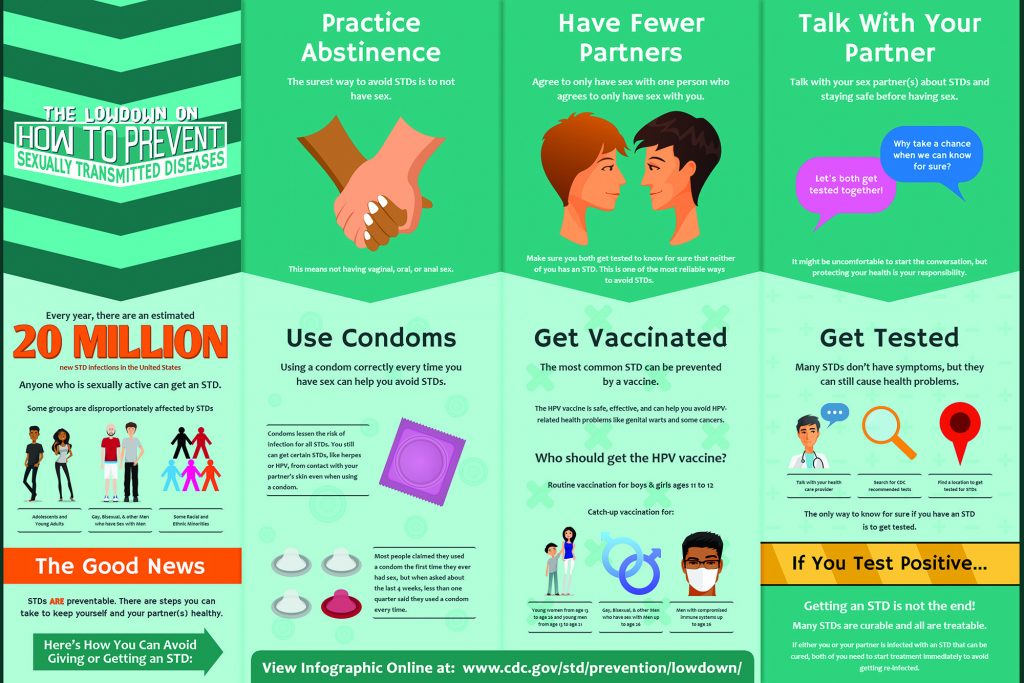
Sexually Transmitted Disease Surveillance, 2020 serves as a reminder that STDs remain a significant public health concern, even in the face of a pandemic. In 2020, COVID-19 significantly affected STD surveillance and prevention efforts. This report reflects the realities of a strained public health infrastructure, while simultaneously providing the most current data on reported cases of STDs in the United States. Trends presented in this report should be interpreted cautiously.
Chlamydia
In 2020, a total of 1,579,885 cases of Chlamydia trachomatis infection were reported to the CDC, making it the most common notifiable sexually transmitted infection in the United States for that year. This case count corresponds to a rate of 481.3 cases per 100,000 population, a decrease of 13% compared with the rate in 2019. During 2019–2020, rates of reported chlamydia decreased among both males and females, in all regions of the United States, and, except for rates among non-Hispanic persons of multiple races, among all racial/Hispanic ethnicity groups.
Decreases in rates of reported chlamydia in 2020 are unlikely due to a reduction in new infections. As chlamydial infections are usually asymptomatic, case rates are heavily influenced by screening coverage. During the COVID-19 pandemic, many health care clinics limited in-person visits to patients with symptoms or closed entirely, and it is likely that preventive health care visits where STD screening usually happens, such as annual reproductive health visits for young women, decreased. During the initial shelter-in-place orders in March and April of 2020, the number of chlamydia cases decreased substantially when compared to the number of cases reported in 2019 and the deficit persisted throughout the year.
