bloody diarrhea
- abdominal cramps
- abdominal pain
- a constant urge to pass stool
Left-sided colitis
This affects the rectum and the left side of the sigmoid and descending colon.
Symptoms usually include:
- bloody diarrhea
- abdominal cramping on the left side
- weight loss
Pancolitis
This affects the whole colon. Symptoms include:
- occasionally severe, bloody diarrhea
- abdominal pain and cramps
- fatigue
- considerable weight loss
Fulminant colitis
This is a rare, potentially life threatening form of colitis that affects the whole colon.
Symptoms tend to include severe pain and diarrhea, which can lead to dehydration and shock.
Fulminant colitis can present a risk of colon rupture and toxic megacolon, which causes the colon to become severely distended.
Diet
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), some dietary measures may help relieve symptoms, including:
- eating smaller, more regular meals, such as five or six small meals per day
- drinking plenty of fluids, especially water, to prevent dehydration
- avoiding caffeine and alcohol, which can both increase diarrhea
- avoiding sodas, which can increase gas
- keeping a food diary to identify which foods make symptoms worse
A doctor may suggest temporarily following a specific diet depending on symptoms, such as:
- a low fiber diet
- a lactose-free diet
- a low fat diet
- a low salt diet
It may help to take supplements or eliminate particular foods from the diet. However, a person should discuss any complementary or alternative measures with a doctor before trying them.
Here, find out more about what to eat and avoid with ulcerative colitis.
Causes
The exact causes of ulcerative colitis are unclear. However, they may involve the following:
Genetic factors
ResearchTrusted Source suggests that people with ulcerative colitis are more likely to have certain genetic features. The specific genetic feature that a person has may affect the age at which the disease appears.
Environment
The following environmental factors might affect the onset of ulcerative colitis:
- diet
- air pollution
- cigarette smoke
Immune system
The body might respond to a viral or bacterial infection in a way that causes the inflammation associated with ulcerative colitis.
Once the infection resolves, the immune system continues to respond, which leads to ongoing inflammation.
Another theory suggests that ulcerative colitis may be an autoimmune condition. A fault in the immune system may cause it to fight nonexistent infections, leading to inflammation in the colon.
Risk factors
Some known risk factors for ulcerative colitis include:
- Age: Ulcerative colitis can affect people at any age but is more common at 15–30 years of age.
- Ethnicity: White people and those of Ashkenazi Jewish descent have a higher risk of developing the condition.
- Genetics: Although recent studies have identified specific genes that may play a role in ulcerative colitis, the link is unclear due to the role of environmental factors.
Diagnosis
A doctor will ask about a person’s symptoms and medical history. They will also ask whether any close relatives have had ulcerative colitis, IBD, or Crohn’s disease.
They will also check for signs of anemia, or low iron levels in the blood, and tenderness around the abdomen.
Several tests can help rule out other possible conditions and diseases, including Crohn’s disease, infection, and irritable bowel syndrome.
These include:
- blood tests
- stool tests
- X-ray
- barium enema, during which a healthcare professional passes a fluid called barium through the colon to show any changes or anomalies in a scan
- sigmoidoscopy, in which a healthcare professional inserts a flexible tube with a camera at the end, called an endoscope, into the rectum
- colonoscopy, wherein a doctor examines the whole colon using an endoscope
- a CT scan of the abdomen or pelvis
A person with ulcerative colitis will need to see a doctor who specializes in treating conditions of the digestive system, or a gastroenterologist.
They will assess the type and severity of the condition and create a treatment plan.
Treatment
Ulcerative colitis symptoms can range from mild to severe, but it needs treatment. Without treatment, the symptoms may go away, but there is a higher chance of them coming back.
Most people will receive outpatient treatment. However, around 15% of people with the disease have a severe form. Of these, 1 in 5 may need to spend time in the hospital.
Treatment will focus on:
- maintaining remission to prevent further symptoms
- managing a flare until symptoms go into remission
Various medications are available, and a doctor will make a treatment plan that takes individual needs and wishes into account. Natural approaches can support medical treatment, but they cannot replace it.
Long-term treatment to maintain remission
The first aim of treatment is to reduce the risk of a flare and its severity if a flare does occur. Long-term therapy can help achieve this.
There are several types of medication, and a doctor will make a treatment plan to suit the individual.
Ulcerative colitis results from a problem with the immune system. Three types of drugs that can help are biologics, immunomodulators, and small molecules. These target the way the immune system works.
They include:
- TNF-α antagonists, such as infliximab (Remicade) or adalimumab (Humira)
- anti-integrin agents, such as vedolizumab (Entyvio)
- Janus kinase inhibitors, such as tofacitinib (Xeljanz)
- interleukin 12/23 antagonists, such as ustekinumab (Stelara)
- immunomodulators, for instance, thiopurines (azathioprines) and methotrexate
These drugs can help people with moderate to severe symptoms, but they may have adverse effects. People should talk to their doctor about the options available and the benefits and risks of each drug.
However, for mild to moderate symptoms, guidelines suggest 5-aminosalicylic acid, or aminosalicylates (5-ASA), as a first-line treatment.
Examples include:
- mesalamine
- balsalazide
- sulfasalazine
Other options
Aminosalicylates: In the past, 5-ASA played a key role in treating the symptoms of ulcerative colitis. These are still an option, but current guidelines recommend focusing on long-term treatment to prevent symptoms from occurring in the first place.
Steroids: These can help manage inflammation if aminosalicylates do not help. However, long-term use can have adverse effects, and experts recommend minimizing their use.
Managing severe active ulcerative colitis
A person with severe symptoms may need to spend time in the hospital. Hospital treatment can reduce the risk of malnutrition, dehydration, and life threatening complications, such as colon rupture. Treatment will include intravenous fluids and medications.
