Medical myths: All about skin
Our skin plays multiple roles. For instance, it helps keep our insides inside and blocks the path of pathogens. It also helps us stay warm when it is cold and cool down when it is hot.
Importantly, the skin provides a home for sensory neurons, which let us sense the world around us.
Despite the wide range of physiological functions this organ plays, it is arguably most famous for being the largest organ of the body, although some scientists disagree. The skin is also our most visible organ.
And because it is so visible, skin has also become the target organ for a wide range of products, many of which promise clearer, healthier, more youthful skin.
Because the skin, for many of us, is the poster child of our face, it is no wonder that scientists, doctors, and charlatans have paid it a great deal of attention over the years.
With this heady cocktail of high visibility and multiple physiological roles, it is no wonder that public dermatological perceptions are a mixed bag of myths and misunderstandings.
In this article, we will address 12 common confusions. To help us wrestle fact from fiction, we enlisted the help of three experts:
- Prof. Hywel C. Williams, OBE, D.Sc.: a Fellow of the Academy of Medical Sciences and a National Institute for Health Research Senior Investigator Emeritus. Prof. Williams is also a professor of dermato-epidemiology and co-director of the Center of Evidence-Based Dermatology at Queen’s Medical Centre at Nottingham University Hospitals National Health Service (NHS) Trust.
- Dr. Derrick Phillips: a dermatologist and spokesperson for the British Skin Foundation.
- Dr. Beth G. Goldstein: Founder at Get Mr. and Central Dermatology Center.
1. Expensive skin cream can keep your skin ‘young’ forever
The skin cream industry is huge. For instance, in the United States in 2020, “prestige skin care” sales totaled $1.1 billion from April to June. And that marked an 18% drop from 2019 sales.
However, despite their lucrative popularity and regardless of cost, no skin creams can protect skin against aging indefinitely. “This is a marketing ploy and is certainly not true,” said Dr. Phillips.
As Prof. Williams explained to Medical News Today, “Simple moisturizers can achieve quite a lot. Creams containing topical retinoids can improve photoaging effects.” He dryly notes, however, that he is “not aware of any cream that keeps skin young forever.”
Dr. Goldstein informed us that “90% of skin aging is from photodamage. So all of the creams that state they can prevent wrinkles and aging are missing the mark.”
In agreement, Dr. Phillips wrote: “The most important intervention in slowing down the process is using a sunscreen with broadband UV cover.” Notably, he also notes that “these needn’t be expensive.”
2. Drinking water keeps your skin hydrated
This is a half-truth. According to Prof. Williams, drinking water only keeps your skin hydrated “in the sense that water keeps the body hydrated and skin is the largest organ of the body.”
It is only at certain, rare times when this might be the case. “There is no evidence that drinking water directly impacts your skin unless in extremes, such as heat stroke or severe dehydration,” said Dr. Goldstein.
3. Antibacterial soap is best for the skin
This is a myth. The skin’s natural microbiome is vital for maintaining healthy skin. “Using antibacterial soaps can upset that natural balance,” explained Prof. Williams. “They can also be harsher on the skin than pH neutral soaps.”
“Removing both the good and bad bacteria on a regular basis is not always the best idea,” added Dr. Goldstein, “unless you are in a situation where this is important, for instance, if you work in healthcare, food handling, or of course, during a pandemic.”
4. Having a dirty face causes acne
In Prof. Williams’s professional opinion, this is “nonsense.” Unless, he explained, the dirt “is contamination with oily substances such as hair pomade, oily make-up, or occupational oil exposure.”
Standard dirt will not produce acne.
“Acne is caused by a complex interaction of hormones and the skin, not dirt. People will use scrubs, toners, and many products to clean their faces to address or prevent acne, but often this can just result in irritation. The pores are plugged by keratin, a protein produced by the skin cells, not dirt.”
– Dr. Goldstein
Diving into the details, Dr. Phillips told MNT that, although the skin’s microbiome may differ in people who have acne compared with those who do not, this is not due to cleanliness.
He also adds an interesting note about a rather modern dermatological condition:
“In the past year, there has been a rise in ‘cell phone’ acne, where people get acne spots on the side of their face that presses against their mobile phones. It is thought to be related to a combination of short-wavelength visible light from smartphones, sweat, dust, heat, friction, and bacteria on the surface of the phones. Flares may be prevented by regularly cleaning phone screens.”
5. Chocolate causes acne
Simply put, Prof. Williams writes that this is “another myth.” For the reasons outlined above, this has no basis in fact.
6. All sun exposure is bad for the skin
“All sun exposure causes some degree of photodamage,” explained Prof. Williams, “but some sun exposure is essential for boosting vitamin D synthesis,” especially for people in regions that are further from the equator and those with darker skin who receive lower sun exposure.
Similarly, Dr. Philips told MNT that “The sun is a major source of vitamin D, which is important for bone health and may play a role in the immune system. We also know that UV exposure from the sun has anti-inflammatory properties that can be beneficial in some skin conditions, such as psoriasis, eczema, and pruritus.”
However, he also explained that “these benefits must be counterbalanced against the risk of skin cancer, which we know in white populations is directly related to UV exposure.” He recommends using high-factor sunscreen, wearing appropriate clothing, and staying in the shade between 11 a.m. and 3 p.m. on sunny days.
As someone who focuses on skin cancer surgery, Dr. Goldstein took a firmer line:
“There is a skin cancer epidemic with at least five million new cancers treated each year in the U.S. The majority of these cancers are due to sun exposure.”
Although vitamin D is essential, she explained that we can also derive it from foods and supplements,“1 in 5 Americans will get skin cancer, and melanoma is set to be the most common cancer among men, and only second to breast cancer in women by 2040.”
7. A spray tan protects against UV rays
A spray tan will not protect against sun damage unless it contains added UV protectants. “Just spraying color onto the skin does not protect against UV rays,” said Prof. Williams.
Dr. Phillips reiterates the message: “They do not provide any protection against UV radiation and should not be used as an alternative to sunscreen.”
8. Vitamin E helps get rid of scars
Over the years, many scientists have investigated whether vitamin E reduces the appearance of scars, but our experts were unanimous in their responses. To date, Prof Williams says, the evidence is “unconvincing.”
Dr. Goldstein agreed that “current data do not support the use of vitamin E to help get rid of scars.”
Dr. Phillips goes one step further, writing that “in some instances, it can be detrimental.” However, as an alternative approach, he told us that “silicone gel products have been consistently shown to prevent scar overgrowth and improve the appearance of mature scars.”
9. ’Natural’ products are better for the skin
Products that are marketed as “natural” are popular among consumers. However, the term “natural” says nothing about a product’s effectiveness or safety.