Rates of reported chlamydia are highest among adolescents and young adults. In 2020, almost two-thirds (61%) of all reported chlamydia cases were among persons aged 15–24 years. Decreases in rates of diagnosed and reported chlamydia during 2020 were most noticeable among females aged 15–24 years, one of the populations targeted for chlamydia screening. Although still high, rates of reported chlamydia decreased 15% among 15–19-year-old females and decreased 10% among 20–24-year-old females during 2019–2020.
Deaths from Excessive Alcohol Use in the United States
Excessive alcohol use was responsible for more than 140,000 deaths in the United States each year during 2015–2019, or more than 380 deaths per day. These estimates are from the CDC’s Alcohol-Related Disease Impact (ARDI) application, using a new methodology. The ARDI application shows estimates of alcohol-attributable deaths and years of potential life lost from 58 conditions by age, sex, and state. See how use of this methodology would affect previous ARDI estimates.
Each year, deaths from excessive drinking:
- Shortened the lives of those who died by an average of 26 years, for a total of nearly 3.6 million years of potential life lost.
- Usually involved adults aged 35 or older and males.
- Were mostly due to health effects from drinking too much over time, such as various types of cancer, liver disease, and heart disease.
- Led to premature deaths. Deaths from drinking too much in a short time (from causes such as motor vehicle crashes, poisonings involving substances in addition to alcohol, and suicides) accounted for more than half of the years of potential life lost.
Excessive drinking is a leading cause of preventable death in the United States, and it is also costly. It cost the nation $249 billion in 2010 (the most recent year of data available).
Everyone Can Help Prevent Excessive Alcohol Use
You can:
- Choose not to drink or to drink in moderation by limiting intake to 2 drinks or less in a day (if you’re a man) and 1 drink or less in a day (if you’re a woman), on days when alcohol is consumed. Some people should not drink any alcohol, including if they:
- Are pregnant or might be pregnant.
- Are younger than 21.
- Have certain medical conditions or are taking certain medicines that can interact with alcohol.
- Are recovering from an alcohol use disorder or are unable to control the amount they drink.
- Check your drinking, and learn more about the benefits of drinking less alcohol.
- Support effective community strategies to prevent excessive alcohol use, such as those recommended by the Community Preventive Services Task Force.
- Not serve or provide alcohol to anyone who should not be drinking, including people younger than 21 or those who have already consumed too much.
- Talk with your health care provider about your drinking behavior and request counseling if you drink too much.
Check your drinking. This quick assessment can help.
States and communities can:
- Implement effective strategies for preventing excessive alcohol use to reduce the availability and accessibility of alcohol and increase its price, including regulating the number and concentration of alcohol outlets, limiting days and hours of alcohol sales, and avoiding further privatization of alcohol sales. Check out CDC’s alcohol outlet density measurement resources.
- Enforce existing laws and regulations about alcohol sales and service.
- Partner with law enforcement, community groups, health departments, and doctors, nurses, and other health care providers to reduce excessive drinking and related harms.
- Track the role of alcohol in injuries and deaths, with more routine alcohol toxicology testing among patients and people who have died.
- Routinely monitor and report on measures of excessive alcohol use and the status of effective alcohol policies.
Healthy Weight
Achieving and maintaining a healthy weight includes healthy eating, physical activity, optimal sleep, and stress reduction. Several other factors may also affect weight gain.
Healthy eating features a variety of healthy foods. Fad diets may promise fast results, but such diets limit your nutritional intake, can be unhealthy, and tend to fail in the long run.
How much physical activity you need depends partly on whether you are trying to maintain your weight or lose weight. Walking is often a good way to add more physical activity to your lifestyle.
Managing your weight contributes to good health now and as you age. In contrast, people who have obesity, compared to those with a healthy weight, are at increased risk for many serious diseases and health conditions. See examples of programs that can help.
Helping people maintain a healthy weight is part of CDC’s work to achieve health equity.
Health Equity
In the United States, chronic diseases are leading causes of death and disability, and some groups are affected more than others. For example, obesity is a chronic disease that increases the risk of heart disease, type 2 diabetes, and many types of cancer. The US prevalence of obesity varies by racial and ethnic group, education, age, location, and physical ability.