Surgery
If other treatments do not provide relief, surgery may be an option.
Some surgical options include:
- Colectomy: A surgeon removes part or all of the colon.
- Ileostomy: A surgeon makes an incision in the stomach, extracts the end of the small intestine, and connects it to an external pouch, called a Kock pouch. The pouch then collects waste material from the intestine.
- Ileoanal pouch: A surgeon constructs a pouch from the small intestine and connects it to the muscles surrounding the anus. The ileoanal pouch is not an external pouch. Sometimes it is called a J-pouch.
According to the American Gastroenterological Association, around 10–15% of people with ulcerative colitis will need a colectomy.
Lifestyle and natural remedies
Some home care strategies and remedies may help manage the symptoms of ulcerative colitis.
Natural medicine
Here are some options that people may use:
- Probiotics: A 2019 review suggests that some probiotics may help manage IBD.
- Herbal remedies: Other researchTrusted Source from 2019 found that some herbal remedies may help reduce symptoms and manage the condition. Examples include aloe vera gel and wheatgrass juice.
- Fruits and other plant-based foods: Some earlier research shows that ingredients naturally present in blueberries, black raspberries, cocoa, Indian quince, green tea, grapes, olive oil, and Indian gooseberries may have a beneficial effect.
- Spices: Garlic, ginger, fenugreek, saffron, turmeric, and Malabar tamarind may help with IBD symptoms.
Research has not yet confirmed the possible benefits of the options above, but moderate amounts appear safe to add to the diet. However, it is worth checking with a healthcare professional first.
Lifestyle options
Scientists have also found that the following may help:
Education: The more a person knows about a health condition, the more in control they tend to feel. Learning about ulcerative colitis can help ease anxiety and lead to effective coping and management techniques, research from 2017Trusted Source shows.
Exercise: Some research suggests that aerobic exercise may have an anti-inflammatory effect, which could benefit people with ulcerative colitis. One 2019 studyTrusted Source, for example, found that combining exercise with an anti-inflammatory diet could have a positive effect. Check with a healthcare professional before changing an exercise routine, however, as 20% of participants with ulcerative colitis in a 2016 study experienced a worsening of symptoms after doing intense exercise.
Mindfulness: In a 2020 study, 37 people with ulcerative colitis engaged in a mindfulness-based intervention that involved four online therapy and four face-to-face sessions. After 6 months, the participants had lower markers of inflammation than 20 participants who did not have the sessions.
Complications
The possible complications of ulcerative colitis can range from a lack of nutrients to potentially fatal bleeding from the rectum.
Possible complications include:
Colorectal cancer
Ulcerative colitis, especially if symptoms are severe or extensive, increases the risk of developing colon cancer.
According to the NIDDK, colon cancer risk is highest when ulcerative colitis affects the entire colon for longer than 8 years.
Toxic megacolon
This complication occurs in a few cases of severe ulcerative colitis.
In toxic megacolon, gas becomes trapped, causing the colon to swell. When this occurs, there is a risk of colon rupture, septicemia, and shock.
Other complications
Other possible complications of ulcerative colitis include:
- inflammation of the skin, joints, and eyes
- liver disease
- osteoporosis
- perforated colon
- severe bleeding
- severe dehydration
To prevent bone density loss, a doctor may prescribe vitamin D supplements, calcium, or other medications.
Attending regular medical appointments, closely following a doctor’s advice, and being aware of symptoms can help prevent these complications.
Obesity
Obesity is a major risk factor for various metabolic disorders and cardiovascular diseases.
According to the World Health Organization (WHO), today, most of the world’s population lives in countries where obesity kills more people than malnutrition.
The prevalence of obesity has significantly increased in adults in the past few decades. As such, researchers are engaged in finding new ways to understand and potentially treat obesity.
A new study, which appears in the open-access journal PLOS Biology found that high levels of a cytokine — interleukin-25 — promotes the production of beige fat cells.
The study’s results might help find new ways to treat obesity and other metabolic disorders.
Significance of beige fat in humans
Not all fat stored in the body is harmful to health. Typically, there are two types of fat tissue: brown and white.
Brown fat helps turn food into heat, whereas white fat is responsible for storing calories; thus, an excess of white fat contributes to obesity.
However, scientists have discovered another type of fat cell in human adults, known as beige fat. Typically, these cells burn energy in a similar way to brown fat rather than storing it like white fat.
How do beige cells burn energy?
Beige fat cells, or adipocytes, are present in white adipose tissue. They can perform functions similar to both white and brown adipocytes. Generally, they act like white cells by storing energy.
However, when exposed to cold temperatures, they behave like brown cells and dissipate energy by creating heat.
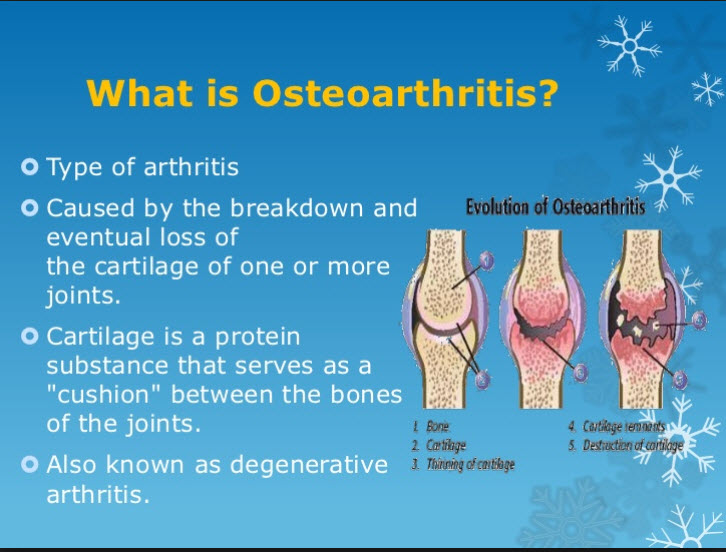
Everything you need to know about osteoarthritis
Osteoarthritis (OA) causes inflammation in the joints and the breakdown and gradual loss of joint cartilage. As the cartilage wears down, a person experiences pain and difficulty with movement.
