My Parents Are Vaccinated but I’m Not. Is It Safe for Us to Visit?
There’s no zero-risk activity while the virus is still circulating. But older adults who have been vaccinated should feel more confident in taking part in activities with people who are considered low-risk.
For older adults who have been isolated from family and friends for the better part of a year to stay safe from the coronavirus, the emergency authorization of two COVID-19 vaccines offers some light at the end of the tunnel.
While the vaccine certainly offers more protection, experts caution it’ll still take some time before life returns to normal.
That includes what visits with loved ones will look like.
It’s exciting for people who have been vaccinated to think about resuming those things again, but we’re still not out of the woods yet.
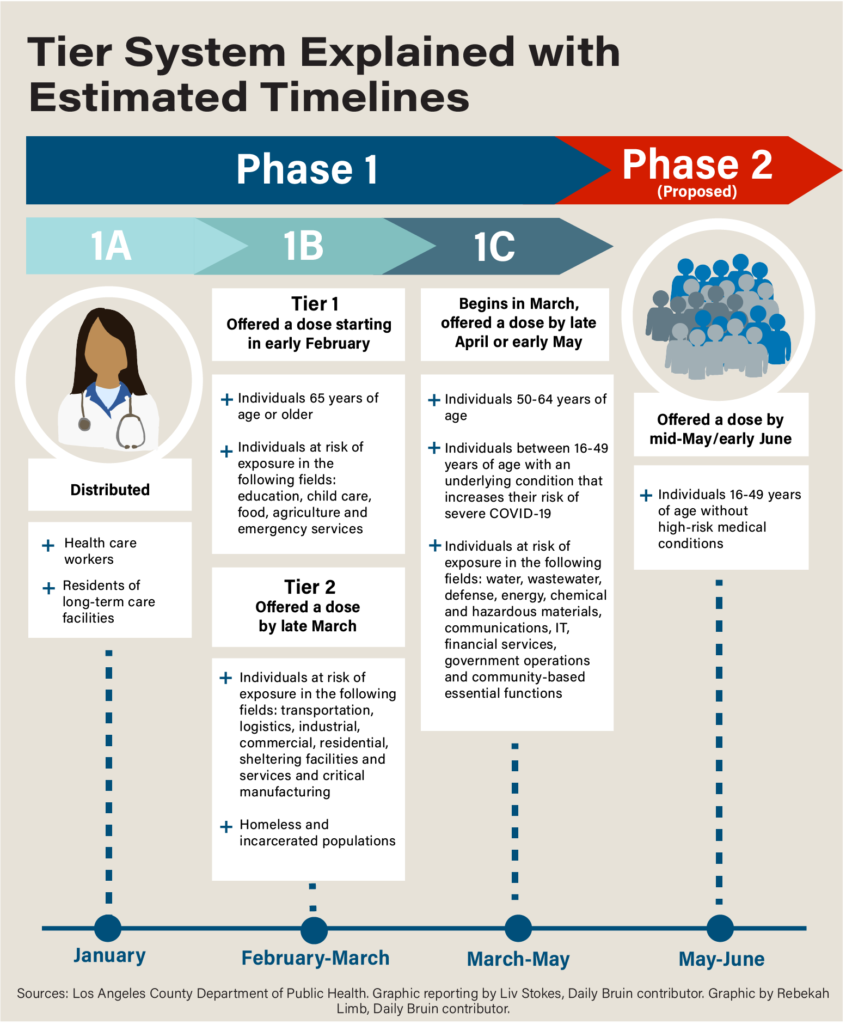
As the United States continues its vaccine rollout, people over the age of 75, along with frontline essential workers, are being prioritized to receive the shot after healthcare personnel and nursing home residents.
In the next phase, people 65 to 74 and adults with underlying health conditions will be offered the vaccine.
This will put many families in a situation where older adults are vaccinated, but their children and grandchildren aren’t.
Healthline spoke with medical experts to see how families should go about visiting loved ones safely in these situations.
The risk is not zero
Dr. Colleen Kelley, an associate professor of infectious diseases at Emory University School of Medicine, said that while the vaccine is moving the country in the right direction, “we are not in a zero risk situation and a few things need to happen before we get down to even a minimal risk situation.”
Those things include getting most of the population vaccinated and getting community transmission of COVID-19 under control.
“We are still at levels well above what we saw during the summer surge in most places,” said Kelley, who’s also a principal investigator for the Moderna and Novavax phase 3 vaccine clinical trials at the Ponce de Leon clinical research site.
Both she and Factora said it’ll be well into 2021 before we get to this point.
Until then, the same protective measures that have been in place to prevent the spread of COVID-19, including physical distancing, mask wearing, and good hand hygiene, should continue to be practiced when visiting loved ones.