What Is CDC’s DNPAO Doing?
CDC’s Division of Nutrition, Physical Activity, and Obesity (DNPAO) leads the nation’s public health efforts to promote good nutrition, regular physical activity, and a healthy weight for everyone. These priorities help improve overall health and well-being and prevent, delay, and manage many chronic diseases.
Yet everyone does not have access to affordable, nutritious food and safe places to be physically active. We work with partners and state, tribal, local, and territorial health agencies and organizations to remove environmental and systemic barriers to health. Health equity is when everyone has the opportunity to be as healthy as possible. Our health equity work focuses on three areas:
- Leading domestic and international programs and initiatives.
- Applying data from monitoring and research.
- Providing health equity resources.
What Influences Health Equity?
Social Determinants of Health
The conditions in which we are born, live, learn, work, play, worship, and age are social determinants of health (SDOH). Examples include access to safe and affordable housing, quality education, and quality health care.
Differences in SDOH contribute to persistent chronic disease disparities among racial, ethnic, and socioeconomic groups as well as in different geographies and among people with different physical abilities.
Racism
Racism is a system of structures, policies, practices, and norms that assigns value and determines opportunity because of the way people look or the color of their skin. This results in conditions that unfairly give advantages to some and disadvantages to others. These advantages and disadvantages are passed down through generations.
Racism, both interpersonal and systemic, limits the ability for some groups to build wealth by determining who owns land, buys houses, gets a quality education, and gets living wage jobs. Racism also affects access to quality health care.
Aligned Work
Within the CDC, DNPAO is part of the National Center for Chronic Disease Prevention and Health Promotion. Our work is aligned with the center’s focus on five social determinants of health: built environment, community-clinical linkages, food and nutrition security, social connectedness, and tobacco-free policies.
Along with more than 25 federal agencies, CDC participates in an Interagency Workgroup developing a Long-Term Recovery and Resilience plan [PDF-181KB]. The purpose is toalign federal actions, outline strategies to improve vital conditions, support community and individual recovery from the effects of COVID-19, and positively affect health and well-being over the next 10 years and beyond. Vital conditions are characteristics of places and institutions that communities and individuals need to reach their full potential and serve as the guiding framework for the federal plan. Vital conditions include basic needs for health and safety, life-long learning, a thriving natural world, reliable transportation, humane housing, and a community-centered environment with meaningful work and wealth.
