High blood pressure research
In this special feature, we collate some of the most intriguing hypertension studies from 2019. We particularly focus on nutrition, risk factors, and hypertension’s relationship with dementia.
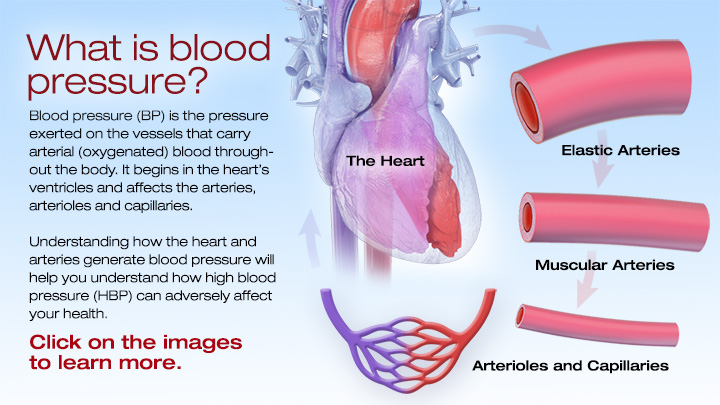
Today, in the United States, around 1 in 3 adults has high blood pressure, which doctors also call hypertension.
Hypertension increases the risk of cardiovascular events, such as stroke and coronary disease, and, if doctors don’t treat it, it can reduce lifespan.
Because it is worryingly prevalent, and because the physical ramifications can be significant, scientists are plowing a great deal of effort into understanding hypertension.
Although people first identified hypertension as a medical condition thousands of years ago, scientists are still picking away at the details.
Research that scientists completed in 2019 has thrown out some exciting and, in some cases, unexpected findings. For instance, a paper appearing in February concluded that, for women over 80 years of age, having “normal” blood pressure had an increased risk of mortality when compared with individuals with high blood pressure.
Elsewhere, Greek scientists concluded that napping might help reduce blood pressure. “Midday sleep appears to lower blood pressure levels at the same magnitude as other lifestyle changes,” explains one of the researchers, Dr. Manolis Kallistratos.
Another surprising study, which scientists presented at the 83rd Annual Scientific Meeting of the Japanese Circulation Society, concluded that needing to urinate multiple times at night might be a sign of hypertension.
The role of nutrition
The food that we eat has a huge impact on our overall health; that goes without saying. The America Heart Association, for instance, suggest that eating a diet rich in fruits and vegetables and avoiding products with high levels of salt and fat can help keep blood pressure in check.
Over the past few years, interest in nutrition, in general, has skyrocketed. More and more, scientists are focusing on individual foods or food compounds that can directly benefit health. So, although poor diet is a well-known risk factor for hypertension, researchers in 2019 drilled down deeper.
Specific foods and supplements
One study appearing in 2019 investigated the impact of consuming walnuts on blood pressure. It concluded that the individuals who ate an experimental walnut-heavy diet experienced a significant reduction in blood pressure.
In these types of studies, it is worth digging a little deeper; often, industry or organizations who might stand to benefit from positive results are funding them. The walnut study above, for instance, was partly funded by the California Walnut Commission.
This observation does not mean that we should dismiss the results out of hand, but it provides pause for thought.
Another recent study concentrated on spirulina, which is the dried biomass of a bacterium called Spirulina platensis. Manufacturers can add it to foods, and some people take it as a supplement.
Earlier experiments hinted at spirulina’s potential to reduce hypertension, and in the most recent study, they attempted to find out why this might be.
The scientists concluded that a protein that the digestion of spirulina produces causes blood vessels to relax. The authors hope that this protein, known as SP6, might one day be useful in the treatment of hypertension.
Preservatives, additives, and water
Rather than focus on specific foods, a further study looked at the impact of buying food from local retailers rather than supermarkets.
The authors theorized that by eating local produce, individuals would avoid consuming the various preservatives and additives that keep food “fresh” over long distances.
Although the study was relatively small, the authors found that after 6 months, those who consumed local produce had lower levels of visceral fat, improved depression scores, and reduced systolic blood pressure.
Approaching from a different angle, a team of scientists recently asked whether drinking water that is high in minerals might reduce blood pressure.
To investigate, they focused on people living in a coastal region of Bangladesh. Drinking water there varies in salinity. In areas of high salinity, the water contains greater quantities of sodium, which we know increases blood pressure. However, the same water also includes more magnesium and calcium, both of which reduce blood pressure.
The authors concluded that higher salinity levels decreased blood pressure overall; they write that “the [blood pressure]-lowering effects of [calcium] and [magnesium] counteracted the harmful effects of [sodium].