“Today in February, I would do the same things I was doing in December,” Kelley said. “Visit outdoors wherever possible. If you’re indoors, be masked. We still need to keep any gatherings very small and limited as much as possible.”
One reason for this is that whichever vaccine an individual gets, it won’t be 100 percent effective. “Even with 94 or 95 percent efficacy with the Moderna and Pfizer vaccine, you still have that risk,” Factora said.
At the rate at which the virus is spreading across the country, even that 5 percent chance can still be risky.
“Even though the vaccine protects you, there’s still that risk that you’ll contract it and for older adults, you’re still going to be at higher risk of severe illness, hospitalization, and death compared to the rest of the population,” Factora said.
It’s also not known yet how well the vaccine is going to protect against emergent variants of the virus that are more contagious.
“That’s something scientists are studying, but it’s going to take some time to figure out,” Factora said.
What activities are safe for older adults who have been vaccinated?
There’s no zero-risk activity while the virus is still circulating. But older adults who have been vaccinated should feel more confident in taking part in activities with people who are considered low-risk.
“Particularly outdoor activities and particularly gatherings that are small, if you’re seeing family members who are not vaccinated but are still practicing social distancing and mask wearing,” Factora said, “you should feel safer because you now have an added protection with the vaccine.”
However, there’s an added complication for many families: The vaccine hasn’t been authorized for use in children.
The Pfizer vaccine has been authorized for people 16 and older, while the Moderna vaccine has been authorized for people 18 and older.
“There’s no time soon where we expect our children to be vaccinated,” Kelley said.
This may be of particular concern when it comes to older children and teenagers who are more likely to have larger social circles.
“In these instances, I think it’s a good idea for older adults to ask questions before a visit about where their grandkids have been over the last 10 days,” Factora said.
“If they’ve been keeping to themselves during that time and haven’t had symptoms, then you’re at lower risk of getting something because you’re outside the window where risk of transmission is highest,” he said.
Factora added: “If you can prepare for planned events by asking these questions and again keep the visits outdoors and limited, I think that’s a safe way for grandparents to see their grandkids.”
Experts said that once everyone in your social bubble has been vaccinated, the risk of COVID-19 transmission goes down.
While this may take a while for families with multiple generations, older adults should feel more comfortable about spending time with peers of the same age who have also been vaccinated.
“If you get vaccinated and the people within your bubble get vaccinated, you should have greater confidence that you’ll be less likely to contract COVID-19,” Factora said.
“This is great for many older adults in independent or assisted living facilities,” he said. “Engaging in social activities like card games and common dinners with friends and neighbors who have also been vaccinated, this should give you a better sense of safety.”
Until more of the population is vaccinated and community transmission goes down, older adults should still stay away from closed indoor spaces that are poorly ventilated.
“Bars, restaurants, crowded rooms, places where there’s lots of people — these are circumstances that are still considered highest risk that should be avoided,” Factora said.
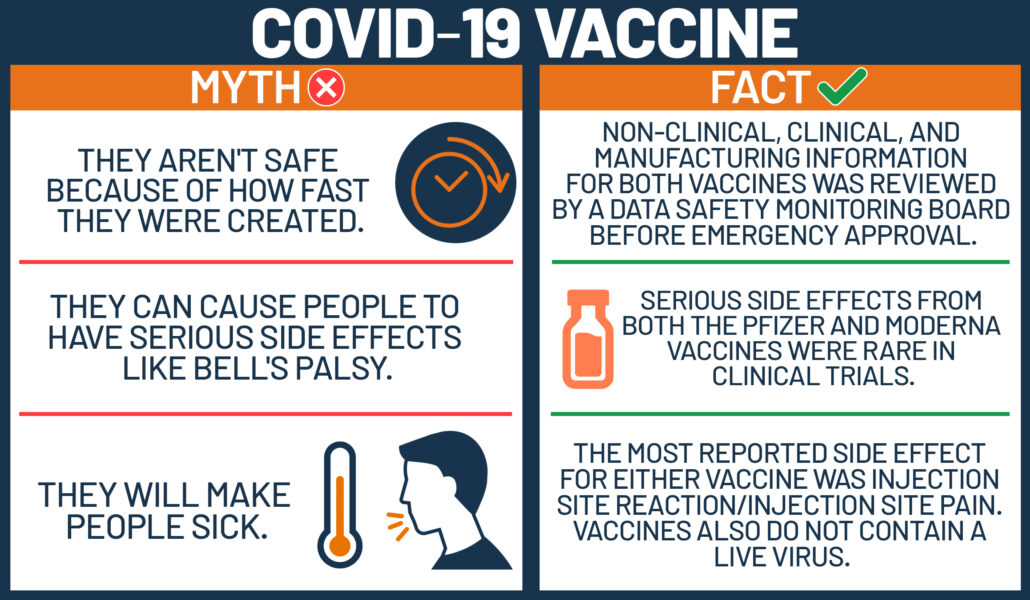
13 COVID-19 vaccine myths
Of all the modern medical interventions we have at our disposal, few have been victim to as much falsehood as vaccines. As the world battles a pandemic, stripping the truth from the lies is more urgent than ever.
