Medical myths: All about heart disease
This week’s edition of Medical Myths will focus its beams on the many half-truths and misconceptions that surround heart disease. Among other topics, we cover smoking, coughing, exercising, supplements, and statins.
Globally, heart disease is the number one cause of death. It is responsible for 17.9 million deaths each year.
According to the Centers for Disease Control and Prevention (CDC), in the United States, one person dies every 36 seconds from cardiovascular disease. Heart disease accounts for 1 in 4 deaths in the U.S.
1. Young people do not need to worry about heart disease
It is true that heart disease is more likely to affect people over the age of 65, but 4–10% of heart attacks occur in people under the age of 45 years, mainly in men. In addition, it is how we live our lives as children, adolescents, and adults that lays the groundwork for heart health as we age.
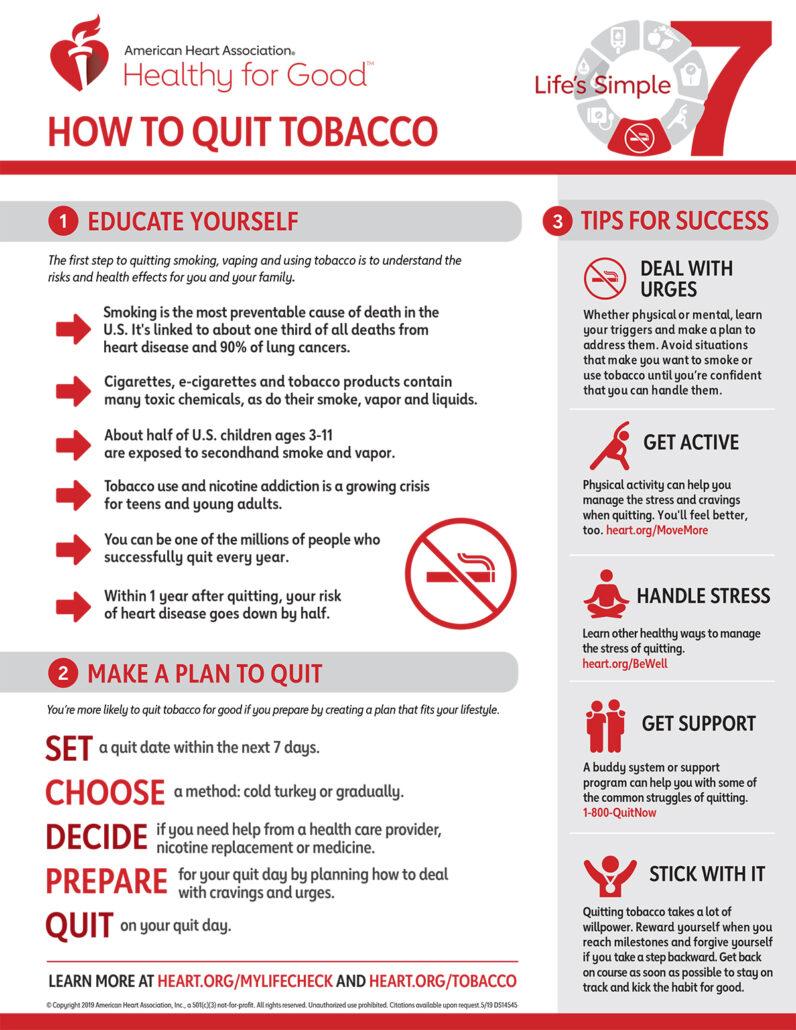
For instance, eating a diet that is high in trans and saturated fats or smoking tobacco slowly increases the risk of heart disease as we age. Changes to lifestyle today build the foundation for a healthier heart in later life.
In the U.S. as a whole, heart disease mortality has slowly dropped since the 1970s , although the trend seems to be slowing. However, in some regions, rates have increased.
One study that investigated heart disease mortality in different age groups in the U.S. found that “over 50% of counties experienced increases in heart disease mortality from 2010 through 2015 among adults aged 35–64 years.”
2. People should avoid exercise if they have heart disease
This is a myth. Exercise helps strengthen the heart muscle and improve blood flow around the body.
In August 2020, the European Society of Cardiology published guidelines on exercise in patients with cardiovascular disease. Prof. Sanjay Sharma, who was involved in creating the guidelines, explains:
“The chance of exercise triggering a cardiac arrest or heart attack is extremely low.” However, he also adds a note of caution: “People who are completely inactive and those with advanced heart disease should consult their doctor before taking up sports.”
3. I take cholesterol-lowering drugs, so I can eat whatever I like
Some drugs, such as statins, reduce the level of cholesterol in the blood. However, this does not mean that a person who is taking statins can consume foods containing saturated fats with abandon.
Cholesterol is either consumed in the food that you eat or produced in the liver. Statins block an enzyme in the liver that is necessary for producing cholesterol, reducing overall blood cholesterol levels. However, this means that ingested cholesterol can still make it into the blood.