Causes and risk factors
Some risk factors for hypertension are fairly well established; they include drinking excessive amounts of alcohol, smoking tobacco, stress, and obesity. However, because high blood pressure is so common, there are likely to be many more factors at play.
Similarly, although scientists know which lifestyle and dietary factors influence blood pressure, they are not entirely sure how they cause the changes.
Understanding why and how blood pressure arises in some people and not others is essential and could, potentially, lead to innovative ways of treating or preventing hypertension.
Some scientists are exploring possible risk factors which, at face value, seem unlikely. For instance, one paper, appearing in the Journal of Public Health in June, examined the role of where people live.
Earlier studies found an association between exposure to air pollution and hypertension risk, and this latest work confirms those earlier suspicions and takes it a step further.
As expected, the researchers found a relationship between air pollution and hypertension; however, the increase in risk was only significant for those who were living in multi-family homes, such as blocks of flats.
The authors believe that this might be due to several factors, for instance, living in close quarters with other people may be more stressful or more noisy. This study provides a glimpse of the complex realm of potential elements that might influence blood pressure.
Oral hygiene
Bizarrely, one group of scientists recently investigated how mouthwash might influence hypertension risk.
Publishing their findings in the journal Frontiers in Cellular and Infection Microbiology, the authors conclude that mouthwash kills “good bacteria” in the mouth. These good bacteria produce nitric oxide (NO), which is important for blood vessel health.
NO acts as a vasodilator, which means it causes the muscles that line blood vessels to relax, thereby widening the vessels and reducing blood pressure.
In particular, the scientists concentrated on the chemical chlorhexidine, which they found in some mouthwashes.
According to the authors, they demonstrated that “twice-daily chlorhexidine usage was associated with a significant increase in systolic blood pressure after 1 week of use, and recovery from use resulted in an enrichment in nitrate-reducing bacteria on the tongue.”
Still focusing on the oral region, a 2019 review looked for links between gum disease and hypertension. They showed that individuals with severe periodontitis — a form of gum disease — had a 49% increased risk of hypertension.
Senior author Prof. Francesco D’Aiuto explains their results in a nutshell: “We observed a linear association — the more severe periodontitis is, the higher the probability of hypertension.”
The role of zinc
Another project investigated the role of zinc in maintaining blood pressure at healthy levels. Over the years, researchers have noted links between low zinc levels and an increased risk of high blood pressure, but the precise mechanism has been tough to pin down.
The latest research identified the key player in this interaction between zinc and blood pressure; according to the authors, the sodium chloride cotransporter (NCC) in the kidney is the lynchpin. The NCC is responsible for pumping sodium back into the body, thereby preventing it from being excreted in the urine.
Zinc interacts with the NCC: when zinc is present, the NCC is less active, meaning that the body retains less sodium. This is important because high sodium levels — from consuming too much salt, for instance — are factors in increasing the risk of hypertension.
The authors hope that this new knowledge will help improve treatment and write:
“Understanding the specific mechanisms by which [zinc deficiency] contributes to [blood pressure] dysregulation may have an important effect on the treatment of hypertension in chronic disease settings.”
Hypertension and dementia
Scientists have identified a relationship between hypertension and vascular dementia. The association makes sense because vascular dementia can occur following stroke, and hypertension is a risk factor for stroke.
However, it also appears that hypertension might increase the risk of other types of dementia, including Alzheimer’s disease.
A study appearing in June this year found that a common blood pressure drug — nilvadipine — slowed the progress of Alzheimer’s disease by improving blood flow in the brain.
Specifically, the research team showed that people who took the medication had a 20% increase in blood flow in the hippocampus, a brain region vital for memory and learning, in comparison to those who did not take nilvadipine.
Patterns throughout life
Other scientists have looked at fluctuations in blood pressure and their possible role in dementia. For instance, one investigation that recruited participants who were living with Alzheimer’s disease found that the condition progressed quicker in those whose blood pressure fluctuated most.
“More fluctuations [in blood pressure] might affect whether cognitive function declines more slowly or rapidly.”
Senior author Dr. Jurgen Claassen
With a similar theme, another group of scientists observed the pattern of blood pressure across decades. The authors summarize their findings:
“[A] pattern of sustained hypertension from middle to late life and a pattern of midlife hypertension followed by late-life hypotension were associated with an increased risk for subsequent dementia, compared with participants who maintained normal blood pressure.”
Another project that charted hypertension over a lifespan found that individuals with high or rising blood pressure between 36 and 53 years of age were more likely to have white matter lesions and a smaller brain volume in later life.
The authors hope that these findings will inspire both doctors and the public to check and take charge of their blood pressure sooner rather than later.
As 2020 rolls into view, hypertension is sure to stay high on the medical research agenda. As science gradually untangles hypertension’s causes and mechanisms, managing and minimizing this highly prevalent condition must draw ever closer.