OA is a common joint disorder. It develops in the hand, for example, in 1 in 12 people over the age of 60, according to the Arthritis Foundation.
OA is a progressive disease, which means that symptoms worsen over time.
There is no cure, but treatment can help manage pain and swelling and keep a person mobile and active.
Symptoms
OA leads to pain and stiffness in the joints.
In the early stages, a person may have no symptoms. Symptoms may occur in one or more joints, and they tend to appear gradually.
When symptoms develop, they can include:
- pain and stiffness that worsen after not moving the joint for a while
- swelling
- difficulty moving the affected joint
- warmth and tenderness in the joints
- a loss of muscle bulk
- a grating or crackling sound in the joint, known as crepitus
The progression of OA involves:
- synovitis — mild inflammation of the tissues around the joints
- damage and loss of cartilage
- bony growths that form around the edges of joints
Effects
Cartilage is a protective substance that cushions the ends of the bones in the joints and allows the joints to move smoothly and easily.
In people with OA, the smooth surface of the cartilage becomes rough and starts to wear away. As a result, the unprotected bones start to rub together, causing damage and pain.
Eventually, bony lumps form on the joint. The medical names for these are bone spurs or osteophytes, and they can lend a knobbly appearance to the joint.
As the bones change shape, the joints become stiffer, less mobile, and painful. Fluid may also accumulate in the joint, resulting in swelling. While OA can develop in any joint, it commonly affects the knees, hips, hands, lower back, and neck.
The knees
OA usually occurs in both knees, unless it results from an injury or another condition.
A person with the condition may notice that:
- There is pain when walking, especially uphill or upstairs.
- The knees lock into position, making it harder to straighten the leg.
- There is a soft, grating sound when they bend or flex the knee.
The hips
A person with OA in the hips may find that any movement of the hip joint, such as standing up or sitting down, can cause difficulty or discomfort.
Pain in the hips is a common feature of the condition. OA in the hips can also cause pain in the knee or in the thighs and buttocks.
A person may experience this pain while resting as well as while walking, for example.
The hands
In the hands, OA can develop in:
- the base of the thumb
- the top joint of the other fingers, closest to the nail
- the middle joint of the other fingers
A person with the condition may notice:
- pain, stiffness, and swelling in the fingers
- bumps that develop on the finger joints
- a slight bend sideways at the affected joints
- fluid-filled lumps or cysts on the backs of the fingers, which may be painful
- a bump that develops where the thumb joins the wrist, which can make it difficult to write or turn a key
For some people, the finger pain decreases and eventually goes away, though the swelling and bumps remain.
Anyone who experiences joint stiffness and swelling for more than 2 weeks should see a doctor.
Causes
Doctors do not know the exact cause of OA, but it seems to develop when the body is unable to repair joint tissue in the usual way.
It often affects older people, but it can occur at any age.
Genetic factors
Some genetic features increase the risk of developing OA. When these features are present, the condition can occur in people as young as 20 years old.
Trauma and overuse
A traumatic injury, surgery, or overuse of a joint can undermine the body’s ability to carry out routine repairs and may trigger OA, eventually leading to symptoms.
It can take several years for OA symptoms to appear after an injury.
Reasons for overuse or repeated injury include jobs and sports that involve repetitive movement.
Risk factors
A number of risk factors increase the chances of developing OA.
- Sex: OA is more common among females than males, especially after the age of 50.
- Age: Symptoms are more likely to appear after the age of 40, though OA can develop in younger people after an injury — especially to the knee — or as a result of another joint condition.
- Obesity: Excess weight can put strain on weight-bearing joints, increasing the risk of damage.
- Occupation: Jobs that involve repetitive movements in a particular joint increase the risk.
- Genetic and hereditary factors: These can increase the risk in some people.
Other conditions
Some diseases and conditions make it more likely that a person will develop OA.
- inflammatory arthritis, such as gout or rheumatoid arthritis
- Paget’s disease of the bone
- septic arthritis
- poor alignment of the knee, hip, and ankle
- having legs of different lengths
- some joint and cartilage abnormalities that are present from birth
Diagnosis
A doctor will ask about symptoms and perform a physical examination.
No definitive test can diagnose OA, but tests can show whether damage has occurred and help rule out other causes.
Tests may include:
X-rays and MRI: These can reveal bone spurs around a joint or a narrowing within a joint, suggesting that cartilage is breaking down.
Joint fluid analysis: A doctor will use a sterile needle to withdraw fluid from an inflamed joint for analysis. This can rule out gout or an infection.
Blood tests: These can help rule out other conditions, such as rheumatoid arthritis.
Treatment
While no treatment can reverse the damage of OA, some can help relieve symptoms and maintain mobility in the affected joints.
Interventions include exercise, manual therapy, lifestyle modification, and medication.
Medication
Medication can help reduce pain.
Acetaminophen (Tylenol)
This can relieve pain in people with mild to moderate symptoms. Follow the doctor’s instructions, as overuse can lead to side effects and cause interactions with other medications.
Nonsteroidal anti-inflammatory drugs
If acetaminophen does not help, the doctor may recommend a stronger pain reliever, which may include ibuprofen, aspirin, or diclofenac.