In short, statins may just be able to override the adverse effects of a poor diet, but a poor diet will increase risk of other independent risk factors for heart disease, such as obesity, hypertension, and diabetes.
4. Heart disease runs in my family, so there is nothing I can do to stop it
If close family members have experienced heart disease, it could mean that you have an increased risk. However, it is not set in stone, and there are a number of ways to reduce the risk, even for people with a genetic susceptibility.
These include eating a healthful diet, stopping smoking, managing blood pressure, and exercising regularly.
It is also worth noting that if heart disease runs in the family, it may not be a sign of genetic susceptibility. Families tend to share lifestyle factors, such as diet and exercise habits, both of which can impact the risk of heart disease.
5. Vitamins can prevent heart disease
Although most vitamins, taken at the recommended doses, are unlikely to be bad for heart health, there is no evidence that taking any vitamin supplements can reduce the risk of heart disease. And they certainly cannot replace a healthful diet and regular exercise.
For instance, a systematic review and meta-analysis looked for associations between multivitamin and mineral supplements and a number of cardiovascular outcomes, including coronary heart disease and stroke.
The analysis, published in 2018, took data from 18 existing studies, including 2,019,862 participants.
The authors concluded that multivitamin and mineral “supplementation does not improve cardiovascular outcomes in the general population.”
According to Victoria Taylor, the nutrition lead at the British Heart Foundation: “There are no shortcuts when it comes to nutrition — supplements are not a replacement for healthy food. You might be prescribed a vitamin or mineral supplement by a health professional for other reasons, but we do not recommend people take multivitamins to help prevent heart and circulatory diseases.”
6. I have smoked for years, there is no point stopping now
This is a myth. Smoking tobacco is a major cause of heart disease. As soon as a person stops smoking, the health benefits begin. The National Institute on Aging write:
“It doesn’t matter how old you are or how long you’ve been smoking, quitting smoking at any time improves your health. When you quit, you are likely to add years to your life, breathe more easily, have more energy, and save money.”
They also explain that you will lower the risk of heart attack and stroke and have better circulation.
7. Heart disease only really affects men
This is a myth, as heart disease is the leading cause of death in both men and women. In 2017 in the U.S., 24.2% of men and 21.8% of women died from heart disease.
However, when strokes, which have similar risk factors, are added in, the figures are even more similar between men and women: 28.7% of men and 28% of women died from heart disease or stroke.
It is a common misconception that only men are affected by heart disease. It is true that men tend to develop cardiovascular disease at an earlier age than women and have a greater risk of coronary heart disease. However, women have a higher risk of stroke.
One paper explains, “Although the incidence of [cardiovascular disease] in women is usually lower than in men, women have a higher mortality and worse prognosis after acute cardiovascular events.”
8. Cardiac arrest and heart attack are the same
Heart attacks and cardiac arrests are not the same thing. A heart attack is a circulation problem. It occurs when the coronary artery, which carries oxygenated blood to the muscles of the heart, becomes blocked.
A cardiac arrest is an “electrical problem,” where the heart stops pumping blood around the body effectively. Cardiac arrests are often caused by a heart attack.
During a heart attack, an individual is likely to be conscious. During a cardiac arrest, they are almost always unconscious. Both are a medical emergency.
9. Coughing during a heart attack can save your life
According to some sources, coughing vigorously during a heart attack — so-called cough CPR — can save your life.
This is an internet distortion of a paper published over 40 years ago, which showed that patients who had a cardiac arrest during arteriography in hospital and who coughed every 1–3 seconds stayed conscious for an additional 39 seconds.
There is no evidence that this technique works in the community for heart attacks that are not induced by medical procedures.
According to Christopher Allen, a senior cardiac nurse:
“The absolute priority when you think you or someone else is having a heart attack is to call [the emergency services]. This way, paramedics can assess and aid you, and you’ll get to hospital as fast as possible. There is no medical evidence to support ‘cough CPR.’”
10. People with heart disease should avoid eating all fat
A person with cardiovascular disease certainly should reduce their intake of saturated fats — which are found in foods such as butter, biscuits, bacon, and sausages — and partially hydrogenated and trans fats, which are found in foods such as baked goods, frozen pizzas, and microwave popcorn.
However, unsaturated fats can provide benefits. For instance, there is some evidence that omega-3, which is a polyunsaturated fat, might protect heart health.
The American Heart Association recommend “that all adults eat fish (particularly fatty fish) at least 2 times a week. Fish is a good source of protein and is low in saturated fat. Fish, especially oily species like mackerel, lake trout, herring, sardines, albacore tuna, and salmon, provide significant amounts of the two kinds of omega-3 fatty acids shown to be cardioprotective, eicosapentaenoic acid and docosahexaenoic acid.”
They also recommend eating plant-derived omega-3 fatty acids. These can be found in tofu and other forms of soybeans; walnuts, flaxseeds, and their oils; and canola oil.
The take-home
Heart disease is common, but it is not inevitable. There are lifestyle changes that we can all implement to reduce the risk of developing cardiovascular problems, whatever our age.