According to the World Health Organization (WHO), between 2010 and 2015, vaccines prevented an estimated 10 million deaths.
Scientists have worked tirelessly to create safe and effective vaccines to protect us against SARS-CoV-2. Now, as many governments roll out COVID-19 vaccines, scientists and medical experts are facing a new challenge: misinformation and associated vaccine hesitancy.
Some anti-vaxxers — individuals who believe vaccines cause a range of medical ills — dedicate their entire lives to railing against vaccines. In reality, vaccines have saved lives of millions of people.
Vaccine hesitancy is nothing new and, in many ways, perfectly reasonable. For instance, misinformation about the vaccines’ safety and potential effects on the body is rife on the internet. Also, the COVID-19 vaccines were developed unusually swiftly and use relatively new technology.
Today, a significant percentage of the United States population, and the world at large, are nervous to take a shot that could save their lives.
In this article, we tackle some of the most common myths associated with the COVID-19 vaccines. Although it will not convince dyed-in-the-wool anti-vaxxers, we hope that this information will prove useful for those who are hesitant.
1. The vaccines are not safe, because they were developed so fast
It is true that scientists developed the COVID-19 vaccines faster than any other vaccine to date — under 1 year. The previous record breaker was the mumps vaccine, which was developed in 4 years.
There are a number of reasons the COVID-19 vaccines were developed more quickly, none of which reduces its safety profile.
For instance, scientists were not starting from scratch. Although SARS-CoV-2 was new to science, researchers have been studying coronaviruses for decades.
Also, because COVID-19 has touched every continent on earth, the process of vaccine development involved an unprecedented worldwide collaboration. And, while many scientific endeavors face funding difficulties, COVID-19 researchers received funding from a wide range of sponsors.
Another factor that slows vaccine development is recruiting volunteers. In the case of COVID-19, there was no shortage of people who wanted to help.
Also, under normal circumstances, clinical trials are run sequentially. But in this instance, scientists could run some trials simultaneously, which saved a great deal of time.
These factors and more meant that the vaccine could be developed swiftly without compromising safety.
In short: identifying the virus was quicker; we already had experience with similar pathogens; technology has moved on since the 1980s; every government on earth had a vested interest; and there were few financial restraints.
2. The vaccine will alter my DNA
Some COVID-19 vaccines, including the Pfizer-BioNTech and Moderna vaccines, are based on messenger RNA (mRNA) technology. These vaccines work differently to traditional types of vaccine.
Classical vaccines introduce an inactivated pathogen or part of a pathogen to the body to “teach” it how to produce an immune response.
By contrast, an mRNA vaccine delivers the instructions for making a pathogen’s protein to our cells. Once the protein is created, the immune system responds to it, priming it to respond to future attacks by the same pathogen.
However, the mRNA does not hang around in the body, and it is not integrated into our DNA. Once it has provided the instructions, the cell breaks it down.
In fact, the mRNA will not even reach the cell’s nucleus, which is where our DNA is housed.
3. COVID-19 vaccines can give you COVID-19
The COVID-19 vaccines cannot give an individual COVID-19. Regardless of the type of vaccine, none contains the live virus. Any side effects, such as headache or chills, are due to the immune response and not an infection.
4. The vaccine contains a microchip
A YouGov poll conducted in the U.S. last year asked 1,640 people a range of questions about COVID-19. An incredible 28% of respondents believe that Bill Gates plans to use the COVID-19 vaccinations as a vehicle to implant microchips into the population.
According to some, this microchip will allow shadowy elites to track their every move. In reality, our mobile phones already complete that task effortlessly.
There is no evidence that any of the COVID-19 vaccines contains a microchip.
Although the specifics vary from conspiracy theory to conspiracy theory, some believe that the vaccine contains radio-frequency identification tags. These consist of a radio transponder, radio receiver, and transmitter. It is not possible to shrink these components to a size small enough to fit through the end of a needle.
5. COVID-19 vaccines can make you infertile
There is no evidence that the COVID-19 vaccines impact fertility. Similarly, there is no evidence that they will endanger future pregnancies.
This rumor began because of a link between the spike protein that is coded by the mRNA-based vaccines and a protein called syncytin-1. Syncytin-1 is vital for the placenta to remain attached to the uterus during pregnancy.
However, although the spike protein does share a few amino acids in common with syncytin-1, they are not even nearly similar enough to confuse the immune system.