A person can take these orally or topically, applying the medication directly to the skin.
Capsaicin cream
This is a topical medication that contains the active compound in chilies. It creates a sensation of heat that can reduce levels of substance P, a chemical that acts as a pain messenger.
Pain relief can take 2 weeks to a month to fully take effect.
Do not use the cream on broken or inflamed skin, and avoid touching the eyes, face, and genitals after using it.
Intra-articular cortisone injections
Corticosteroid injections in the joint can help manage severe pain, swelling, and inflammation. These are effective, but frequent use can lead to adverse effects, including joint damage and a higher risk of osteoporosis.
Duloxetine (Cymbalta) is an oral drug that can help treat chronic musculoskeletal pain.
Physical therapy
Various types of physical therapy may help, including:
Transcutaneous electrical nerve stimulation (TENS): A TENS unit attaches to the skin with electrodes. Electrical currents then pass from the unit through the skin and overwhelm the nervous system, reducing its ability to transmit pain signals.
Thermotherapy: Heat and cold may help reduce pain and stiffness in the joints. A person could try wrapping a hot water bottle or an ice pack in a towel and placing it on the affected joint.
Manual therapy: This involves a physical therapist using hands-on techniques to help keep the joints flexible and supple.
Assistive devices
Various tools can provide physical support for a person with OA.
Special footwear or insoles can help, if OA affects the knees, hips, or feet, by distributing body weight more evenly. Some shock-absorbing insoles can also reduce the pressure on the joints.
A stick or cane can help take the weight off of the affected joints and may reduce the risk of a fall. A person should use it on side of the body opposite to the areas with OA.
Splints, leg braces, and supportive dressings can help with resting a painful joint. A splint is a piece of rigid material that provides joint or bone support.
Do not use a splint all the time, however, as the muscles can weaken without use.
Surgery
Some people may need surgery if OA severely affects the hips, knees, joints, or the base of the thumbs.
A doctor will usually only recommend surgery if other therapies have not helped or if there is severe damage in a joint.
Some helpful procedures include:
Arthroplasty
This involves a surgeon removing the damaged areas and inserting an artificial joint, made of metal and plastic. Some refer to this procedure as a total joint replacement.
The joints that most often require replacing are the hip and knee joints, but implants can also replace the joints in the shoulder, finger, ankle, and elbow.
Most people can use their new joint actively and painlessly. However, there is a small risk of infection and bleeding. An artificial joint may also come loose or wear down and eventually need replacing.
Arthrodesis
This involves a surgeon realigning, stabilizing, or surgically fixing the joint to encourage the bones to fuse. Increased stability can reduce pain.
A person with a fused ankle joint will be able to put their weight on it painlessly, but they will not be able to flex it.
Osteotomy
This involves a surgeon removing a small section of bone, either above or below the knee joint. It can realign the leg so that the person’s weight no longer bears down as heavily on the damaged part of the joint.
This can help relieve symptoms, but the person may need knee replacement surgery later on.
Complications
Septic arthritis is joint inflammation caused by bacteria. Joint replacement surgery slightly increases the risk of this infection.
This is a medical emergency, and hospitalization is necessary. Treatment involves antibiotic medication and drainage of the infected fluid from the joint.
Lifestyle tips
A range of strategies can help ease the symptoms of OA. Ask the doctor for advice about suitable lifestyle adjustments. They may recommend:
Exercise and weight control
Exercise is crucial for:
- maintaining mobility and range of movement
- improving strength and muscle tone
- preventing weight gain
- building up muscles
- reducing stress
- lowering the risk of other conditions, such as cardiovascular disease
Current guidelines recommend that everyone should do at least 150 minutes of moderate-intensity exercise each week.
A doctor or physical therapist can help develop an exercise program, and it is important to follow their instructions carefully to prevent further damage.
Choose activities that will not put additional strain on the joints. Swimming and other types of water-based exercise are a good way to keep fit without putting additional pressure on the joints.
Assistive devices and adjustments
A loss of mobility due to OA can lead to further problems, such as:
- an increased risk of falls
- difficulty carrying out daily tasks
- stress
- isolation and depression
- difficulty working
A physical or occupational therapist can help with these issues. They may recommend:
Assistive devices: Using a walker or cane can help prevent falls.
Adjustments to furniture and home fittings: Higher chairs and devices such as levers that make it easier to turn faucet knobs, for example, can help.
Talking to an employer: It may be possible to make adjustments to the workplace or arrange for more flexible hours.
Supplements
Some research has suggested that people with low vitamin D levels have a higher risk of OA. Also, in people with a low vitamin C intake, the disease may progress more rapidly.
Low levels of vitamin K and selenium may also contribute, but confirming these findings will require further research.
Some people use supplements for OA, including:
- omega-3 fatty acids
- calcium
- vitamin D
The American College of Rheumatology note that there is not enough evidence to support the safety and effectiveness of these supplements for OA. They recommend asking a doctor before using them.
Outlook
OA is a common disease that causes joints to deteriorate, leading to pain and stiffness. It tends to appear during middle age or later.
There is currently no cure, but researchers are looking for ways to slow or reverse the damage. Lifestyle remedies and pain relief medications can help manage it.
15 natural ways to lower your blood pressure
High blood pressure is a dangerous condition that can damage your heart. It affects one in three people in the US and 1 billion people worldwide.
If left uncontrolled, high blood pressure raises your risk of heart disease and stroke.
But there’s good news. There are a number of things you can do to lower your blood pressure naturally, even without medication.
Here are 15 natural ways to combat high blood pressure.