“Arsenic is natural after all,” Prof. Williams reminded us. “Many natural products, such as moisturizers, are very expensive and have no additional benefit over cheaper, refined products.”
He also noted that “natural products can have just as many side effects as well-tested medical products — they may not be as effective, and they may suffer from stability issues. But it is a personal choice — if people like the sound of the word ‘natural’ as a euphemism for ‘gentle’ or ‘safe’ and want to pay for the product, that is up to them.”
“Poison ivy is all-natural,” said Dr. Goldstein, “but you would not rub it all over your skin.” She also explained that all-natural products can still have “serious environmental impacts.” Importantly, according to Dr. Phillips, natural ingredients, especially in high quantities, can trigger allergies and irritate the skin.
10. Wounds need air to heal
This is a long-standing and pervasive myth, but, as Prof. Williams explained succinctly, it is “not true — wounds heal better with a clean, moist environment.”
In agreement, Dr. Goldstein said, “Research has shown that cells migrate better to initiate and continue healing in a moist environment in the early stages of healing in particular. Keeping a wound covered with Aquaphor or similar ointment and a bandage is ideal [if there is no infection].”
She also noted that, toward the end of the healing process, once new connective tissue and microscopic blood vessels have formed, air can aid the healing process.
11. Exfoliating daily is essential for healthy skin
Skin exfoliation is the process of removing dead cells from the surface of the skin. This can be achieved by using an exfoliation tool, a granular surface, or chemicals.
Although popular, exfoliation is not essential. As Prof. Williams explained to MNT, “the skin feels smoother after exfoliating, but repeated exfoliation is damaging the natural skin barrier.”
12. Black salve is a safe treatment for skin cancer
Over recent years, so-called black salve, a derivative of the bloodroot plant, has entered the marketplace. Unscrupulous companies market it as a way to treat skin cancer. In reality, black salve can be dangerous.
Prof. Williams told us that “sanguinarine — the active ingredient in black salve — can cause severe tissue necrosis and may not kill all skin cancer cells. Always see a dermatologist to get suspected skin cancer diagnosed properly first and discuss treatment options if then confirmed.”
He also sent us a link to a recent article discussing black salve. The authors explain that “clinical data concerning the efficacy of bloodroot primarily come from case studies with unfavorable outcomes involving patients who self-treated with bloodroot-containing black salves.”
Dr. Goldstein mirrors these findings, explaining that “I have seen sad outcomes of people trying this treatment.” She also reiterated that black salve damages healthy tissue without effectively curing cancer.
Dr. Phillips confirms the negative consequences of black salve: “The Food and Drug Administration (FDA) has listed black salve as a fake cancer cure, and it should be avoided!”
How can we prevent the spread of SARS-CoV-2 in children?
Children are being hospitalized with COVID-19 in record numbers across the United States. As most children are not old enough to get vaccinated, hospitalizations could further increase as schools reopen. Doctors and epidemiologists are thus calling for the use of safety precautions, such as masks and ventilation, during class.
The rise in cases of COVID-19 among children in the U.S. is primarily linked to the Delta variant. Cases are rising especially quickly in communities with low rates of COVID-19 vaccinations.
Although the Centers for Disease Control and Prevention (CDC) recommend universal indoor masking and physical distancing in schools, mask-wearing is optional in North Dakota and Ohio.
Rapidly increasing infection rates among children and teachers have forced many schools in the U.S. to halt in-person learning and turn to hybrid models of education. This comes despite 175 pediatric disease experts agreeing earlier this year that elementary schools could open full-time for in-person instruction.
Although children generally have milder COVID-19 symptoms than adults, the fact that few studies have investigated how the disease affects children means that many questions remain unanswered. For example, why are so many children being hospitalized with COVID-19? Which children are most at risk? And what can parents and authorities do so that children can return to school safely?
To answer these questions and more, we spoke with seven doctors and researchers who specialize in pediatrics and infectious diseases and have worked directly with children with COVID-19.
Why are COVID-19 hospitalizations among children increasing?
The Delta variant of COVID-19 is more than two times as contagious as previous variants. Alongside school reopenings, this may partially explain the increase in pediatric hospitalizations due to COVID-19.
The Delta variant that is circulating widely is more contagious, and children are getting infected more often than previously during the pandemic.
Now, you have a more contagious variant with fewer mitigation measures in place. With the rising number of cases, unfortunately, you will see more hospitalizations. As an example, if 2% of children need hospitalization, then it’s a big difference between 2% of 10,000 cases vs. 2% of 100,000 cases.
Another reason for rising COVID-19 hospitalizations among children may be that those under the age of 12 years cannot get the vaccination yet.
Vaccines remain effective at preventing severe illness, hospitalization, and death from [SARS-CoV-2] infection, even Delta strain infection,” Kristin Moffitt, M.D., an infectious disease expert at Boston Children’s Hospital, MA. “This is consistent with reports that the overwhelming majority of hospitalizations and deaths during the recent surge are occurring in unvaccinated individuals.
“Since children under 12 aren’t yet able to be vaccinated, and many adolescents and young adults remain unvaccinated relative to older individuals, this age group is making up a bigger proportion of those at risk for severe illness based on their unvaccinated status,” she added.
Dr. Karen Ravin, M.D., chief of infectious diseases at Nemours Children’s Hospital in Delaware, agreed. “Children under 12 years of age make up a substantial proportion of the unvaccinated population in the U.S., so they are the population at highest risk,” she said. “Early in the pandemic, schools were closed, and children had a lower risk of exposure in the community. Contrast this to now, schools are open for in-person instruction so children are at greater risk for being exposed, becoming infected, and, unfortunately, being hospitalized.”
“Overall, children are at lower risk for severe illness, hospitalization, and death due to COVID-19, but they are not at no risk.”
– Dr. Karen Ravin
“Early in the pandemic, those over 65 accounted for more severe disease and hospitalization. Now that this age group has a higher percentage of vaccinated persons, the disease burden will be seen in the younger, unvaccinated population,” noted Dr. Adriana Cadilla, an infectious diseases pediatric specialist at Nemours Children’s Hospital in Orlando, FL. “[In Florida,] there has been over a four-fold increase in child [SARS-CoV-2] infections in the past month,” Dr. Cadilla added.
Is the Delta variant more severe than earlier strains?
Although the number of COVID-19 cases among children is increasing more quickly now than at any other time in the pandemic, it is unclear whether the Delta variant of SARS-CoV-2 is more severe for children than previous variants.
“We don’t know if the Delta variant causes more severe disease for kids than previous variants, but it’s definitely more contagious,” said Dr. Chang.