The rumor appears to have begun courtesy of Dr. Wolfgang Wodarg. In December of last year, he petitioned the European Medicines Agency to halt COVID-19 vaccine trials in the European Union. Among his concerns was the syncytin-1 “issue” mentioned above.
Dr. Wodarg has a history of skepticism toward vaccines and has downplayed the severity of the COVID-19 pandemic. Dr. Wodarg and the former vice president and chief scientist of Pfizer Inc. pharmaceuticals joined voices to make claims about the vaccine producing infertility, thus stoking widespread fears.
However, there is no evidence that any COVID-19 vaccine affects fertility.
6. The COVID-19 vaccine contains fetal tissue
Over the years, anti-vaxxers have spread rumors that vaccines contain fetal tissue. Neither the COVID-19 vaccines nor any other vaccine contains any tissue from fetuses.
As Dr. Michael Head, a senior research fellow at the University of Southampton in the United Kingdom, told the BBC, “There are no fetal cells used in any vaccine production process.”
7. People who have had COVID-19 do not need the vaccine
Even people who have tested positive for SARS-CoV-2 in the past should be vaccinated. As the Centers for Disease Control and Prevention (CDC) write:
“Due to the severe health risks associated with COVID-19 and the fact that reinfection with COVID-19 is possible, [a] vaccine should be offered to you regardless of whether you already had [a SARS-CoV-2] infection.”
There is also a chance that the initial test produced a false positive — in other words, the test was positive, but there was no viral infection. For this reason, it is better to err on the side of caution.
8. After receiving the vaccine, you cannot transmit the virus
COVID-19 vaccines are designed to prevent people from becoming ill following a SARS-CoV-2 infection. However, a person who has been vaccinated may still be able to carry the virus, which means that they might also be able to transmit it.
Because scientists do not yet know whether the vaccines will prevent infection, once a person has been vaccinated, they should continue to wear a mask in public, wash their hands, and practice physical distancing as recommended by regional authorities.
9. Once I have been vaccinated, I can resume a normal life
Unfortunately, for the reasons mentioned above, this is not true.
10. The vaccine will protect against COVID-19 for life
Because scientists have only been studying the virus for around 1 year, we do not know how long immunity will last. According to the WHO:
“It’s too early to know if COVID-19 vaccines will provide long-term protection. […] However, it’s encouraging that available data suggest that most people who recover from COVID-19 develop an immune response that provides at least some period of protection against reinfection — although we’re still learning how strong this protection is and how long it lasts.”
It may be that we will need to have an annual COVID-19 shot, in the same way that we do with the flu shot.
11. People with preexisting conditions cannot take the vaccine
This is untrue. People with most preexisting conditions — including heart disease, diabetes, and lung disease — can take a COVID-19 vaccine. However, if anyone is concerned, it is always advisable to speak with a doctor.
In fact, because preexisting conditions, such as obesity and heart disease, can increase the risk of developing more severe COVID-19 symptoms, being vaccinated is even more important for people with preexisting health issues.
There is an exception: individuals who are allergic to any of the components of the vaccine should not have the shot. Anyone who has had an allergic reaction to any vaccine in the past should speak with their doctor.
However, the CDC recommend “that people with a history of severe allergic reactions not related to vaccines or injectable medications — such as food, pet, venom, environmental, or latex allergies — get vaccinated. People with a history of allergies to oral medications or a family history of severe allergic reactions may also get vaccinated.”
12. People with compromised immune systems cannot have the vaccine
Because the vaccine does not contain a live pathogen, it will not cause an infection. Therefore, individuals who have a compromised immune system can still take the vaccine. However, they may not build up immune protection to the same degree as someone with a fully functioning immune system.
The CDC also explain that few people who have a compromised immune system were involved in the vaccine trials:
“Immunocompromised individuals may receive [a] COVID-19 vaccination if they have no contraindications to vaccination. However, they should be counseled about the unknown vaccine safety profile and effectiveness in immunocompromised populations.”
13. Older adults cannot have the vaccine
This is a myth. Currently, in most countries where officials are rolling out the vaccine, older adults are being prioritized, as they are most at risk of severe illness.
Also, some of the clinical trials had specific subgroups that included older adults to check the vaccine’s safety in this population.
In Norway, 23 frail older adults died shortly after they received the Pfizer-BioNTech vaccine. This, perhaps, helps explain why this myth is gaining traction.
The Norwegian Medicines Agency (NOMA) are currently investigating the situation. Steinar Madsen, a medical director at NOMA, believes that common adverse reactions, such as fever, nausea, and diarrhea, “may aggravate underlying disease in the elderly.”