1. Walk and exercise regularly
Exercise is one of the best things you can do to lower high blood pressure. Regular exercise helps make your heart stronger and more efficient at pumping blood, which lowers the pressure in your arteries. In fact, 150 minutes of moderate exercise, such as walking, or 75 minutes of vigorous exercise, such as running, per week, can help lower blood pressure and improve your heart health.
What’s more, doing even more exercise than this reduces your blood pressure even further, according to the National Walkers’ Health Study.
Bottom line: Walking just 30 minutes a day can help lower your blood pressure. More exercise helps reduce it even further.
2. Reduce your sodium intake
Salt intake is high around the world. In large part, this is due to processed and prepared foods.
For this reason, many public health efforts are aimed at lowering salt in the food industry.
Many studies have linked high salt intake with high blood pressure and heart events, including stroke.
However, more recent research indicates that the relationship between sodium and high blood pressure is less clear.
One reason for this may be genetic differences in how people process sodium. About half of people with high blood pressure and a quarter of people with normal levels seem to have a sensitivity to salt.
If you already have high blood pressure, it’s worth cutting back your sodium intake to see if it makes a difference. Swap out processed foods with fresh ones and try seasoning with herbs and spices rather than salt.
Bottom line: Most guidelines for lowering blood pressure recommend reducing sodium intake. However, that recommendation might make the most sense for people who are salt-sensitive.
3. Drink less alcohol
Drinking alcohol can raise blood pressure. In fact, alcohol is linked to 16% of high blood pressure cases around the world.
While some research has suggested that low-to-moderate amounts of alcohol may protect the heart, those benefits may be offset by adverse effects.
In the U.S., moderate alcohol consumption is defined as no more than one drink a day for women and two for men. If you drink more than that, cut back.
Bottom line: Drinking alcohol in any quantity may raise your blood pressure. Limit your drinking in line with the recommendations.
4. Eat more potassium-rich foods
Potassium is an important mineral.
It helps your body get rid of sodium and eases pressure on your blood vessels.
Modern diets have increased most people’s sodium intake while decreasing potassium intake.
To get a better balance of potassium to sodium in your diet, focus on eating fewer processed foods and more fresh, whole foods.
Foods that are particularly high in potassium include:
- vegetables, especially leafy greens, tomatoes, potatoes, and sweet potatoes
- fruit, including melons, bananas, avocados, oranges, and apricots
- dairy, such as milk and yogurt
- tuna and salmon
- nuts and seeds
- beans
Bottom line: Eating fresh fruits and vegetables, which are rich in potassium, can help lower blood pressure.
5. Cut back on caffeine
If you’ve ever downed a cup of coffee before you’ve had your blood pressure taken, you’ll know that caffeine causes an instant boost.
However, there’s not a lot of evidence to suggest that drinking caffeine regularly can cause a lasting increase.
In fact, people who drink caffeinated coffee and tea tend to have a lower risk of heart disease, including high blood pressure, than those who don’t drink it.
Caffeine may have a stronger effect on people who don’t consume it regularly.
If you suspect you’re caffeine-sensitive, cut back to see if it lowers your blood pressure.
Bottom line: Caffeine can cause a short-term spike in blood pressure, although for many people, it does not cause a lasting increase.
6. Learn to manage stress
Stress is a key driver of high blood pressure.
When you’re chronically stressed, your body is in a constant fight-or-flight mode. On a physical level, that means a faster heart rate and constricted blood vessels.
When you experience stress, you might also be more likely to engage in other behaviors, such as drinking alcohol or eating unhealthful food that can adversely affect blood pressure.
Several studies have explored how reducing stress can help lower blood pressure. Here are two evidence-based tips to try:
- Listen to soothing music: Calming music can help relax your nervous system. Research has shown it’s an effective complement to other blood pressure therapies.
- Work less: Working a lot, and stressful work situations, in general, are linked to high blood pressure.
Bottom line: Chronic stress can contribute to high blood pressure. Finding ways to manage stress can help.
7. Eat dark chocolate or cocoa
Here’s a piece of advice you can really get behind.
While eating massive amounts of dark chocolate probably won’t help your heart, small amounts may.
That’s because dark chocolate and cocoa powder are rich in flavonoids, which are plant compounds that cause blood vessels to dilate.
A review of studies found that flavonoid-rich cocoa improved several markers of heart health over the short term, including lowering blood pressure.
For the strongest effects, use non-alkalized cocoa powder, which is especially high in flavonoids and has no added sugars.
Bottom line: Dark chocolate and cocoa powder contain plant compounds that help relax blood vessels, lowering blood pressure.
8. Lose weight
In people with overweight, losing weight can make a big difference to heart health.
According to a 2016 study, losing 5% of your body mass could significantly lower high blood pressure .
In previous studies, losing 17.64 pounds (8 kilograms) was linked to lowering systolic blood pressure by 8.5 mm Hg and diastolic blood pressure by 6.5 mm Hg.
To put that in perspective, a healthy reading should be less than 120/80 mm Hg.
The effect is even greater when weight loss is paired with exercise.
Losing weight can help your blood vessels do a better job of expanding and contracting, making it easier for the left ventricle of the heart to pump blood.
Bottom line: Losing weight can significantly lower high blood pressure. This effect is even more significant when you exercise.
9. Quit smoking
Among the many reasons to quit smoking is that the habit is a strong risk factor for heart disease.
Every puff of cigarette smoke causes a slight, temporary increase in blood pressure. The chemicals in tobacco are also known to damage blood vessels.
Surprisingly, studies haven’t found a conclusive link between smoking and high blood pressure. Perhaps this is because smokers develop a tolerance over time.
Still, since both smoking and high blood pressure raise the risk of heart disease, quitting smoking can help lessen that risk.
Bottom line: There’s conflicting research about smoking and high blood pressure, but what is clear is that both increase the risk of heart disease.