Due to low testing and hospital admissions among children from previous variants, the data to compare the outcome of COVID-19 strains are sparse. As schools reopen, however, and safety precautions such as mask-wearing wane, more children are becoming infected with SARS-CoV-2 at the same time, leading to higher numbers of children developing severe COVID-19.
There are some indications to suggest that COVID-19 from the Delta variant is more severe in children than with earlier strains,” Dr. Allison Ross Eckard, M.D., professor of pediatrics and medicine at the Medical University of South Carolina.
“We are seeing a greater number of children, particularly unvaccinated adolescents, with more severe COVID-19 resulting in respiratory failure that is requiring intubation and sometimes ECMO (heart-lung bypass machine), ARDS (a very serious lung condition that develops as a result of the inflammation associated with COVID-19), and other COVID-related problems — all complications we more commonly see in adults,” she continued.
“It may be that the increased number of hospitalizations among children is a result of both of these factors — more cases combined with a higher chance of severe disease. More data is needed to determine the exact reason(s) behind what we are seeing,” she added.
Which children are at higher risk of adverse outcomes from COVID-19?
The CDC says that children with underlying medical conditions, such as congenital heart disease or genetic, neurologic, or metabolic conditions, could have an increased risk of severe outcomes from COVID-19.
The CDC states that this higher risk also applies to children with obesity, diabetes, asthma, chronic lung disease, sickle cell disease, or immunosuppression.
“Children who are at higher risk of adverse outcomes from COVID-19 are those under 1 year of age, those with underlying conditions, and those with immunocompromising conditions, including those on immunocompromising medications,” Dr. Tina Q. Tan, M.D., medical director at Ann & Robert H. Lurie Children’s Hospital of Chicago.
“Other children may also develop more severe disease, resulting in the need for hospitalization, but at a lower rate than those with underlying or immunocompromising conditions,” she added.
“Anecdotally, most of our hospitalized patients with COVID-19 are unvaccinated teenagers. Many of these teens are quite ill, and their only risk factors are obesity and/or asthma,” Dr. Danielle Zerr, M.D., M.P.H., professor and division chief of pediatric infectious disease and adjunct professor of epidemiology, University of Washington.
Dr. Chang echoed these statements, saying that teenagers with a body mass index of 25 or above and infants under the age of 1 year have a higher risk of hospitalization.
“Many families think their children are healthy and, therefore, not at risk of severe COVID-19,” said Dr. Eckard. “While that is true statistically, we cannot always predict which children will develop severe disease, and children [without underlying conditions] sometimes do develop severe disease.”
“In addition, some children are healthy but perhaps require an inhaler a couple of times per year, or some children’s families don’t even realize they are overweight. So, there is sometimes a misconception about a child’s risk. Therefore, it is very important for every family to discuss their child’s health with their primary care physicians to ensure that all children are appropriately protected.”
– Dr. Allison Eckard
“We are still learning what causes some children to develop more severe COVID-19 than others, but it is important to know that perfectly healthy children can develop severe COVID-19,” Elizabeth Mack, M.D., M.S., medical director of pediatric critical care medicine at the Medical University of South Carolina, told MNT.
Dr. Mack also noted that the risk of death from severe COVID-19 remains a possibility even for children without underlying conditions.
Race, ethnicity, and socioeconomic conditions may also play a role in adverse outcomes from COVID-19 among children. Dr. Cadilla noted, “Hospitalization rates are higher among Hispanic [and] Latino children and non-Hispanic Black children, mirroring adult data.”
While more data are necessary to confirm why this is the case among children, among adults, research highlights deep-seated inequities that put these populations at higher risk.
For example, Hispanic, Latinx, and non-Hispanic Black populations are more likely to be uninsured, working in jobs that do not offer remote working, and living in conditions that make it difficult to practice physical distancing and self-isolation. These populations also have higher rates of underlying health conditions, such as diabetes and obesity.
For live updates on the latest developments regarding the novel coronavirus and COVID-19, click here.
All data and statistics are based on publicly available data at the time of publication. Some information may be out of date. Visit our coronavirus hub and follow our live updates page for the most recent information on the COVID-19 pandemic.
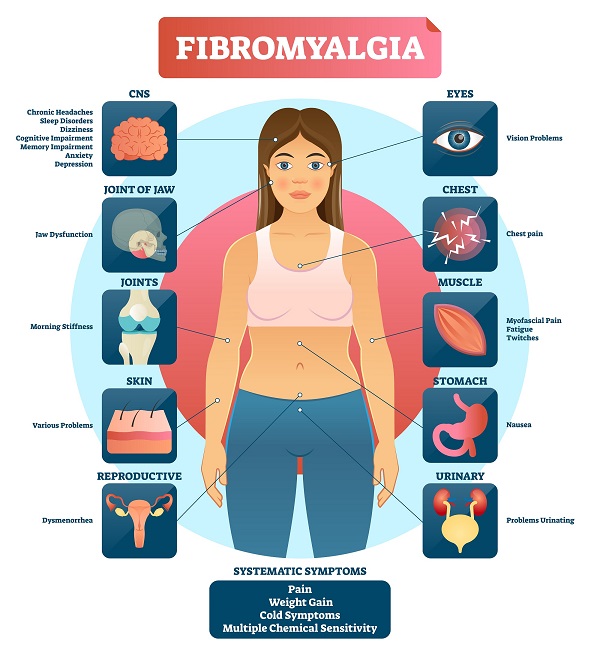
Everything you need to know about fibromyalgia
Fibromyalgia is a common and chronic syndrome that causes bodily pain and mental distress.
Symptoms of fibromyalgia can be confused with those of arthritis, or joint inflammation. However, unlike arthritis, it has not been found to cause joint or muscle inflammation and damage. It is seen as a rheumatic condition, in other words, one that causes soft tissue pain or myofascial pain.
According to the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), around 5 million adults aged 18 years or over in the United States experience fibromyalgia, and 80 to 90 percent of fibromyalgia patients are women.
Symptoms
Common symptoms include:
- widespread pain
- jaw pain and stiffness
- pain and tiredness in the face muscles and adjacent fibrous tissues
- stiff joints and muscles in the morning
- headaches
- irregular sleep patterns
- irritable bowel syndrome (IBS)
- painful menstrual periods
- tingling and numbness in the hands and feet
- restless leg syndrome (RLS)
- sensitivity to cold or heat
- difficulties with memory and concentration, known as “fibro-fog”
- fatigue
The following are also possible:
- problems with vision
- nausea
- pelvic and urinary problems
- weight gain
- dizziness
- cold or flu-like symptoms
- skin problems
- chest symptoms
- depression and anxiety
- breathing problems
Symptoms can appear at any time during a person’s life, but they are most commonly reported around the age of 45 years.