Healthy People 2030, a Department of Health and Human Services project, offers measurable, objectives as well as developmental and research objectives to improve health and well-being. The social determinants of health objectives include economic stability, education access and quality, health care access and quality, neighborhoods that promote health and safety, and increased social and community support
The World Health Organization works to address social determinants of health by compiling and disseminating evidence on what works to address these determinants to help build capacity and advocate for more action.
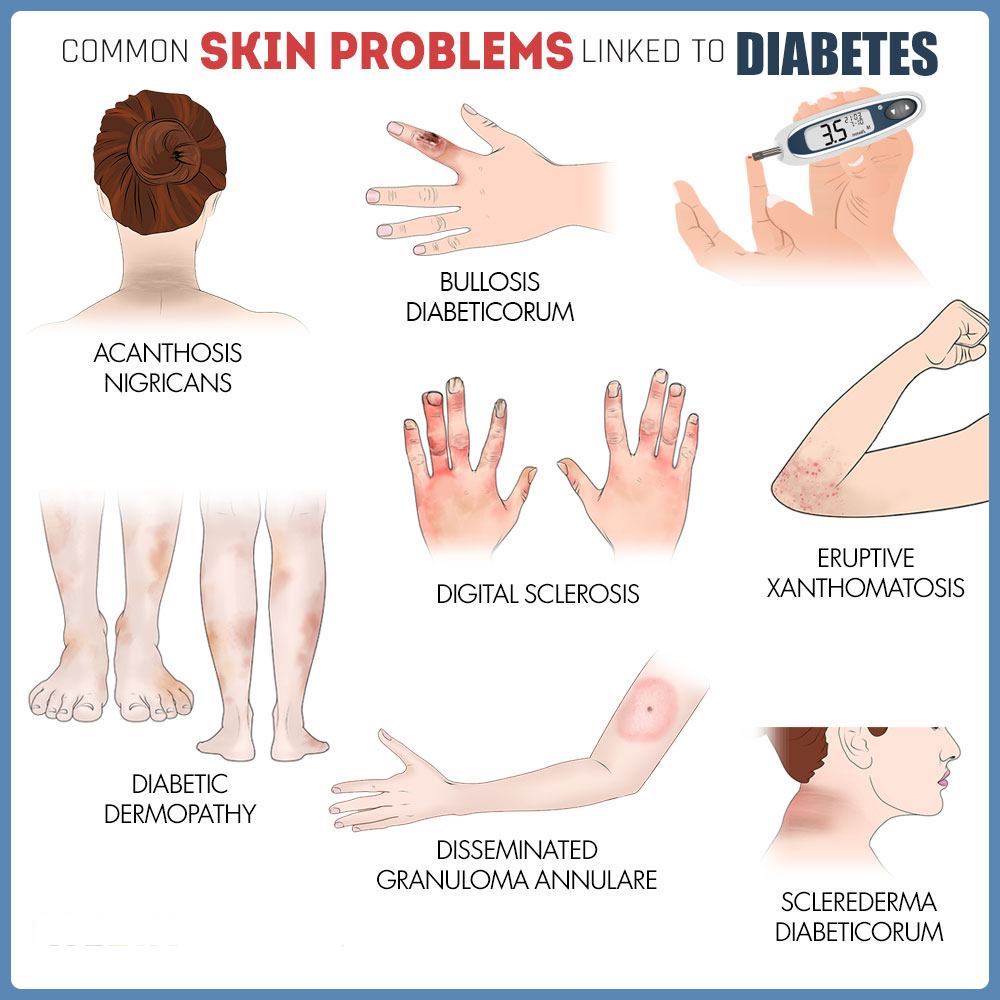
Diabetes and Your Skin
If you notice any unusual changes in your skin, it’s important to see your doctor. Early diagnosis and treatment are key to preventing serious complications.
Did you know that diabetes can affect many parts of your body, including your skin? In fact, skin changes are one of the most common signs of diabetes. Learn about the signs of diabetes that can appear on your skin.
The skin is the largest organ of the human body. It’s packed with nerves and blood vessels that allow us to sense touch, temperature, pain, and pressure. Diabetes can affect the nerves and blood vessels in your body, including those in your skin. Changes in your skin can be a sign that something is going on beneath the surface.
When diabetes affects your skin, it’s often a sign that your blood sugar levels are too high over time. Some skin changes can appear even before you’ve been diagnosed with diabetes. Others could be a sign that your diabetes treatment needs to be adjusted. Either way, you’ll want to make an appointment with a doctor to be screened for diabetes or to talk about adjusting your treatment. They can help you prevent serious complications with your skin and other parts of your body.
Keep reading to learn about 9 skin conditions that can occur with diabetes and what you can do to treat or prevent them.
1. Acanthosis nigricans (AN)
This skin condition causes a dark patch or band of velvety skin that can appear in body creases such as your neck, armpits, or groin. Sometimes the patches can also appear on your hands, elbows, or knees.
What causes it: AN is a sign of insulin resistance and can be a sign of prediabetes or type 2 diabetes. It is common in people who have obesity.
What to do: Some creams can help make the spots look better, but the most effective treatment is to address the root cause, like obesity or insulin resistance. Lifestyle changes such as being physically active and maintaining a healthy weight can help reverse insulin resistance.
2. Diabetic dermopathy
This condition is also known as shin spots, and it’s harmless. The spots look like red or brown round patches or lines in the skin and are common in people with diabetes. They appear on the front of your legs (your shins) and are often confused with age spots. The spots don’t hurt, itch, or open up.
What causes it: Diabetes can cause changes in small blood vessels that reduce blood supply to the skin.