10. Cut added sugar and refined carbs
There’s a growing body of research showing a link between added sugar and high blood pressure.
In the Framingham Women’s Health Study, women who drank even one soda per day had higher levels than those who drank less than one soda per day.
Another study found that having one less sugar-sweetened beverage per day was linked to lower blood pressure .
And it’s not just sugar — all refined carbs, such as the kind found in white flour — convert rapidly to sugar in your bloodstream and may cause problems.
Some studies have shown that low carb diets may also help reduce blood pressure.
One study on people undergoing statin therapy found that those who went on a 6-week, carb-restricted diet saw a greater improvement in blood pressure and other heart disease markers than people who did not restrict carbs .
Bottom line: Refined carbs, especially sugar, may raise blood pressure. Some studies have shown that low carb diets may help reduce your levels.
11. Eat berries
Berries are full of more than just juicy flavor.
They’re also packed with polyphenols, natural plant compounds that are good for your heart.
Polyphenols can reduce the risk of stroke, heart conditions, and diabetes, as well as improving blood pressure, insulin resistance, and systemic inflammation.
One study assigned people with high blood pressure to a low-polyphenol diet or a high-polyphenol diet containing berries, chocolate, fruits, and vegetables.
Those consuming berries and polyphenol-rich foods experienced improved markers of heart disease risk.
Bottom line: Berries are rich in polyphenols, which can help lower blood pressure and the overall risk of heart disease.
12. Try meditation or deep breathing
While these two behaviors could also fall under “stress reduction techniques,” meditation and deep breathing deserve specific mention.
Both meditation and deep breathing may activate the parasympathetic nervous system. This system is engaged when the body relaxes, slowing the heart rate, and lowering blood pressure.
There’s quite a bit of research in this area, with studies showing that different styles of meditation appear to have benefits for lowering blood pressure.
Deep breathing techniques can also be quite effective.
In one study, participants were asked to either take six deep breaths over the course of 30 seconds or simply sit still for 30 seconds. Those who took breaths lowered their blood pressure more than those who just sat.
Try guided meditation or deep breathing. Here’s a video to get you started.
Bottom line: Both meditation and deep breathing can activate the parasympathetic nervous system, which helps slow your heart rate and lower blood pressure.
13. Eat calcium-rich foods
People with low calcium intake often have high blood pressure.
While calcium supplements haven’t been conclusively shown to lower blood pressure, calcium-rich diets do seem linked to healthful levels.
For most adults, the calcium recommendation is 1,000 milligrams (mg) per day. For women over 50 and men over 70, it’s 1,200 mg per day.
In addition to dairy, you can get calcium from collard greens and other leafy greens, beans, sardines, and tofu. Here is a list of calcium-rich plant-based foods.
Bottom line: Calcium-rich diets are linked to healthy blood pressure levels. You can get calcium through eating dark leafy greens and tofu, as well as dairy.
14. Take natural supplements
Some natural supplements may also help lower blood pressure. Here are some of the main supplements that have evidence behind them:
- Aged garlic extract: Researchers have used aged garlic extract successfully as a stand-alone treatment and along with conventional therapies for lowering blood pressure.
- Berberine: Traditionally used in Ayurvedic and Chinese medicine, berberine may increase nitric oxide production, which helps decrease blood pressure.
- Whey protein: A 2016 study found that whey protein improved blood pressure and blood vessel function in 38 participants.
- Fish oil: Long credited with improving heart health, fish oil may benefit people with high blood pressure the most.
- Hibiscus: Hibiscus flowers make a tasty tea. They’re rich in anthocyanins and polyphenols that are good for your heart and may lower blood pressure.
Bottom line: Researchers have investigated several natural supplements for their ability to lower blood pressure.
15. Eat foods rich in magnesium
Magnesium is an important mineral that helps blood vessels relax.
While magnesium deficiency is pretty rare, many people don’t get enough.
Some studies have suggested that getting too little magnesium is linked with high blood pressure, but evidence from clinical studies has been less clear.
Still, eating a magnesium-rich diet is a recommended way to ward off high blood pressure.
You can incorporate magnesium into your diet by consuming vegetables, dairy products, legumes, chicken, meat, and whole grains.
Bottom line: Magnesium is an essential mineral that helps regulate blood pressure. Find it in whole foods, such as legumes and whole grains.
Take home message
High blood pressure affects a large proportion of the world’s population.
While drugs are one way to treat the condition, there are many other natural techniques, including eating certain foods that can help.
BACK PAIN
Back pain is a common reason for absence from work and for seeking medical treatment. It can be uncomfortable and debilitating.
It can result from injury, activity and some medical conditions. Back pain can affect people of any age, for different reasons. As people get older, the chance of developing
lower back pain increases, due to factors such as previous occupation and degenerative disk disease.
Lower back pain may be linked to the bony lumbar spine, discs between the vertebrae, ligaments around the spine and discs, spinal cord and nerves, lower back muscles, abdominal and pelvic internal organs, and the skin around the lumbar area.
Pain in the upper back may be due to disorders of the aorta, tumors in the chest, and spine inflammation.
Causes
Problems with the spine such as osteoporosis can lead to back pain.
The human back is composed of a complex structure of muscles, ligaments, tendons, disks, and bones, which work together to support the body and enable us to move around.
The segments of the spine are cushioned with cartilage-like pads called disks.
Problems with any of these components can lead to back pain. In some cases of back pain, its cause remains unclear.
Damage can result from strain, medical conditions, and poor posture, among others.
Strain
Back pain commonly stems from strain, tension, or injury. Frequent causes of back pain are:
- strained muscles or ligaments
- a muscle spasm
- muscle tension
- damaged disks
- injuries, fractures, or falls
Activities that can lead to strains or spasms include:
- lifting something improperly
- lifting something that is too heavy
- making an abrupt and awkward movement
Structural problems
A number of structural problems may also result in back pain.