Treatment
Around 20 percent of people with fibromyalgia try acupuncture within the first 2 years. It may work, but more research is needed.
Medical attention is needed because fibromyalgia can be difficult to manage. As it is a syndrome, each patient will experience a different set of symptoms, and an individual treatment plan will be necessary.
Treatment may include some or all of the following:
- an active exercise program
- acupuncture
- psychotherapy
- behavior modification therapy
- chiropractic care
- massage
- physical therapy
- low-dose anti-depressants, although these are not a first-line treatment
People with fibromyalgia need to work with their doctor to come up with a treatment plan that provides the best results.
Drugs
Drugs may be recommended to treat certain symptoms.
These may include over-the-counter (OTC) pain relievers. However, the European League Against Rheumatism (EULAR) issued a recommendation against using non-steroidal anti-inflammatory drugs (NSAIDs) to treat fibromyalgia in their updated 2016 guidelines.
Antidepressants, such as duloxetine, or Cymbalta, and milnacipran, or Savella, may help reduce pain. Anti-seizure drugs, such as gabapentin also known as Neurontin, and pregabalin, or Lyrica, may be prescribed.
However, a review has suggested that patients often stop using these drugs because they are not effective in relieving pain or because of their adverse effects.
Patients should tell the doctor about any other medications they are taking to avoid side-effects and interactions with other drugs.
Exercise
A combination of aerobic exercise and resistance training, or strength training, has been linked to a reduction in pain, tenderness, stiffness, and sleep disturbance, in some patients.
If exercise is helping with symptoms, it is important to maintain consistency in order to see progress. Working out with a partner or personal trainer may help to keep the exercise program active.
Acupuncture
Some patients have experienced improvements in their quality of life after starting acupuncture therapy for fibromyalgia. The number of sessions required will depend on the symptoms and their severity.
One study found that 1 in 5 people with fibromyalgia use acupuncture within 2 years of diagnosis. The researchers concluded that it may improve pain and stiffness. However, they call for more studies.
Behavior modification therapy
Behavior modification therapy is a form of cognitive behavioral therapy (CBT) that aims to reduce negative, stress- or pain-increasing behaviors and improve positive, mindful behaviors. It includes learning new coping skills and relaxation exercises.
Causes
The exact cause of fibromyalgia is unclear. However, current thinking in the field of Rheumatology suggests that fibromyalgia is a problem with central pain processing in the brain, where there may be an increased sensitivity or perception of pain to a given trigger.
There is a range of likely risk factors, including:
- a stressful, traumatic physical or emotional event, such as a car accident
- repetitive injuries
- rheumatoid arthritis or other autoimmune diseases, such as lupus
- central nervous system (CNS) problems
- the way our genes regulate how we process painful stimuli
Fibromyalgia may also be hereditary. Females who have a close relative with fibromyalgia have a higher risk of experiencing it themselves.
People with rheumatoid arthritis, lupus, or spinal arthritis, known ankylosing spondylitis, have a higher risk of developing fibromyalgia, as do patients with some other rheumatic diseases.
Diagnosis
It can take some time to confirm a diagnosis of fibromyalgia because the symptoms resemble those of other conditions, such as hypothyroidism. These conditions must first be ruled out before diagnosing fibromyalgia.
There are no laboratory tests for the condition, and this, too, can lead to delayed or missed diagnosis.
The American College of Rheumatology has established three criteria for diagnosing fibromyalgia.
- pain and symptoms over the previous week, out of 19 identified body parts, plus levels of fatigue, unsatisfactory sleep, or cognitive problems
- symptoms that have been ongoing for at least 3 months
- no presence of another health problem that would explain the symptoms
Previously, ‘tender points’ were used to diagnose the condition. However, these are no longer recommended to aid the diagnosis of fibromyalgia.
Diet
Dietary measures have been suggested for improving the symptoms of fibromyalgia.
These include:
- High-energy foods that are low in sugar: Foods such as almonds, beans, oatmeal, avocado, and tofu contain plenty of fiber but no added sugar. These can help boost energy throughout the day, helping to improve tiredness symptoms that occur as a result of the condition.
- Avoiding foods that have gluten: A 2014 study has suggested that gluten sensitivity can contribute to fibromyalgia. The study showed that removing foods that contain gluten from the diet may be able to reduce the pain, even in patients who do not have celiac disease. This is also linked to a diet plan for reducing inflammation.
- Cutting out fermentable oligo-di-mono-saccharides and polyols (FODMAP): A recent study showed that a diet low in FODMAP could have promising effects on pain levels in people with fibromyalgia.
- Not eating additives and excitotoxins: One report showed that cutting out additives from the diet, such as aspartame and monosodium glutamate (MSG), can reduce pain symptoms significantly. The pain of the people involved in the study was also shown to increase once these additives were put back in the diet.
- Eating more seeds and nuts: There is little evidence to support a direct relationship between seeds, nuts, and an improvement in fibromyalgia symptoms. However, they are known to contain powerful micronutrients and minerals that are important for cell function, and this may support people with the condition.
Maintaining a balanced diet and healthy weight is vital to ongoing health and can improve a person’s quality of life. Studies have shown that people with both fibromyalgia and obesity showed an improvement in quality of life and pain symptoms once they lost weight.
More research is needed on the effects of diet on fibromyalgia, but making sure the diet is low in sugar and gluten is a good starting point. There is certainly no harm is trying these options to support treatment.
Tender points
When reading up on fibromyalgia, you may have come across the term ‘tender points.’
These are certain areas of the body in which fibromyalgia is said to cause the most pain. These include the back of the head, inner knees, and outer elbows. Pain can also be increased in the neck and shoulders, the outer hips, and the upper chest.
Doctors used to diagnose fibromyalgia based on how they react to pressure at these points. However, this is no longer seen as an accurate way to diagnose the condition, and tender points are no longer used as a reliable indicator of fibromyalgia.
Injections are not advised at these points. However, the pain is now thought to be more widespread and present differently in different people. Instead of specific areas or points of pain, fibromyalgia is identified by the severity and chronic nature of the pain.
Seek medical attention to rule out other causes of pain in these areas.
Outlook
There is no definitive cure for fibromyalgia, but more treatment options and clearer diagnostic criteria are now available.
Symptoms can improve significantly, as long as the patient follows their treatment plan.