Madsen also explained that “these are very rare occurrences, and they occurred in very frail patients with very serious disease.” He went on to add,
“We are now asking for doctors to continue with the vaccination but to carry out extra evaluation of very sick people whose underlying condition might be aggravated by it.”
The take-home
It is hard to believe that not much more than 1 year ago, COVID-19 and SARS-CoV-2 were entirely unknown. Now, we have a number of viable, effective, and safe vaccines.
In this internet-fueled era, rumors grow and spread like wildfire. The addition of a significant dose of fear and anxiety provides the perfect petri dish in which to grow stubborn, dangerous myths.
The situation and the science are moving quickly, and the best advice is to ensure that you always take information from reliable sources and do not pay attention to powerful but misleading social media posts.
Learn how to tell if someone has COVID-19 or the flu here.
COVID-19 and the flu can cause similar symptoms. However, there are several differences between them.
The novel strain of coronavirus (SARS-CoV-2) causes coronavirus disease 19 (COVID-19).
Both COVID-19 and the flu are respiratory illnesses that spread from person to person. This article will discuss the differences between COVID-19 and the flu.
Symptoms
The symptoms of the flu and COVID-19 have some differences.
People who have the flu will typically experience symptoms within 1–4 days. The symptoms for COVID-19 can develop between 1–14 days. However, according to 2020 research, the median incubation period for COVID-19 is 5.1 days.
As a point of comparison, the incubation period for a cold is 1–3 days.
The symptoms of COVID-19 are similar in both children and adults. However, according to the Centers for Disease Control and Prevention (CDC), children typically present with fever and mild, cold-like symptoms, such as a runny nose and a cough.
The following table outlines the symptoms of COVID-19, the flu, and a cold.
Severity and mortality
The symptoms of COVID-19 and flu can range from mild to severe. Both can also cause pneumonia.
It is important to note that the World Health Organization (WHO) have classified mild symptoms of COVID-19 to mean that a person will not require hospitalization. The WHO classify mild cases to consist of symptoms including:
- fever
- cough
- fatigue
- loss of appetite
- sore throat
- headache
The CDC also lists the following as potential symptoms:
- breathlessness
- muscle pain
- chills
- new loss of taste or smell
According to the WHO, around 15% of COVID-19 cases are severe, and 5% are critical. Those in a critical state require a ventilator to breathe. The chance of severe and critical infection is higher with COVID-19 than the flu.
COVID-19 is also more deadly. According to the WHO, the mortality rate for COVID-19 appears to be higher than that of the flu.
Compared with the flu, research on COVID-19 is still in its early stages. These estimates may change over time.
Transmission
Both SARS-CoV-2 and the flu virus can spread through person to person contact.
Tiny droplets containing the viruses can pass from someone with the infection to someone else, typically through the nose and mouth through coughing and sneezing.
The virus can also live on surfaces. The WHO is not sure exactly how long the virus can survive, but it could be days.
According to the CDC, people can transmit the flu virus to people who are 6 feet (ft) away. According to the WHO, people should stay at least 6 ft away from anyone coughing or sneezing to help prevent the transmission of the SARS-CoV-2 infection.
According to the WHO, the speed of transmission differs between the two viruses. The symptoms of flu appear sooner, and it can spread faster than the SARS-CoV-2 virus.
The organization also indicate that people with flu can pass the virus on before they show any symptoms. A person can also pass on the SARS-CoV-2 infection even if they have no symptoms.
There are also differences in transmission between children and adults.
According to the WHO, the transmission of the flu from children to adults is common. However, based on early data it appears that it is more common for adults to pass the SARS-CoV-2 infection onto children. Children are less likely to develop symptoms.
The CDC recommend that people wear cloth face masks in public places where it is difficult to maintain physical distancing. This will help slow the spread of the virus from people who do not know that they have contracted it, including those who are asymptomatic. People should wear cloth face masks while continuing to practice physical distancing.
Treatment
As flu has been around much longer than COVID-19, there are more treatment options.
Most people with the flu do not require medical treatment. But a doctor might prescribe antiviral drugs in some cases, which can reduce the symptoms by 1–2 days.
These antiviral drugs help the body fight the virus. They treat symptoms and reduce how long the illness lasts.
There are currently no antiviral drugs approved to treat COVID-19, although scientists are currently researching drugs in trials. When scientists have had more time to study the disease, the availability of antivirals to treat COVID-19 will likely increase.
Although there is currently no approved treatment or vaccination for COVID-19, there are ways to help treat the symptoms and any complications that can occur.
For mild cases, a person should remain home and undertake social distancing. Healthcare professionals may prescribe antipyretics to reduce the fever.
For more severe cases, a person may require supplemental oxygen or mechanical ventilation on a breathing machine to treat the respiratory problems that may occur.
Prevention
The most effective way of preventing the flu is through vaccination.