- Ruptured disks: Each vertebra in the spine is cushioned by disks. If the disk ruptures there will be more pressure on a nerve, resulting in back pain.
- Bulging disks: In much the same way as ruptured disks, a bulging disk can result in more pressure on a nerve.
- Sciatica: A sharp and shooting pain travels through the buttock and down the back of the leg, caused by a bulging or herniated disk pressing on a nerve.
- Arthritis: Osteoarthritis can cause problems with the joints in the hips, lower back, and other places. In some cases, the space around the spinal cord narrows. This is known as spinal stenosis.
- Abnormal curvature of the spine: If the spine curves in an unusual way, back pain can result. An example is scoliosis, in which the spine curves to the side.
- Osteoporosis: Bones, including the vertebrae of the spine, become brittle and porous, making compression fractures more likely.
- Kidney problems: Kidney stones or kidney infection can cause back pain.
Movement and posture
Adopting a very hunched sitting position when using computers can result in increased back and shoulder problems over time.
Back pain can also result from some everyday activities or poor posture.
Examples include:
- twisting
- coughing or sneezing
- muscle tension
- over-stretching
- bending awkwardly or for long periods
- pushing, pulling, lifting, or carrying something
- standing or sitting for long periods
- straining the neck forward, such as when driving or using a computer
- long driving sessions without a break, even when not hunched
- sleeping on a mattress that does not support the body and keep the spine straight
Other causes
Some medical conditions can lead to back pain.
- Cauda equina syndrome: The cauda equine is a bundle of spinal nerve roots that arise from the lower end of the spinal cord. Symptoms include a dull pain in the lower back and upper buttocks, as well as numbness in the buttocks, genitalia, and thighs. There are sometimes bowel and bladder function disturbances.
- Cancer of the spine: A tumor on the spine may press against a nerve, resulting in back pain.
- Infection of the spine: A fever and a tender, warm area on the back could be due to an infection of the spine.
- Other infections: Pelvic inflammatory disease, bladder, or kidney infections may also lead to back pain.
- Sleep disorders: Individuals with sleep disorders are more likely to experience back pain, compared with others.
- Shingles: An infection that can affect the nerves may lead to back pain. This depends on which nerves are affected.
Risk factors
The following factors are linked to a higher risk of developing low back pain:
- occupational activities
- pregnancy
- a sedentary lifestyle
- poor physical fitness
- older age
- obesity and excess weight
- smoking
- strenuous physical exercise or work, especially if done incorrectly
- genetic factors
- medical conditions, such as arthritis and cancer
Lower back pain also tends to be more common in women than in men, possibly due to hormonal factors. Stress, anxiety, and mood disorders have also been linked to back pain.
Symptoms
The main symptom of back pain is an ache or pain anywhere in the back, and sometimes all the way down to the buttocks and legs.
Some back issues can cause pain in other parts of the body, depending on the nerves affected.
The pain often goes away without treatment, but if it occurs with any of the following people should see their doctor:
- weight loss
- fever
- inflammation or swelling on the back
- persistent back pain, where lying down or resting does not help
- pain down the legs
- pain that reaches below the knees
- a recent injury, blow or trauma to the back
- urinary incontinence
- difficulty urinating
- fecal incontinence, or loss of control over bowel movements
- numbness around the genitals
- numbness around the anus
- numbness around the buttocks
When to see a doctor
You should seek medical help if you experience any numbness or tingling, or if you have back pain:
- that does not improve with rest
- after an injury or fall
- with numbness in the legs
- with weakness
- with fever
- with unexplained weight loss
Diagnosis
A doctor will usually be able to diagnose back pain after asking about symptoms and carrying out a physical examination.
An imaging scan and other tests may be required if:
- back pain appears to result from an injury
- there may be underlying cause that needs treatment
- the pain persists over a long period
An X-ray, MRI, or CT scan can give information about the state of the soft tissues in the back.
- X-rays can show the alignment of the bones and detect signs of arthritis or broken bones, but they may not reveal damage in the muscles, spinal cord, nerves, or disks.
- MRI or CT scans can reveal herniated disks or problems with tissue, tendons, nerves, ligaments, blood vessels, muscles, and bones.
- Bone scans can detect bone tumors or compression fractures caused by osteoporosis. A radioactive substance or tracer is injected into a vein. The tracer collects in the bones and helps the doctor detect bone problems with the aid of a special camera.
- Electromyography or EMG measures the electrical impulses produced by nerves in response to muscles. This can confirm nerve compression, which may occur with a herniated disk or spinal stenosis.
The doctor may also order a blood test if infection is suspected.
Other types of diagnosis
- A chiropractor will diagnose through touch, or palpation, and a visual examination. Chiropractic is known as a direct approach, with a strong focus on adjusting the spinal joints. A chiropractor may also want to see the results of imaging scans and any blood and urine tests.
- An osteopath also diagnoses through palpation and visual inspection. Osteopathy involves slow and rhythmic stretching, known as mobilization, pressure or indirect techniques, and manipulation of joints and muscles.
- A physical therapist focuses on diagnosing problems in the joints and soft tissues of the body.
Chronic or acute pain?
Back pain is categorized into two types:
- Acute pain starts suddenly and lasts for up to 6 weeks.
- Chronic or long-term pain develops over a longer period, lasts for over 3 months, and causes ongoing problems.
If a person has both occasional bouts of more intense pain and fairly continuous mild back pain, it can be hard for a doctor to determine whether they have acute or chronic back pain.