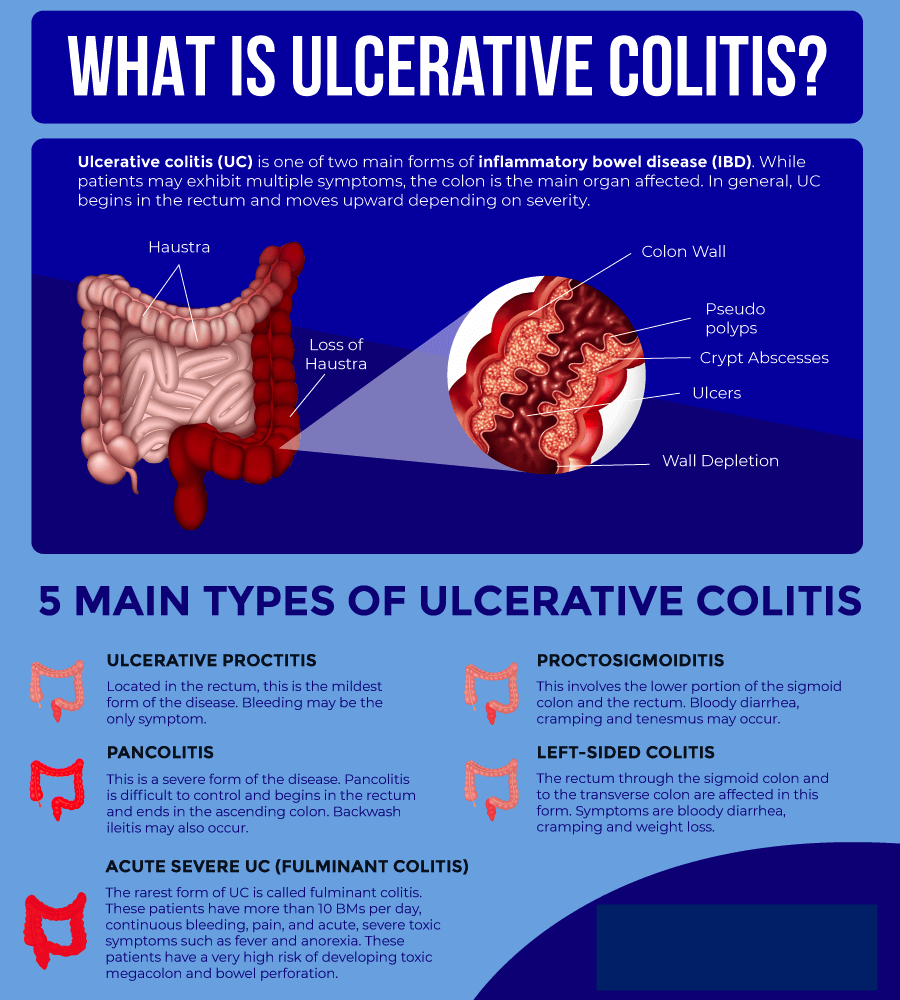
Ulcerative colitis is a relatively common long-term condition that causes inflammation in the colon. It is a form of inflammatory bowel disease (IBD) that is similar to Crohn’s disease.
The colon removes nutrients from undigested food and eliminates waste products through the rectum and anus as feces.
In severe cases, ulcers form on the lining of the colon. These ulcers may bleed, which produces pus and mucus.
Various medication options are available, and doctors can tailor treatment to meet individual needs.
Symptoms
The first symptom of ulcerative colitis is usually diarrhea.
Stools become progressively looser, and some people may experience abdominal pain with cramps and a severe urge to go to the bathroom.
Diarrhea may begin slowly or suddenly. Symptoms depend on the extent and spread of inflammation.
The most common symptoms of ulcerative colitis include:
- abdominal pain
- bloody diarrhea with mucus
Some people may also experience:
- fatigue or tiredness
- weight loss
- loss of appetite
- anemia
- elevated temperature
- dehydration
- a constant urge to pass stools
Symptoms are often worse early in the morning.
Symptoms may be mild or absent for months or years at a time. However, they will usually return without treatment and vary depending on the affected part of the colon.
What causes red diarrhea?
Types
Symptoms may vary depending on the area of inflammation.
The sections below discuss the various types of ulcerative colitis, many of which affect different parts of the colon:
Ulcerative proctitis
This type affects only the end of the colon, or the rectum. Symptoms tend to include:
- rectal bleeding, which may be the only symptom
- rectal pain
- an inability to pass stools despite frequent urges
Ulcerative proctitis is usually the mildest type of ulcerative colitis.
Proctosigmoiditis
This involves the rectum and the sigmoid colon, which is the lower end of the colon.
Symptoms include:
- bloody diarrhea
- abdominal cramps
- abdominal pain
- a constant urge to pass stool
Left-sided colitis
This affects the rectum and the left side of the sigmoid and descending colon.
Symptoms usually include:
- bloody diarrhea
- abdominal cramping on the left side
- weight loss
Pancolitis
This affects the whole colon. Symptoms include:
- occasionally severe, bloody diarrhea
- abdominal pain and cramps
- fatigue
- considerable weight loss
Fulminant colitis
This is a rare, potentially life threatening form of colitis that affects the whole colon.
Symptoms tend to include severe pain and diarrhea, which can lead to dehydration and shock.
Fulminant colitis can present a risk of colon rupture and toxic megacolon, which causes the colon to become severely distended.
Diet
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), some dietary measures may help relieve symptoms, including:
- eating smaller, more regular meals, such as five or six small meals per day
- drinking plenty of fluids, especially water, to prevent dehydration
- avoiding caffeine and alcohol, which can both increase diarrhea
- avoiding sodas, which can increase gas
- keeping a food diary to identify which foods make symptoms worse
A doctor may suggest temporarily following a specific diet depending on symptoms, such as:
- a low fiber diet
- a lactose-free diet
- a low fat diet
- a low salt diet
It may help to take supplements or eliminate particular foods from the diet. However, a person should discuss any complementary or alternative measures with a doctor before trying them.
Here, find out more about what to eat and avoid with ulcerative colitis.
Causes
The exact causes of ulcerative colitis are unclear. However, they may involve the following:
Genetic factors
ResearchTrusted Source suggests that people with ulcerative colitis are more likely to have certain genetic features. The specific genetic feature that a person has may affect the age at which the disease appears.
Environment
The following environmental factors might affect the onset of ulcerative colitis:
- diet
- air pollution
- cigarette smoke
Immune system
The body might respond to a viral or bacterial infection in a way that causes the inflammation associated with ulcerative colitis.
Once the infection resolves, the immune system continues to respond, which leads to ongoing inflammation.
Another theory suggests that ulcerative colitis may be an autoimmune condition. A fault in the immune system may cause it to fight nonexistent infections, leading to inflammation in the colon.
Risk factors
Some known risk factors for ulcerative colitis include:
- Age: Ulcerative colitis can affect people at any age but is more common at 15–30 years of age.