New Year’s resolutions: How to boost success rates
Do we make New Year’s resolutions just to ignore them? Are they merely promises doomed to fail? In this feature, we ask whether, statistically speaking, these resolutions work, and what increases the chances of success.
New Year’s resolutions are an ancient tradition that continues to this day.
The Babylonians started each year with pledges to pay debts and return borrowed items.
The Romans began their year by promising the two faced god, Janus, that they would behave better.
In modern societies, many people still promise to make changes as the new year dawns; this desire, in many cases, is fueled by the excesses of the holiday period.
Most commonly, it would seem, New Year’s resolutions revolve around weight loss, quitting smoking, reducing drinking, and exercising more.
How effective are annual resolutions?
A study from 1989 tracked 200 people living in Pennsylvania as they attempted to make changes based on New Year’s resolutions.
On average, the participants made 1.8 resolutions, most commonly, to stop smoking or lose weight. Less frequently, people pledged to improve relationships, and a surprisingly low 2.5% were hoping to control their drinking habits.
An impressive 77% managed to hold to their pledges for 1 week, but the success rate dropped to 19% over 2 years. Although that is a substantial drop out rate, it means that 1 in 5 of those participants achieved their goal.
Of the 77% successful resolvers, more than half slipped at least once, and, on average, people slipped 14 times across the 2 years.
A study in the Journal of Consulting and Clinical Psychology in 1988 followed the efforts of 153 New Year’s resolvers who were determined to quit smoking.
At 1 month, 77% of participants had managed at least one 24-hour period of abstinence. Overall, though, the results seemed a little disappointing with the authors writing:
“Only 13% of the sample was abstinent at 1 year, and 19% reported abstinence at the 2-year follow-up.”
Another study, appearing in PLOS ONE, took a more general look at behavior. The research team tracked the food shopping habits of 207 households from July 2010 to March 2011.
Unsurprisingly, the researchers found that, during the holiday period, expenditure increased by 15%. Three-quarters of this increase went on less healthful items.
Also, as expected, when January rolled around, the sale of healthful items shot up by 29.4%.
However, the sale of less healthful items did not drop in tandem with this health drive — people were buying more nutritious items, but still purchasing the same amount of unhealthful food.
Overall, the number of calories they purchased in the New Year was higher than during the holiday period. The authors conclude:
“Despite resolutions to eat more healthfully after New Year’s, consumers may adjust to a new ‘status quo’ of increased less-health[ful] food purchasing during the holidays, and dubiously fulfill their New Year’s resolutions by spending more on health[ful] foods.”
The authors believe that the key to successful resolutions is to focus on replacing unhealthful items with healthful ones, rather than buying both.
That is sound advice, but not necessarily easy to implement.
Successes and failures of weight loss goals
In 2009, GlaxoSmithKline released Orlistat, which they hailed as “the first clinically proven over-the-counter weight loss aid” in Europe.
As part of their marketing push, the company also conducted an internet survey about weight loss that included questions about New Year’s resolutions.
Although the survey was not meant to be a scientific study, it generated a substantial pool of data with 12,410 females from six European countries responding.
A group of researchers took advantage of this dataset and published an analysis in the journal Obesity Facts.
They found that around half of the women had made a weight loss New Year’s resolution in the past 2 years.
As for success rates, they observed that women with a body mass index (BMI) of under 25, which health experts define as “normal,” were successful 20% of the time.
However, of thos with a BMI of 30 or above — which doctors class as overweight or obese — only 9% reported some success.
In the overweight group, three-quarters of the female respondents said that their primary reason for failing to lose weight was that it took too long to see results. Around one-third of those who were obese or overweight stated that they were not successful due to a lack of confidence.
What increases the chances of succeeding?
In the Pennsylvania study we mention above, the scientists found no link between success rate and participants’ sex or age; similarly, the type of resolution did not influence how likely they were to succeed.
The researchers contacted participants by telephone after 1 week, 1 month, 3 months, 6 months, and 2 years.
During these interviews, the researchers also asked participants what techniques they used to help them keep their resolutions, and how often they implemented each one.
They found that the most successful resolvers were applying stimulus control at all five checkpoints.
Stimulus control is the act of keeping things around you that remind you why you chose the resolution.
For instance, someone who is quitting smoking might keep a picture of their young child nearby to remind them why they decided to stop.
At the 6-month and 2-year mark, successful resolvers were using self-liberation (or willpower), and reinforcement management — rewarding themselves for being successful.
Conversely, individuals who did not keep their resolutions most commonly employed self-blame and wishful thinking.
The study we highlighted above that followed the fates of 153 smokers also looked at factors that made quitting more likely. The authors explain:
“The use of multiple strategies for cessation was associated with abstinence at the 2-year follow-up. A strong motivation to quit was found to be important for both initial success and long-term maintenance.”