What to do: This skin condition is harmless and doesn’t need treatment. If you do have any concerns about shin spots, talk to your doctor.
3. Necrobiosis lipoidica
This condition causes yellow, reddish, or brown patches on your skin. It usually begins as small, raised bumps that look like pimples. As it gets worse, the bumps turn into patches of swollen, hard skin. This skin condition is rare, but if it does develop it can be itchy and painful.
What causes it: The cause of necrobiosis lipoidica isn’t completely clear, but women are more likely to have it than men. It usually develops when changes in fat and collagen (a fiber-like protein in your body) happen beneath the skin’s surface.
What to do: There is no cure for the condition, so treatment is focused on managing signs and symptoms. In the early stages, topical steroid creams can be used to keep it from getting worse. You’ll want to talk with your doctor so they can find the right treatment plan for you.
4. Bullosis diabeticorum (diabetic blisters)
This condition looks like burn blisters. They can develop on your lower legs and feet, and sometimes on your arms and hands. They can look scary, but they are painless and usually heal on their own.
What causes it: The cause of diabetic blisters is unknown. They can appear with no known injury to the skin. You’re more likely to get diabetic blisters if your blood sugars levels are high over time.
What to do: Most blisters heal on their own without leaving a scar. Daily inspection of your feet and skin is the best way to find early signs of blisters. The best way to prevent them from developing or getting worse is to bring your blood sugar down to normal levels.
5. Eruptive xanthomatosis
This condition causes small, reddish-yellow bumps on the back of your hands, feet, arms, legs, and buttocks. They can be tender and itchy.
What causes it: This condition is rare. It’s caused by having high levels of cholesterol and triglycerides (fat in the blood).
What to do: The best treatment is to bring blood fat levels under control. Your doctor may also want to prescribe medicine to help lower your cholesterol. Talk to your doctor about having your cholesterol checked so that you can take steps to prevent high cholesterol.
6. Digital sclerosis
This condition starts with tight, thick, waxy skin on your fingers and can cause your finger joints to become stiff and hard to move. If blood sugar levels remain high, digital sclerosis can cause your skin to become hard, thick, and swollen and can spread throughout your body.
What causes it: This condition is more common in people with type 1 diabetes who have high blood sugar levels.
What to do: The only treatment for digital sclerosis is to bring blood sugar levels down into the normal range. Physical therapy may help improve the range of motion of affected joints.
7. Bacterial infections
Bacterial infections cause tissue (cells that make up organs and other body parts) to become inflamed, hot, swollen, red, and painful. Common bacterial infections include those on the eyelids, hair follicles, and fingernails.
What causes it: Anyone can get a bacterial infection, but people with diabetes tend to get more than people without diabetes. Bacteria thrive when there is too much glucose (sugar) in the body. A common type of bacteria responsible for bacterial infections in people with diabetes is staphylococcus (staph).
What to do: Bacterial infections usually can be treated with antibiotics. Keeping your blood sugar levels within the normal range can help you avoid infections. Healthy eating, getting physical activity, and taking your medicine as instructed can help you manage your blood sugar.
8. Fungal infections
Fungal infections create itchy rashes surrounded by tiny red blisters and scales. They usually develop in warm, moist folds of the skin. Common fungal infections include jock itch, athlete’s foot, ringworm, and vaginal infections.
What causes it: Like bacterial infections, anyone can get a fungal infection, but they are common in people with diabetes. Fungal infections are more likely to occur when blood sugar levels are high.
What to do: Talk to your doctor about prescription or over-the-counter medicine that can help treat fungal infections. Keeping blood sugar levels within the normal range by checking your blood sugar often, eating healthy, and getting regular exercise is the best way to prevent fungal infections.
9. Dry, itchy skin
This skin condition is common, even for people who don’t have diabetes. But dry, itchy skin can be a result of poor circulation, which is more likely when you have diabetes.
What causes it: Too much sugar in the blood causes the body to pull fluid from its cells so that it can produce enough urine to remove the excess sugar. This can make your skin dry.