Many strains of influenza can cause infection. The most common strains vary depending on the season.
Doctors will try to predict what strains will be most common each season to select the right vaccine components.
The best way to prevent spreading the SARS-CoV-2 virus includes:
- washing hands regularly
- avoiding touching the face
- keeping at least 6 ft away from anyone sneezing and coughing
- covering the mouth when sneezing or coughing
- staying at home if feeling unwell
- working from home if possible
- avoiding crowds and gatherings of any size
Causes
Both COVID-19 and the flu are viral infections.
Viruses are tiny microbes that survive by invading other living cells. These cells become host cells to the virus, which multiplies inside of them. They can then spread to new cells around the body.
Coronaviruses are a family of viruses that cause respiratory infections. The SARS-CoV-2 causes the infection that leads to COVID-19.
There are two types of viruses that cause the flu — influenza A and B. There are also several subtypes of influenza A. Any of these viruses can cause the flu.
Summary
COVID-19 and flu share some similar symptoms. The symptoms of flu tend to occur faster and can have greater variation. But COVID-19 is more likely to lead to severe illness or death.
Both viruses spread via person to person contact. Flu spreads faster and is more likely to affect children.
As the flu has been around longer, there are several effective antiviral treatments and vaccines available. Researchers and scientists are developing these for COVID-19, but treatments and vaccines are not likely to be available soon.
The best way to prevent COVID-19 is to practice social distancing, which means avoiding any non-essential social contact or travel. It is essential to maintain good personal and domestic hygiene by washing the hands regularly and keeping surfaces and utensils clean.
Viral infections cause both COVID-19 and the flu. But COVID-19 is due to the SARS-CoV-2 virus, and flu is from influenza A and B viruses.

How do COVID-19 vaccines compare with other existing vaccines?
The novelty of the COVID-19 vaccines may seem daunting for some, and it is natural for questions to arise on their effectiveness. In this feature, we examine the difference between effectiveness and efficacy, compare the COVID-19 frontrunner vaccines to other vaccines, such as the flu shot, and compare their safety considerations.
All data and statistics are based on publicly available data at the time of publication. Some information may be out of date. Visit our coronavirus hub and follow our live updates page for the most recent information on the COVID-19 pandemic.
As Pfizer/BioNTech roll out their COVID-19 vaccine throughout the United Kingdom and the United States, the world wonders how effective it will be.
Looking at the three leading vaccines that we have previously reported on, Pfizer/BioNTech boasts 95% efficacy, the Oxford/AstraZeneca vaccine candidate has an average of 70% efficacy, while the Moderna vaccine candidate reportedly has 94.1% efficacy.
Effectiveness vs. efficacy — what is the difference?
Firstly, it is worth noting that “effectiveness” and “efficacy” are not the same. Despite news outlets frequently using them interchangeably, efficacy refers to how a vaccine performs under ideal lab conditions, such as those in a clinical trial. In contrast, effectiveness refers to how it performs in the real world.
In other words, in a clinical trial, a 90% efficacy means that there are 90% fewer cases of disease in the group receiving the vaccine compared with the placebo group.
However, the participants chosen for a clinical trial tend to be healthier and younger than those in the general population, and they generally have no underlying conditions. Furthermore, researchers do not normally include certain groups in these studies, such as children or pregnant people.
So, while a vaccine can prevent disease in a trial, we might see this effectiveness drop when administered to the wider population.
However, that is not in itself a bad thing.
Pfizer study shows vaccine effective against new variant
Scientists recently identified two new strains of SARS-CoV-2 — one of which had been discovered in the United Kingdom and the other in South Africa. A new Pfizer study concludes that its vaccine should be effective against the U.K. variant.
Both new variants, which appear to be more contagious, have mutations in a spike protein called N501Y.
Because most vaccines currently under investigation essentially teach the immune system to respond to the spike proteins, some people have questioned whether the vaccines will be effective against the variants.
The new study, which appears on a preprint server, is a combined effort from Pfizer and scientists at the University of Texas Medical Branch at Galveston.
The researchers analyzed blood samples from 20 people who had received the Pfizer–BioNTech vaccine during previous clinical trials.
They demonstrated that antibodies from vaccine recipients successfully fought off a virus with the N501Y mutation. The study has limitations, though. For instance, the variant first identified in South Africa has an additional mutation known as E484K, which the new study did not address.
Importantly, the study has also not yet been peer-reviewed. Meanwhile, Pfizer’s chief scientific officer, Dr. Philip Dormitzer, acknowledges:
“It was a very reassuring finding that at least this mutation, which was one of the ones people are most concerned about, does not seem to be a problem.”