- Ethnicity: White people and those of Ashkenazi Jewish descent have a higher risk of developing the condition.
- Genetics: Although recent studies have identified specific genes that may play a role in ulcerative colitis, the link is unclear due to the role of environmental factors.
Diagnosis
A doctor will ask about a person’s symptoms and medical history. They will also ask whether any close relatives have had ulcerative colitis, IBD, or Crohn’s disease.
They will also check for signs of anemia, or low iron levels in the blood, and tenderness around the abdomen.
Several tests can help rule out other possible conditions and diseases, including Crohn’s disease, infection, and irritable bowel syndrome.
These include:
- blood tests
- stool tests
- X-ray
- barium enema, during which a healthcare professional passes a fluid called barium through the colon to show any changes or anomalies in a scan
- sigmoidoscopy, in which a healthcare professional inserts a flexible tube with a camera at the end, called an endoscope, into the rectum
- colonoscopy, wherein a doctor examines the whole colon using an endoscope
- a CT scan of the abdomen or pelvis
A person with ulcerative colitis will need to see a doctor who specializes in treating conditions of the digestive system, or a gastroenterologist.
They will assess the type and severity of the condition and create a treatment plan.
Treatment
Ulcerative colitis symptoms can range from mild to severe, but it needs treatment. Without treatment, the symptoms may go away, but there is a higher chance of them coming back.
Most people will receive outpatient treatment. However, around 15% of people with the disease have a severe form. Of these, 1 in 5 may need to spend time in the hospital.
Treatment will focus on:
- maintaining remission to prevent further symptoms
- managing a flare until symptoms go into remission
Various medications are available, and a doctor will make a treatment plan that takes individual needs and wishes into account. Natural approaches can support medical treatment, but they cannot replace it.
Long-term treatment to maintain remission
The first aim of treatment is to reduce the risk of a flare and its severity if a flare does occur. Long-term therapy can help achieve this.
There are several types of medication, and a doctor will make a treatment plan to suit the individual.
Ulcerative colitis results from a problem with the immune system. Three types of drugs that can help are biologics, immunomodulators, and small molecules. These target the way the immune system works.
They include:
- TNF-α antagonists, such as infliximab (Remicade) or adalimumab (Humira)
- anti-integrin agents, such as vedolizumab (Entyvio)
- Janus kinase inhibitors, such as tofacitinib (Xeljanz)
- interleukin 12/23 antagonists, such as ustekinumab (Stelara)
- immunomodulators, for instance, thiopurines (azathioprines) and methotrexate
These drugs can help people with moderate to severe symptoms, but they may have adverse effects. People should talk to their doctor about the options available and the benefits and risks of each drug.
However, for mild to moderate symptoms, guidelines suggest 5-aminosalicylic acid, or aminosalicylates (5-ASA), as a first-line treatment.
Examples include:
- mesalamine
- balsalazide
- sulfasalazine
Other options
Aminosalicylates: In the past, 5-ASA played a key role in treating the symptoms of ulcerative colitis. These are still an option, but current guidelines recommend focusing on long-term treatment to prevent symptoms from occurring in the first place.
Steroids: These can help manage inflammation if aminosalicylates do not help. However, long-term use can have adverse effects, and experts recommend minimizing their use.
Managing severe active ulcerative colitis
A person with severe symptoms may need to spend time in the hospital. Hospital treatment can reduce the risk of malnutrition, dehydration, and life threatening complications, such as colon rupture. Treatment will include intravenous fluids and medications.
Surgery
If other treatments do not provide relief, surgery may be an option.
Some surgical options include:
- Colectomy: A surgeon removes part or all of the colon.
- Ileostomy: A surgeon makes an incision in the stomach, extracts the end of the small intestine, and connects it to an external pouch, called a Kock pouch. The pouch then collects waste material from the intestine.
- Ileoanal pouch: A surgeon constructs a pouch from the small intestine and connects it to the muscles surrounding the anus. The ileoanal pouch is not an external pouch. Sometimes it is called a J-pouch.
According to the American Gastroenterological Association, around 10–15% of people with ulcerative colitis will need a colectomy.
Lifestyle and natural remedies
Some home care strategies and remedies may help manage the symptoms of ulcerative colitis.
Natural medicine
Here are some options that people may use:
- Probiotics: A 2019 review suggests that some probiotics may help manage IBD.
- Herbal remedies: Other researchTrusted Source from 2019 found that some herbal remedies may help reduce symptoms and manage the condition. Examples include aloe vera gel and wheatgrass juice.
- Fruits and other plant-based foods: Some earlier research shows that ingredients naturally present in blueberries, black raspberries, cocoa, Indian quince, green tea, grapes, olive oil, and Indian gooseberries may have a beneficial effect.
- Spices: Garlic, ginger, fenugreek, saffron, turmeric, and Malabar tamarind may help with IBD symptoms.
Research has not yet confirmed the possible benefits of the options above, but moderate amounts appear safe to add to the diet. However, it is worth checking with a healthcare professional first.
Lifestyle options
Scientists have also found that the following may help:
Education: The more a person knows about a health condition, the more in control they tend to feel. Learning about ulcerative colitis can help ease anxiety and lead to effective coping and management techniques, research from 2017Trusted Source shows.
Exercise: Some research suggests that aerobic exercise may have an anti-inflammatory effect, which could benefit people with ulcerative colitis. One 2019 studyTrusted Source, for example, found that combining exercise with an anti-inflammatory diet could have a positive effect. Check with a healthcare professional before changing an exercise routine, however, as 20% of participants with ulcerative colitis in a 2016 study experienced a worsening of symptoms after doing intense exercise.
Mindfulness: In a 2020 study, 37 people with ulcerative colitis engaged in a mindfulness-based intervention that involved four online therapy and four face-to-face sessions. After 6 months, the participants had lower markers of inflammation than 20 participants who did not have the sessions.
Complications
The possible complications of ulcerative colitis can range from a lack of nutrients to potentially fatal bleeding from the rectum.
Possible complications include:
Colorectal cancer
Ulcerative colitis, especially if symptoms are severe or extensive, increases the risk of developing colon cancer.
According to the NIDDK, colon cancer risk is highest when ulcerative colitis affects the entire colon for longer than 8 years.
Toxic megacolon
This complication occurs in a few cases of severe ulcerative colitis.
In toxic megacolon, gas becomes trapped, causing the colon to swell. When this occurs, there is a risk of colon rupture, septicemia, and shock.