What to do: You’ll want to monitor your blood sugar levels and keep them in your target range as much as possible. It also helps if you limit your time in the shower, use mild soaps, and use lotion after showering. Exercise is one of the best ways to improve circulation—and has many other health benefits.
Be Good to Your Skin
Skin is a good indicator of health. If you notice any unusual changes in your skin, it’s important to see your doctor. Early diagnosis and treatment are key to preventing serious complications from skin problems caused by diabetes.
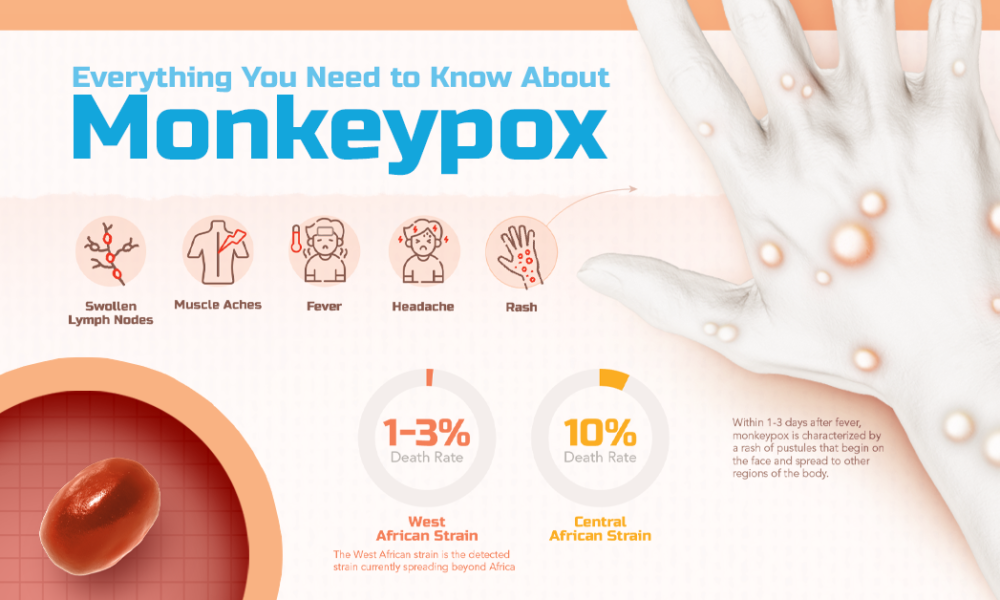
What is Monkeypox?
Monkeypox is a rare disease caused by infection with the monkeypox virus. Monkeypox virus belongs to the Orthopoxvirus genus in the family Poxviridae. The Orthopoxvirus genus also includes variola virus (which causes smallpox), vaccinia virus (used in the smallpox vaccine), and cowpox virus. Monkeypox is not related to chickenpox.
Monkeypox was first discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research. Despite being named “monkeypox”, the source of the disease remains unknown. However, African rodents and non-human primates (like monkeys) may harbor the virus and infect people.
The first human case of monkeypox was recorded in 1970. Since then, monkeypox has been reported in people in several other central and western African countries. Prior to the 2022 outbreak, nearly all monkeypox cases in people outside of Africa were linked to international travel to countries where the disease commonly occurs, or through imported animals.
Sign & Symptoms:
Monkeypox is a rare disease caused by infection with the monkeypox virus. Monkeypox virus is part of the same family of viruses as smallpox. Monkeypox symptoms are similar to smallpox symptoms, but milder; and monkeypox is rarely fatal. Monkeypox is not related to chickenpox.
Symptoms of monkeypox can include:
- Fever
- Headache
- Muscle aches and backache
- Swollen lymph nodes
- Chills
- Exhaustion
- A rash that can look like pimples or blisters that appears on the face, inside the mouth, and on other parts of the body, like the hands, feet, chest, genitals, or anus.
- The rash goes through different stages before healing completely. The illness typically lasts 2-4 weeks.
Sometimes, people get a rash first, followed by other symptoms. Others only experience a rash.