The authors of the preprint conclude: “The ongoing evolution of SARS-CoV-2 necessitates continuous monitoring of the significance of changes for vaccine coverage. This surveillance is accompanied by preparations for the possibility that a future mutation in SARS-CoV-2 might necessitate a vaccine strain change. Such a vaccine update would be facilitated by the flexibility of mRNA-based vaccine technology.”
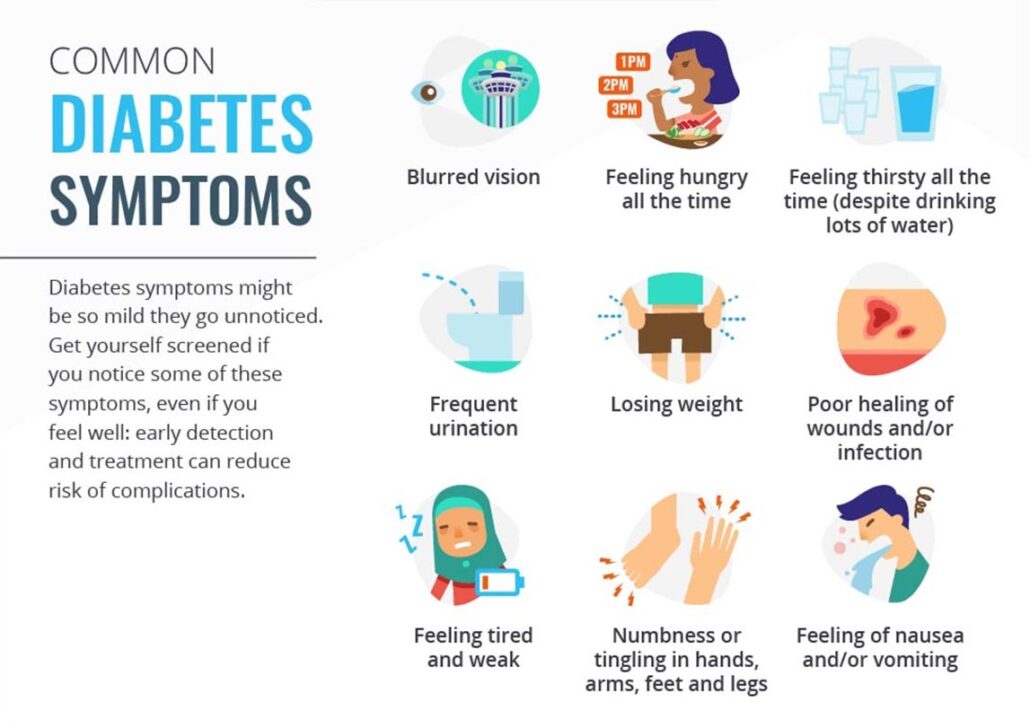
Medical myths: All about diabetes
Globally, diabetes is becoming increasingly prevalent, as are the myths and misconceptions that surround it. Here, we discuss 11 of these repeated untruths.
Currently, around 1 in 10 people in the United States have diabetes. Globally, more than 422 million people are living with the disease.
Although diabetes is a familiar word, symptoms vary, and the biological mechanisms involved are complex. Because it is both common and complicated, half-truths abound.
Unfortunately, some of the myths we cover in this article increase the stigma attached to diabetes. For this reason alone, it is essential to challenge these falsehoods.
Firstly, we will briefly explain what diabetes is and highlight the differences between the three most common forms of diabetes: type 1, type 2, and gestational diabetes.
Type 1 diabetes is an autoimmune disease in which the immune system attacks the pancreas cells that create insulin. It tends to occur earlier in life than type 2 diabetes. In type 2 diabetes, the body does not make enough insulin, does not respond well to insulin, or both.
At least 90% of people with diabetes in the U.S. have type 2.
Gestational diabetes, as the name suggests, occurs during pregnancy. During pregnancy, the body needs more insulin. Gestational diabetes occurs when the body cannot meet these new requirements.
Although gestational diabetes usually goes away after birth, there is a risk of developing it again during future pregnancies and developing type 2 diabetes later in life.
1. Eating sugar causes diabetes
Eating sugar does not directly cause diabetes. However, consuming a sugary diet can lead to overweight and obesity, which are risk factors for type 2 diabetes.
This is a common myth, perhaps understandably — blood sugar levels play an essential role in diabetes. Sugar itself, though, is not a causal factor.
As ever, the story is complex: there does appear to be a link between regularly drinking soda and risk for type 2 diabetes.
One large study published in 2013 found that, even after controlling for energy intake and body mass index (BMI), drinking soda has links with an increased risk of developing the disease. The study did not find this association in relation to other drinks, such as artificially-sweetened beverages and fruit juices.
Scientists still do not understand why some people develop type 1 diabetes, and others do not. However, nutrition is not a risk factor.