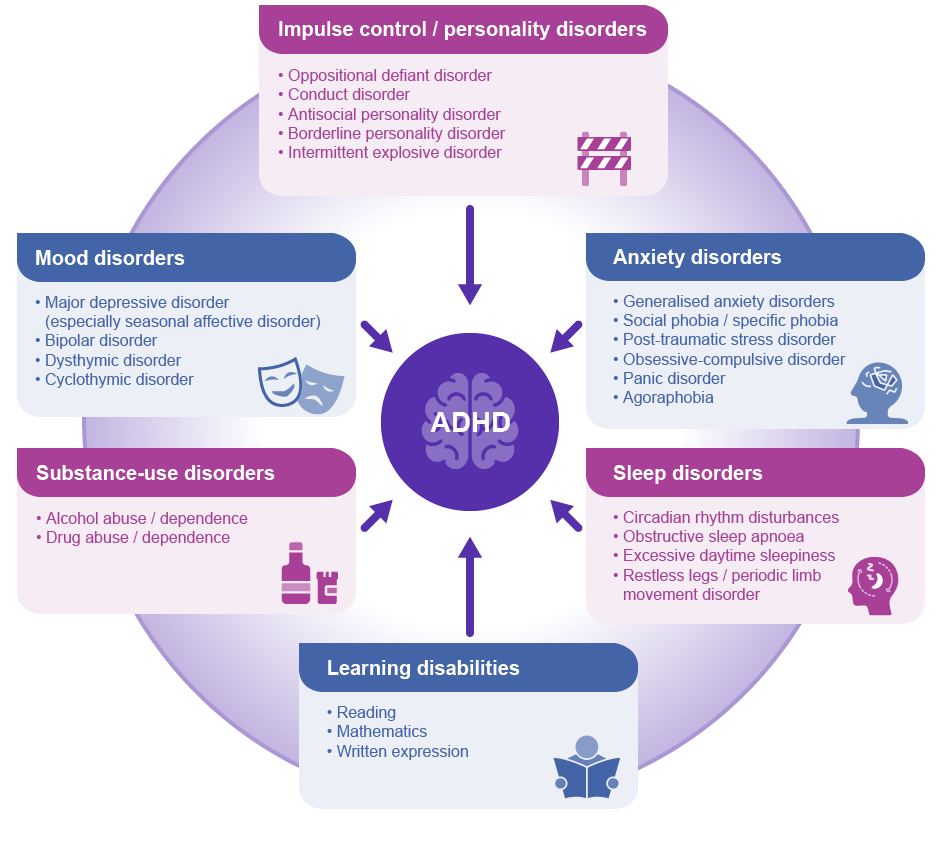
What to know about ADHD
A person with untreated attention deficit hyperactivity disorder (ADHD) has difficulty maintaining attention, managing energy levels, and controlling impulses.
In the United States, around 8.4% of children and 2.5% of adults have ADHD. In some children, ADHD characteristics begin as early as 3 years of age.
Ways of treating ADHD include medication, behavioral management techniques, and other practical strategies.
Below, we explore what ADHD is, how it affects a person, and which treatments can help.
What is ADHD?
People with ADHD have difficulty focusing on tasks and controlling their attention, which can make completing a project, for example, challenging. ADHD can limit a person’s ability to study or work, and it can lead to stress, anxiety, and depression.
Some people with ADHD also find it hard to sit still. They may be quick to act on impulse and become easily distracted.
While children of any age can experience distraction and impulsiveness, these traits are more noticeable in those with ADHD.
Features
ADHD may develop in one of three ways. A doctor may find that the disorder has:
- a predominantly hyperactive and impulsive presentation
- a predominantly inattentive presentation
- a combined presentation
People with ADHD experience hyperactivity, impulsivity, and inattention in varying degrees.
Inattention
Below are some behaviors related to inattention that a person might notice in someone with ADHD:
- daydreaming
- becoming distracted and having difficulty focusing on tasks
- making “careless” mistakes
- appearing to not listen while others are talking
- having difficulty with time management and organization
- frequently losing everyday items
- avoiding tasks that need prolonged focus and thought
- having difficulty following instructions
Hyperactivity and impulsivity
Some or all of the following may be apparent in someone with ADHD:
- seeming constantly “on-the-go” and unable to sit still
- running or climbing at inappropriate times
- having difficulty taking turns in conversations and activities
- fidgeting or tapping the hands or feet
- talking and making noises excessively
- taking unnecessary risks
In adults
Adults and children tend to experience the same symptoms of ADHD, and these can create difficulties in relationships and at work.
The effects of these features vary widely from person to person, and a person may find that their experience of ADHD changes over time.
Not everyone with ADHD is noisy and disruptive. A child may be quiet in class, for example, while facing severe challenges that they do not express.
In females
Females with ADHD may be more likely to have difficulty paying attention, while males may be more likely to experience hyperactivity and impulsivity.
This may be one reason why more males than females receive diagnoses of ADHD. Hyperactivity can be easier to spot than inattention.
Diagnosis
Most children with ADHD receive a diagnosis while they are in elementary school, but some may not do so until adolescence or adulthood.
No single test can identify ADHD, and the symptoms can overlap with those of other conditions. This can make it difficult to diagnose.
A doctor will conduct examinations to rule out other potential causes, such as hearing or vision problems.
Other conditions that can lead to similar behaviors include:
- trouble hearing or seeing
- anxiety
- depression
- learning disabilities
- sleep disorders
A doctor will often ask questions to learn more about the person’s behavioral patterns. They may speak with the individual, members of their family, and any other caregivers, such as teachers.
Many children experience hyperactivity and inattention. For a diagnosis of ADHD, the symptoms must meet specific criteria, including having a significant impact on daily life and schoolwork.