Other studies that have investigated smoking cessation more generally have identified factors that increase the chance of quitting. These factors include staying away from smokey environments, abstaining from alcohol, stress management techniques, and will power.
Another paper took a different approach. Publishing their work in the Journal of Clinical Psychology, the authors set out to understand why some people succeeded where others failed.
To do this, they recruited two sets of participants: 159 New Year’s resolvers and 123 people who were interested in solving a problem at a later date. The researchers followed the participants for 6 months and charted their successes and failures.
In agreement with other studies, the most common reasons for New Year’s resolutions were losing weight, increasing exercise, and quitting smoking.
The authors found that the most successful resolvers used more willpower, stimulus control, reinforcement management, positive thinking, and avoidance strategies.
Conversely, those who were less successful tended to use more wishful thinking, blame and criticize themselves, and make light of the problem.
Ending on a high
Some of the results above might cast a shadow across ambitions to make a change in 2020, but they shouldn’t.
The authors of the study above made some overarching conclusions that should boost the confidence of any New Year’s resolver:
“Resolvers reported higher rates of success than nonresolvers; at 6 months, 46% of the resolvers were continuously successful compared to 4% of the nonresolvers.”
So, although the cards might be stacked against anyone who plans to make a New Year’s resolution, simply by making that resolution, you have boosted your odds of success.
According to this data, forming a New Year’s resolution increases your chances of generating change more than 10-fold.
The authors write that, “Contrary to widespread public opinion, a considerable proportion of New Year resolvers do, in fact, succeed, at least in the short run.”
In conclusion, New Year’s resolutions do not work for everyone. But, as the saying goes, “you’ve got to be in it to win it.”
If you are considering making a resolution for 2020, according to the findings of these studies, the best approach is to keep things around you to remind you why you want to make those changes.
Also, reward yourself for successes, and stay motivated. Throw a healthful dose of willpower into the seasonal mix, and you are likely to succeed. Good luck!

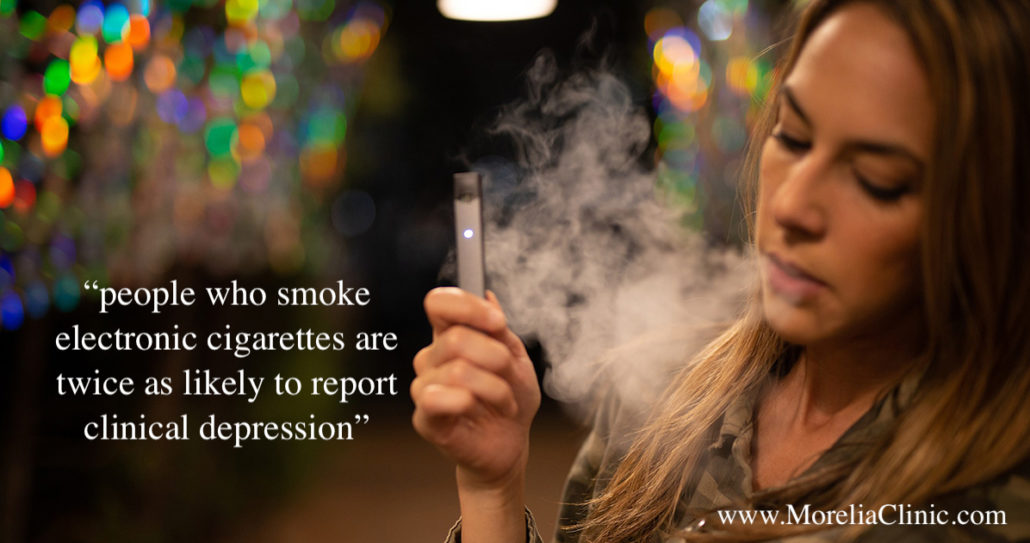
A new study identifies a link between vaping and depression.
A recent study concludes that people who smoke electronic cigarettes are twice as likely to report clinical depression as those who have never vaped. The correlation was particularly strong among younger people.
Known as vaping, battery-powered e-cigarettes use heat to deliver an aerosol cocktail of nicotine and flavors to the user. An e-cigarette produces a small cloud of vapor, whereas a cigarette releases smoke.
Many people believe that the vapor contains water. In fact, it contains varying amounts of toxic chemicals that have links to heart and respiratory diseases, as well as cancer.
The use of e-cigarettes in the United States has snowballed since their introduction a decade ago.
According to the Annals of Internal Medicine
in 2016, an estimated 10.8 million people in the U.S. used e-cigarettes. Of this number, 2.8 million (9.2%) were 18–24 years old.