2. Diabetes is not serious
Perhaps because diabetes is so common, some people believe that it is not a serious disease. This is incorrect. There is no cure for diabetes, and there are a host of complications that can occur if a person does not manage the condition well.
Complications include cardiovascular disease, nerve damage, kidney damage, blindness, skin conditions, and hearing impairment.
In 2018, diabetes was the underlying cause of 84,946 deaths in the U.S. The World Health Organization estimate that diabetes caused the death of 1.6 million people in 2016.
3. Diabetes only affects people with obesity
Overweight and obesity are risk factors for type 2 diabetes and gestational diabetes, but the condition can occur in people of any weight. According to data from the Centers for Disease Control and Prevention (CDC) National Diabetes Statistic Report, 2020, 11% of people with type 2 diabetes in the U.S. are neither overweight nor obese.
Type 1 diabetes has no associations with body weight.
4. Obesity always leads to diabetes
Although obesity increases the risk of diabetes, it does not inevitably lead to the disease. According to the CDC, an estimated 39.8% of adults in the U.S. have obesity, but 13% have diabetes.
5. People with diabetes cannot eat sugar
People with diabetes certainly do need to manage their diets carefully: monitoring carbohydrate intake is important. However, they can still incorporate treats.
The American Diabetes Association explain:
“The key to sweets is to have a very small portion and save them for special occasions, so you focus your meals on healthier foods.”
Individuals with diabetes need to carefully plan what and when they will eat to ensure that their blood sugar levels remain balanced.
A related myth is that people with diabetes need to eat special “diabetes-friendly” foods. These products are often more expensive, and some can still raise glucose levels.
6. Diabetes always leads to blindness and amputation
Thankfully, this is a myth. While it is true that diabetes can lead to blindness and amputations in some cases, it is not inevitable. And for individuals who manage their condition carefully, these outcomes are rare.
The CDC estimate that 11.7% of adults with diabetes have some level of vision impairment. Lower-extremity amputation occurs in around 0.56% of people with diabetes in the U.S.
Experts have identified several risk factors that increase the likelihood of experiencing diabetes-related complications. These include obesity and overweight, smoking, physical inactivity, high blood pressure, and high cholesterol.
7. People with diabetes should not drive
A diabetes diagnosis does not automatically mean that someone needs to stop driving. In a position statement on diabetes and driving, the American Diabetes Association explain:
“Most people with diabetes safely operate motor vehicles without creating any meaningful risk of injury to themselves or others.”
However, they also explain that, if concerns arise, people should undergo assessment on an individual basis. According to the U.S. Department of Transportation:
“People with diabetes are able to drive unless they are limited by certain complications of diabetes. These include severely low blood glucose levels or vision problems. If you are experiencing diabetes-related complications, you should work closely with your diabetes healthcare team to find out if diabetes affects your ability to drive.”
8. Prediabetes always leads to diabetes
In the U.S., an estimated 88 million, or 1 in 3, adults have prediabetes. Prediabetes is a condition where blood sugar levels are higher than normal but not quite high enough to classify as diabetes. If left unchecked, prediabetes can develop into type 2 diabetes.
However, it is not a given. Lifestyle changes can turn the tide. Regular physical activity and a more healthful diet can stop diabetes in its tracks.
9. People with diabetes cannot be active
Once again, this is untrue. In fact, exercise is an important component in the management of diabetes. Among other things, exercise helps drive weight loss and reduces blood pressure, both of which are risk factors for complications. It can also help the body use insulin better.
However, exercise can impact blood sugar levels in various ways, sometimes increasing it and, at other times, decreasing it.
According to Diabetes U.K., “Some days, you’ll do exactly the same type of activity and eat the same foods, but your blood sugar levels may act differently to what you’d expect.”
They also offer tips for managing blood sugar during activity:
- Check your blood sugar while exercising and keep a record of how it behaves to show your doctor. This can help guide any necessary changes in insulin.
- For people who are at risk of hypos, keep fast-acting carbohydrates close to hand.
- Wear diabetes identification so that people can help if needed.
10. You can ‘catch’ diabetes
This is a myth. Pathogens do not cause diabetes, so a person cannot pass it to someone else. Doctors classify it as a noncommunicable disease.
11. Some natural products cure diabetes
Currently, there is no cure for diabetes. Any claims that a product can cure diabetes are false. Many herbal or natural products will do little or nothing and, in some cases, they can potentially cause harm; diabetes.co.uk explain:
“Because certain herbs, vitamins, and supplements may interact with diabetes medications (including insulin) and increase their hypoglycemic effects, it is often argued that using natural therapies could reduce blood sugars to dangerously low levels and raise the risk of other diabetes complications.”
Diabetes is a complex but common disease. As its prevalence increases, it is essential to overturn myths as we find them.