Other complications
Other possible complications of ulcerative colitis include:
- inflammation of the skin, joints, and eyes
- liver disease
- osteoporosis
- perforated colon
- severe bleeding
- severe dehydration
To prevent bone density loss, a doctor may prescribe vitamin D supplements, calcium, or other medications.
Attending regular medical appointments, closely following a doctor’s advice, and being aware of symptoms can help prevent these complications.
Obesity
Obesity is a major risk factor for various metabolic disorders and cardiovascular diseases.
According to the World Health Organization (WHO), today, most of the world’s population lives in countries where obesity kills more people than malnutrition.
The prevalence of obesity has significantly increased in adults in the past few decades. As such, researchers are engaged in finding new ways to understand and potentially treat obesity.
A new study, which appears in the open-access journal PLOS Biology found that high levels of a cytokine — interleukin-25 — promotes the production of beige fat cells.
The study’s results might help find new ways to treat obesity and other metabolic disorders.
Significance of beige fat in humans
Not all fat stored in the body is harmful to health. Typically, there are two types of fat tissue: brown and white.
Brown fat helps turn food into heat, whereas white fat is responsible for storing calories; thus, an excess of white fat contributes to obesity.
However, scientists have discovered another type of fat cell in human adults, known as beige fat. Typically, these cells burn energy in a similar way to brown fat rather than storing it like white fat.
How do beige cells burn energy?
Beige fat cells, or adipocytes, are present in white adipose tissue. They can perform functions similar to both white and brown adipocytes. Generally, they act like white cells by storing energy.
However, when exposed to cold temperatures, they behave like brown cells and dissipate energy by creating heat.
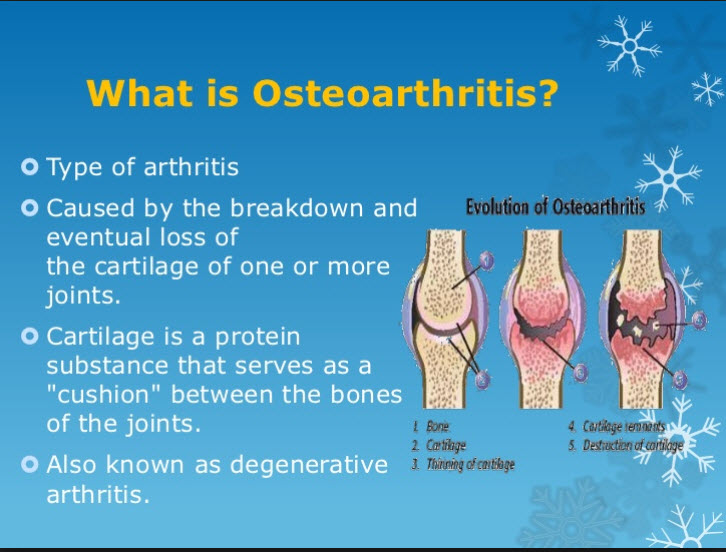
Everything you need to know about osteoarthritis
Osteoarthritis (OA) causes inflammation in the joints and the breakdown and gradual loss of joint cartilage. As the cartilage wears down, a person experiences pain and difficulty with movement.
OA is a common joint disorder. It develops in the hand, for example, in 1 in 12 people over the age of 60, according to the Arthritis Foundation.
OA is a progressive disease, which means that symptoms worsen over time.
There is no cure, but treatment can help manage pain and swelling and keep a person mobile and active.
Symptoms
OA leads to pain and stiffness in the joints.
In the early stages, a person may have no symptoms. Symptoms may occur in one or more joints, and they tend to appear gradually.
When symptoms develop, they can include:
- pain and stiffness that worsen after not moving the joint for a while
- swelling
- difficulty moving the affected joint
- warmth and tenderness in the joints
- a loss of muscle bulk
- a grating or crackling sound in the joint, known as crepitus
The progression of OA involves:
- synovitis — mild inflammation of the tissues around the joints
- damage and loss of cartilage
- bony growths that form around the edges of joints
Effects
Cartilage is a protective substance that cushions the ends of the bones in the joints and allows the joints to move smoothly and easily.
In people with OA, the smooth surface of the cartilage becomes rough and starts to wear away. As a result, the unprotected bones start to rub together, causing damage and pain.
Eventually, bony lumps form on the joint. The medical names for these are bone spurs or osteophytes, and they can lend a knobbly appearance to the joint.
As the bones change shape, the joints become stiffer, less mobile, and painful. Fluid may also accumulate in the joint, resulting in swelling. While OA can develop in any joint, it commonly affects the knees, hips, hands, lower back, and neck.
The knees
OA usually occurs in both knees, unless it results from an injury or another condition.
A person with the condition may notice that:
- There is pain when walking, especially uphill or upstairs.
- The knees lock into position, making it harder to straighten the leg.
- There is a soft, grating sound when they bend or flex the knee.
The hips
A person with OA in the hips may find that any movement of the hip joint, such as standing up or sitting down, can cause difficulty or discomfort.
Pain in the hips is a common feature of the condition. OA in the hips can also cause pain in the knee or in the thighs and buttocks.
A person may experience this pain while resting as well as while walking, for example.
The hands
In the hands, OA can develop in:
- the base of the thumb
- the top joint of the other fingers, closest to the nail
- the middle joint of the other fingers
A person with the condition may notice:
- pain, stiffness, and swelling in the fingers
- bumps that develop on the finger joints
- a slight bend sideways at the affected joints
- fluid-filled lumps or cysts on the backs of the fingers, which may be painful
- a bump that develops where the thumb joins the wrist, which can make it difficult to write or turn a key
For some people, the finger pain decreases and eventually goes away, though the swelling and bumps remain.
Anyone who experiences joint stiffness and swelling for more than 2 weeks should see a doctor.
Causes
Doctors do not know the exact cause of OA, but it seems to develop when the body is unable to repair joint tissue in the usual way.
It often affects older people, but it can occur at any age.
Genetic factors
Some genetic features increase the risk of developing OA. When these features are present, the condition can occur in people as young as 20 years old.
Trauma and overuse
A traumatic injury, surgery, or overuse of a joint can undermine the body’s ability to carry out routine repairs and may trigger OA, eventually leading to symptoms.
It can take several years for OA symptoms to appear after an injury.
Reasons for overuse or repeated injury include jobs and sports that involve repetitive movement.
Risk factors
A number of risk factors increase the chances of developing OA.
- Sex: OA is more common among females than males, especially after the age of 50.
- Age: Symptoms are more likely to appear after the age of 40, though OA can develop in younger people after an injury — especially to the knee — or as a result of another joint condition.
- Obesity: Excess weight can put strain on weight-bearing joints, increasing the risk of damage.
- Occupation: Jobs that involve repetitive movements in a particular joint increase the risk.