Today, some experts consider vaping to be an epidemic among teenagers — the number of high school students who turned to vaping doubled in 2018.
Although links between traditional cigarettes and depression primarily prompted the study, the results of an earlier study that indicated that 9.1% of those with depression were e-cigarette users, compared with 4.5% among the general population was also a factor.
First author of the study, Dr. Olufunmilayo Obisesan of John Hopkins University in Baltimore, MD, told Medical News Today that “Combustible cigarette smoking has been linked with an increased risk of developing major depressive disorder and has also been shown to be highly predictive of future suicidal behavior among individuals with a history of depression.”
“In light of the similarities in some of the constituents of cigarettes and e-cigarettes, we decided to explore the existence of a similar association between e-cigarettes and depression.”
Concerns for youngsters who vape
The study looked at the responses of nearly 900,000 randomly sampled adults aged 18 and older in a cross-sectional study of 2016–2017 data gathered by the Behavioral Risk Factor Surveillance System (BRFSS)
The BRFSS is the largest national telephone survey carried out in the U.S.
“The researchers found that 34% of current e-cigarette users reported having experienced clinical depression, compared with 15% of those who had never vaped. Also, 27% of former users were more likely to report clinical depression, compared with 15% in those who had never used e-cigarettes.
College students aged 18–25 showed the most significant link between e-cigarette use and depression.
The scientists focused on this group in particular because, typically, young people are more likely to experiment with new products, such as e-cigarettes. Tobacco companies often target this demographic in marketing campaigns.
“This highlights the potential susceptibility of e-cigarette users in this group to depression at a particularly vulnerable time in their lives, but also warrants pause in what this kind of nicotine addiction may be doing to our children, high schoolers, and younger, who we know are using e-cigarettes in epidemic proportions,” says Dr. Mariell Jessup of the American Heart Association’s (AHA) Tobacco Center of Regulatory Science.
The AHA has launched a major initiative to tackle youth e-cigarette use and nicotine addiction.
“The main implication of our findings for the youth is that they need to know that there are potential mental health effects associated with the use of e-cigarettes.”
Dr. Olufunmilayo Obisesan
Depression risk rises with increased use
The study also found that the link between e-cigarette use and depression was stronger in people who vaped the most often.
“Clinically, our study provides information that physicians could consider when counseling patients seeking information about e-cigarettes, especially those with depression,” Dr. Obisesan told MNT.
He added that the study emphasized the need for doctors and health professionals to routinely collect information on e-cigarette from individuals during clinic visits, especially among those with mental health conditions. In conclusion, Dr. Obisesan told MNT:
“We hope that our study will provide a baseline for future longitudinal studies that can confirm our findings and establish the direction of association between e-cigarette use and depression, which we currently believe to be bi-directional.”
New evidence suggests that being physically active could help slash prostate cancer risk.
Researchers using a new method of assessing risk factors for prostate cancer have found an intriguing link between a lack of physical activity and an increased risk of this condition.
According to data from the National Cancer Institute (NCI), by the end of 2019, there will have been an estimated 174,650 new cases of prostate cancer in the U.S. alone.
Despite the number of people that this cancer affects every year, specialists still have insufficient knowledge about the risk factors that may play a role in its development.
The NCI cite a mix of modifiable and nonmodifiable factors, including age, a family history of prostate cancer, and the levels of vitamin E, folic acid, and calcium in the body.
Yet there may be other lifestyle-related factors at play, and investigators are hard at work to uncover them.
Recently, a team of researchers from the University of Bristol and Imperial College London in the United Kingdom — alongside colleagues from other academic institutions across the globe — have used a different approach to try to find out more about prostate cancer risk factors.
In their new study, the findings of which now appear in the International Journal of Epidemiology, the investigators used a method called “Mendelian randomization.”
Mendelian randomization
allows researchers to look at genetic variations to assess causal relationships between various potential risk factors and the development of certain outcomes — in this case, prostate cancer.
Physical activity may more than halve risk
In their study, the researchers identified potential risk factors for prostate cancer through the World Cancer Research Fund’s (WCRF) 2018 systematic review of the evidence.
They also had access to the medical information of 79,148 participants with prostate cancer, as well as 61,106 participants without cancer who acted as the controls.
The analysis revealed that individuals with a genetic variation that increased their likelihood of being physically active had a 51% lower risk of prostate cancer than people who did not have this genetic variation.
Moreover, the researchers explain that “physical activity,” in this case, refers to all forms of activity, not just exercise.
Following on from this, the study authors conclude that interventions encouraging males to ramp up their levels of physical activity may have a protective effect against this widespread form of cancer.
“This study is the largest-ever of its kind, which uses a relatively new method that complements current observational research to discover what causes prostate cancer,” notes study co-author Sarah Lewis, Ph.D.