Prevention:
There are number of measures that can be taken to prevent infection with monkeypox virus:
- Avoid contact with animals that could harbor the virus (including animals that are sick or that have been found dead in areas where monkeypox occurs).
- Avoid contact with any materials, such as bedding, that has been in contact with a sick animal.
- Isolate infected patients from others who could be at risk for infection.
- Practice good hand hygiene after contact with infected animals or humans. For example, washing your hands with soap and water or using an alcohol-based hand sanitizer.
- Use personal protective equipment (PPE) when caring for patients.
Practice good hand hygiene after contact with infected animals or humans.
JYNNEOSTM (also known as Imvamune or Imvanex) is an attenuated live virus vaccine which has been approved by the U.S. Food and Drug Administration for the prevention of monkeypox. On November 3, 2021, the Advisory Committee on Immunization Practices (ACIP) voted to recommend JYNNEOS pre-exposure prophylaxis as an alternative to ACAM2000 for certain persons at risk for exposure to orthopoxviruses.
Diarrhea and Swimming
You can get sick with diarrhea if you swallow contaminated recreational water—water in pools, hot tubs, water playgrounds, or oceans, lakes, and rivers. In fact, diarrhea is the most common illness reported for outbreaks linked to recreational water.
Which germs in recreational water cause diarrhea?
You can get diarrhea from germs such as
- Crypto (short for Cryptosporidium)
- Giardia
- Shigella
- Norovirus
- E. coli O157
These germs can survive in properly chlorinated water for minutes to days, depending on the germ.
How do germs that cause diarrhea spread in recreational water?
If someone is sick and has diarrhea in the water, millions of germs can contaminate the water. These germs can make other people sick if they swallow even a small amount of contaminated water. Swallowing 10 or fewer germs can make people sick. Germs can also get in the water if swimmers have poop, even tiny amounts, on their bottoms.
Pool chemicals and filters help kill germs
Filters and disinfectants (chemicals that disinfect the water, such as chlorine or bromine) work together to help kill germs in pools, hot tubs, and water playgrounds. Filters remove debris (such as leaves), which use up the disinfectant in the water. Pool staff make sure chlorine or bromine is at the level needed to kill most germs in the water within minutes. You can still be exposed to germs during the time it takes for the water to go through filters and for the disinfectant to kill germs. You can also get diarrhea from germs that are hard to kill, such as Crypto. Crypto stays alive for more than 7 days, even if water is properly filtered and disinfected.
Many places with pools use one filtration system for more than one pool, which causes water from multiple pools to mix. This means germs from one person’s body could contaminate the water in more than one pool.
How do I protect myself and those I care about?
We all share the water we swim, play, or relax in. Each of us can help protect ourselves, our families, and our friends from germs that can cause diarrhea.
Take the following steps when swimming in any type of water:
- Stay out of the water if you are sick with diarrhea.
- If you have Crypto, don’t go in the water until 2 weeks after diarrhea has completely stopped.
- Don’t poop in the water.
- Don’t swallow the water.
- Take kids on bathroom breaks and check diapers every hour.
- Change diapers away from the water’s edge to keep germs from getting in the water. Wash your hands after.
Before going in pools, water playgrounds, and hot tubs, also take these steps:
- Use test strips to make sure the water has proper free chlorine (amount of chlorine available to kill germs) or bromine level and pH.
- Free chlorine level: at least 1 part per million (ppm) in pools and water playgrounds and at least 3 ppm in hot tubs
- Bromine level: at least 3 ppm in pools and water playgrounds and at least 4 ppm in hot tubs
- pH (affects how well chlorine and bromine can kill germs): 7.2–7.8
- Most superstores, hardware stores, and pool supply stores sell test strips. Follow the directions on the test strip package.
- Shower before you get in the water.
- A 1-minute shower removes most of the dirt, sweat, and oils on your body that use up chlorine or bromine needed to kill germs.
Follow these and other healthy swimming steps to help protect you and those you care about from getting sick.