- Genetic and hereditary factors: These can increase the risk in some people.
Other conditions
Some diseases and conditions make it more likely that a person will develop OA.
- inflammatory arthritis, such as gout or rheumatoid arthritis
- Paget’s disease of the bone
- septic arthritis
- poor alignment of the knee, hip, and ankle
- having legs of different lengths
- some joint and cartilage abnormalities that are present from birth
Diagnosis
A doctor will ask about symptoms and perform a physical examination.
No definitive test can diagnose OA, but tests can show whether damage has occurred and help rule out other causes.
Tests may include:
X-rays and MRI: These can reveal bone spurs around a joint or a narrowing within a joint, suggesting that cartilage is breaking down.
Joint fluid analysis: A doctor will use a sterile needle to withdraw fluid from an inflamed joint for analysis. This can rule out gout or an infection.
Blood tests: These can help rule out other conditions, such as rheumatoid arthritis.
Treatment
While no treatment can reverse the damage of OA, some can help relieve symptoms and maintain mobility in the affected joints.
Interventions include exercise, manual therapy, lifestyle modification, and medication.
Medication
Medication can help reduce pain.
Acetaminophen (Tylenol)
This can relieve pain in people with mild to moderate symptoms. Follow the doctor’s instructions, as overuse can lead to side effects and cause interactions with other medications.
Nonsteroidal anti-inflammatory drugs
If acetaminophen does not help, the doctor may recommend a stronger pain reliever, which may include ibuprofen, aspirin, or diclofenac.
A person can take these orally or topically, applying the medication directly to the skin.
Capsaicin cream
This is a topical medication that contains the active compound in chilies. It creates a sensation of heat that can reduce levels of substance P, a chemical that acts as a pain messenger.
Pain relief can take 2 weeks to a month to fully take effect.
Do not use the cream on broken or inflamed skin, and avoid touching the eyes, face, and genitals after using it.
Intra-articular cortisone injections
Corticosteroid injections in the joint can help manage severe pain, swelling, and inflammation. These are effective, but frequent use can lead to adverse effects, including joint damage and a higher risk of osteoporosis.
Duloxetine (Cymbalta) is an oral drug that can help treat chronic musculoskeletal pain.
Physical therapy
Various types of physical therapy may help, including:
Transcutaneous electrical nerve stimulation (TENS): A TENS unit attaches to the skin with electrodes. Electrical currents then pass from the unit through the skin and overwhelm the nervous system, reducing its ability to transmit pain signals.
Thermotherapy: Heat and cold may help reduce pain and stiffness in the joints. A person could try wrapping a hot water bottle or an ice pack in a towel and placing it on the affected joint.
Manual therapy: This involves a physical therapist using hands-on techniques to help keep the joints flexible and supple.
Assistive devices
Various tools can provide physical support for a person with OA.
Special footwear or insoles can help, if OA affects the knees, hips, or feet, by distributing body weight more evenly. Some shock-absorbing insoles can also reduce the pressure on the joints.
A stick or cane can help take the weight off of the affected joints and may reduce the risk of a fall. A person should use it on side of the body opposite to the areas with OA.
Splints, leg braces, and supportive dressings can help with resting a painful joint. A splint is a piece of rigid material that provides joint or bone support.
Do not use a splint all the time, however, as the muscles can weaken without use.
Surgery
Some people may need surgery if OA severely affects the hips, knees, joints, or the base of the thumbs.
A doctor will usually only recommend surgery if other therapies have not helped or if there is severe damage in a joint.
Some helpful procedures include:
Arthroplasty
This involves a surgeon removing the damaged areas and inserting an artificial joint, made of metal and plastic. Some refer to this procedure as a total joint replacement.
The joints that most often require replacing are the hip and knee joints, but implants can also replace the joints in the shoulder, finger, ankle, and elbow.
Most people can use their new joint actively and painlessly. However, there is a small risk of infection and bleeding. An artificial joint may also come loose or wear down and eventually need replacing.
Arthrodesis
This involves a surgeon realigning, stabilizing, or surgically fixing the joint to encourage the bones to fuse. Increased stability can reduce pain.
A person with a fused ankle joint will be able to put their weight on it painlessly, but they will not be able to flex it.
Osteotomy
This involves a surgeon removing a small section of bone, either above or below the knee joint. It can realign the leg so that the person’s weight no longer bears down as heavily on the damaged part of the joint.
This can help relieve symptoms, but the person may need knee replacement surgery later on.
Complications
Septic arthritis is joint inflammation caused by bacteria. Joint replacement surgery slightly increases the risk of this infection.
This is a medical emergency, and hospitalization is necessary. Treatment involves antibiotic medication and drainage of the infected fluid from the joint.
Lifestyle tips
A range of strategies can help ease the symptoms of OA. Ask the doctor for advice about suitable lifestyle adjustments. They may recommend:
Exercise and weight control
Exercise is crucial for:
- maintaining mobility and range of movement
- improving strength and muscle tone
- preventing weight gain
- building up muscles
- reducing stress
- lowering the risk of other conditions, such as cardiovascular disease
Current guidelines recommend that everyone should do at least 150 minutes of moderate-intensity exercise each week.
A doctor or physical therapist can help develop an exercise program, and it is important to follow their instructions carefully to prevent further damage.
Choose activities that will not put additional strain on the joints. Swimming and other types of water-based exercise are a good way to keep fit without putting additional pressure on the joints.
Assistive devices and adjustments
A loss of mobility due to OA can lead to further problems, such as:
- an increased risk of falls
- difficulty carrying out daily tasks
- stress
- isolation and depression
- difficulty working
A physical or occupational therapist can help with these issues. They may recommend:
Assistive devices: Using a walker or cane can help prevent falls.
Adjustments to furniture and home fittings: Higher chairs and devices such as levers that make it easier to turn faucet knobs, for example, can help.
Talking to an employer: It may be possible to make adjustments to the workplace or arrange for more flexible hours.
Supplements
Some research has suggested that people with low vitamin D levels have a higher risk of OA. Also, in people with a low vitamin C intake, the disease may progress more rapidly.
Low levels of vitamin K and selenium may also contribute, but confirming these findings will require further research.
Some people use supplements for OA, including:
- omega-3 fatty acids
- calcium
- vitamin D
The American College of Rheumatology note that there is not enough evidence to support the safety and effectiveness of these supplements for OA. They recommend asking a doctor before using them.
Outlook
OA is a common disease that causes joints to deteriorate, leading to pain and stiffness. It tends to appear during middle age or later.
There is currently no cure, but researchers are looking for ways to slow or reverse the damage. Lifestyle remedies and pain relief medications can help manage it.