“It suggests that there could be a larger effect of physical activity on prostate cancer than previously thought, so will hopefully encourage men to be more active.”
Sarah Lewis, Ph.D.
Anna Diaz Font, who is head of research funding at WCRF — which, alongside Cancer Research U.K., funded this study — emphasizes the importance of the current findings.
“Up till now, there has only been limited evidence of an effect of physical activity on prostate cancer. This new study looked at the effect of 22 risk factors on prostate cancer, but the results for physical activity were the most striking,” she says.
The study’s findings, Diaz Font believes, “will pave the way for even more research, where similar methods could be applied to other lifestyle factors, to help identify ways men can reduce their risk of prostate cancer.”

What is the difference between cold and flu?
Both flu (influenza) and cold are caused by viruses, and they can have similar symptoms. So how do we know if a person has the flu or a bad cold? In this article, we explain the differences.
Cold and influenza are the most common illnesses in humans.
. Every year, 5-20 percent of the population of America develop flu symptoms.
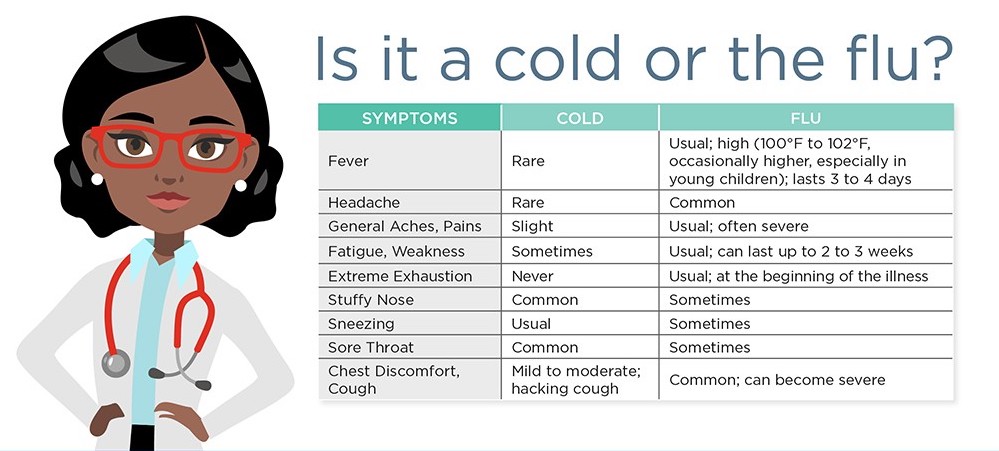
The main difference between cold and flu is that, generally, symptoms of the flu are usually a lot more severe.
Each year, more than 200,000 people are hospitalized because of flu complications; flu is responsible for around 23,600 deaths every year.
Fast facts on colds vs. flu:
- Colds and flu share many of the same symptoms; the major difference being flu is often worse, and accompanied by a high fever.
- According to the Centers for Disease Control and Prevention (CDC), the average adult will have 2-3 colds every year.
- The rhinovirus is the most common cause of cold.
The difference between cold and flu
Cold and flu are caused by different viruses, and, in general, the symptoms of flu are worse. Also, there are less likely to be serious complications from cold, such as pneumonia and bacterial infections.
The main difference between cold and flu symptoms is that flu more commonly includes fever; the fever can be 100 degrees Fahrenheit or higher and last for 3-5 days.
The extreme fatigue associated with flu can persist for weeks. Cold symptoms are generally milder and last about 1 week.
Also, runny nose or nasal congestion is more common with cold than flu.
Vomiting is another key difference; vomiting is not normally associated with the common cold but can be present in flu.
Although the differences above are generally true, without conducting special tests, it is impossible to know for sure whether it is flu or cold. For instance, it is possible to have flu without fever.
What is a cold?
Almost everybody is familiar with the sensation of having a cold. Colds affect both warm and cool climates equally, and the average person will have had many colds from infancy all the way until later life.
Symptoms include a runny nose, sore throat, coughing and sneezing, watery eyes, a headache, and body aches. There is no cure, except for resting and drinking plenty of fluids, but the cold should pass within 7-10 days.
There is normally no need to visit a doctor, but a person with a weakened immune system is more prone to developing pneumonia as a complication
To avoid catching or spreading a cold, people should wash their hands regularly and make sure they sneeze into a tissue or handkerchief, or into their elbow. This is the most hygienic as it stops the spread of germs, which cannot live on clothing or surfaces like they can on skin.
What is flu?
There are three types of flu virus, influenza A, influenza B, and influenza C. Types A and B are the ones that cause seasonal epidemics. One of the key symptoms of flu is feeling feverish or having a temperature of 100 degrees Fahrenheit or above. However, not everyone with the flu will have a fever.
Other symptoms include:
- headaches or body aches
- vomiting, nausea, and possibly diarrhea, especially in children
- a sore throat and a cough
- fatigue
- chills and shivering
- a congested or runny nose
A common cold is less likely to cause a high fever. With a cold, symptoms such as a runny nose or throat irritation will normally improve within a few days.
How to treat flu
The CDC note that the majority of people who have the flu do not need medical attention. Most can remain at home and avoid contact with other people to prevent the disease from spreading. However, the following treatments are available:
- Over-the-counter medications – these can reduce fever. Tylenol can help people with flu feel more comfortable while they recover. Tylenol is also available to purchase online.
- Prescription antiviral flu drugs – these are also available from a physician. They are for people who are at high risk of serious complications and are not normally necessary for effective treatment. They can only be given within a certain amount of time from symptom onset.
- Home remedies – to alleviate symptoms, home remedies such as steam inhalation, nourishing foods like chicken soup, keeping warm, and other comfort measures can be used.
A physician will be able to decide if antivirals are needed. People who tend to be at greater risk include infants under the age of 2, people aged 65 years and older, and pregnant women.
Emergency warning signs for flu
Patients should seek medical help if they notice any of the emergency warning signs.
Warning signs in infants include difficulty breathing, having no appetite, and not producing tears when they cry, or having fewer wet diapers than usual.
Severe symptoms in older children include:
- breathing problems
- bluish skin color
- not drinking enough fluids
- not waking up or interacting
- being so irritable that they do not want to be held
- fever with a rash
If flu-like symptoms improve but then return with fever and a worse cough, the parent should consult a physician.
Anti-flu vaccines and other types of protection
The best way to protect against the flu is by having an annual vaccination, as this helps the body to build up the immune system so that it can fight off the virus more quickly.
The flu vaccine is recommended during pregnancy as it has been proven safe. If flu occurs during pregnancy, it can have serious complications for the unborn child and the mother.
Vulvodynia: What you need to know
Vulvodynia and vestibulodynia refer to a chronic discomfort of the vulva, the part of a woman’s body that protects the genitals.
It includes the external female genitalia, including the mons pubis, the labia majora and minora, the clitoris, and the perineum.
Vulval pain can happen for a number of reasons, but vulvodynia and vestibulodynia are specifically linked to a hypersensitivity of the nerve endings in the skin.
Around 16 percent of women are estimated to have experienced pain or stinging in the vulval area at some time in their life.
Treatment
Treatment aims to alleviate symptoms. As the cause is unknown, finding a solution that works may take some trial and error.
Medications to block pain may include antidepressants, anticonvulsants, or serotonin-norepinephrine reuptake inhibitors (SNRIs).
Other solutions include creams, lotions, and anesthetic gel for applying to the vulval area.
Examples include topical hormone creams containing estrogen and testosterone, topical anesthetics, such as lidocaine, and products that contain an antidepressant or anticonvulsant ingredient. These can be applied 15 to 20 minutes before sexual activity, or when needed. Some of these products are available for purchase online, including lidocaine.
A nerve block is an anesthetic drug that is injected into the nerves that transmit pain signals, in this case, from the vulva to the spine. Interrupting the pain signals in this way can provide short-term relief.
If no other method is effective, surgery to remove the painful tissue may be appropriate.
Two techniques that are currently being investigated are neurostimulation and the spinal infusion pump.
Neurostimulation involves delivering low-voltage electrical stimulation to a specific nerve. This can replace pain with a tingling sensation.
A spinal infusion pump is an implanted device that can deliver low-dose medication to the spinal cord and nerve roots. This can dull pain.
However, there is limited evidence regarding the use of these measures for vulvodynia.
Some researchers have found that physical and psychosexual therapy can help improve sexual functioning, for example, by helping to reverse a fear of touch.
Symptoms
Vulvodynia features a burning, stinging, itching, irritating, or a raw feeling in the vulvar tissue, which may or may not appear inflamed. Patients may describe a feeling of throbbing, itching, aching, soreness, and swelling.
The pain can affect a particular spot, or it may be felt in a wider area, including the clitoris, the perineum, the mons pubis, and the inner thighs. It can also affect the area around the urethra and the top of the legs and inner thighs.
The pain involved in vulvodynia is neuropathic, which means it stems from abnormal signals from the nerve fibers in the vulval area. The nerve endings are hypersensitive.
It may be constant or intermittent. A constant pain that happens when there is no touch or pressure is known as unprovoked vulvodynia.
Vestibulodynia, previously known as vestibulitis, involves a pain that is triggered by light touch, or provoked pain.
Symptoms may be worse during or after sexual intercourse, walking, sitting, or exercising. It can happen when inserting a tampon, or when prolonged pressure is applied, for example, during horseback riding.
Vulvodynia is usually defined as lasting for at least 3 months. It often starts suddenly, and it may last for months or years. It is not life-threatening, but the pain can prevent the individual from carrying out some normal activities. This can also lead to upset or depression.
Complications
Relationship problems can result, because sexual intercourse is painful. One study suggests that 60 percent of women with vulvodynia are unable to engage in sex.
Studies suggest
that women who have vulvodynia can have a normal pregnancy, and that in some cases, pain levels fall during pregnancy. However, women with the condition are more likely to have a cesarean delivery.
Home remedies
Some measures can be taken that do not involve medications.
If vulvodynia occurs, the first step is to stop using any irritants, such as perfumed soaps. A change in menstrual products might help, for example, switching from synthetic to cotton-based items.
Cool gel packs may offer immediate, short-term pain relief. A range of cool gel packs is available for purchase online.
Pelvic floor muscle exercises may help by relaxing tissues in the pelvic floor and releasing tension in muscles and joints.
Biofeedback uses technology to increase an individual’s awareness of how they might be stressing their body. This information can help people change habits that lead to harm or discomfort. For women with vulvodynia, it can help strengthen the pelvic floor muscles, and this may reduce pain.
A trigger point is a specific area of discomfort. Trigger-point therapy involves massaging a small area of tightly contracted muscle to release tension and relieve pain. An anesthetic medication applied directly, for example, as a cream, can also be used to relieve pain in a trigger point.
Since stress can play a role in vulvodynia, either as a trigger or a consequence, stress management may help ease symptoms.
Acupuncture and cognitive behavior therapy are options currently being explored.
Diet
A change in diet may help. Cutting out one food at a time may help to pinpoint a trigger.
Items that commonly trigger a reaction include:
- caffeine
- high-sugar foods
- acidic foods
- processed foods
Causes
Vulvar pain can be caused by infections, neurological problems, inflammatory conditions, and neoplasms, such as squamous cell carcinoma.
Vulvodynia is not related to an underlying condition. The exact cause is unknown. It is not caused by a sexually transmitted or other infection, skin disease, or cancer, although these can also cause pain.
Factors that may raise the risk of vulvodynia include:
- Damage to or irritation of the nerves around the vulva
- A high density of pain-sensing nerve fibers in the vulval area
- High levels of inflammatory substances in the vulval area, for example, because of inflammation
- genetic susceptibility
- pelvic floor muscles are weak or unstable
- unusual or long-term reaction to infection, trauma, or another environmental factor
- changes triggered by hormones
Other factors that increase susceptibility include:
- frequent yeast infections
- sexually transmitted infections (STIs)
- chemical irritation of the external genitals, caused by soaps, feminine hygiene products or detergents in clothing
- rashes on the genital area
- previous laser treatments or surgery on the external genitals
- nerve irritation, injury or muscle spasms in the pelvic area
- diabetes
- precancerous or cancerous conditions on the cervix
Provoked vestibulodynia could result from:
- sexual intercourse
- tampon insertion
- a gynecologic examination
- prolonged sitting
- wearing tight underclothes or pants
- activities such as cycling or horseback riding
Clitorodynia refers to pain in the clitoris.
Vulvodynia can be confused with other vulvovaginal problems, such as chronic tension or spasm of the muscles of the vulvar area called vaginismus.
Prevention
Measures that can reduce the risk of triggering pain include:
- wearing cotton underwear and loose-fitting clothes around the genital area
- avoiding scented toilet paper and perfumed creams and soaps
- avoiding friction or sitting for prolonged periods
- refraining from excessive genital washing
- not douching or using vaginal wipes
- using water-soluble lubricants during sexual intercourse
- patting the area dry after rinsing or urinating
If a vaginal infection is suspected, it is important to have it diagnosed and treated promptly and to discuss with a physician if any treatments appear to make the condition worse.
Diagnosis
Diagnosis may involve a pelvic exam, to look for skin changes and assess the pain.
A cotton swab test is used to delineate the areas of pain and categorize their severity. The physician may press with swab on different areas while asking the patient to rate the level of pain.
The patient should be ready to describe the pain, including the type of pain and its severity, say when it started, and whether it began gradually or suddenly, where it hurts, and how often.
The doctor may use a special magnifying glass, to carry out a colposcopy.
Tests may be carried out to try to find the source of the pain and to eliminate other causes.
These include:
- taking a culture for bacteria and yeast
- blood tests to assess levels of estrogen, progesterone, and testosterone
- a biopsy
In a biopsy, the doctor first numbs the genital area with a painkiller, and then a small piece of tissue is taken for examination under a microscope.

