Pregnant during the COVID-19 crisis
The COVID-19 pandemic has changed the healthcare landscape for many patient populations — including pregnant women.
To mark Mental Health Awareness Month this May, we’re bringing you research-backed information to help support the mental well-being of you and your loved ones during this difficult time.
Altered hospital policies, concerns about contracting the SARS-CoV-2 virus, and changes to doctors’ office hours have all affected pregnancy.
Information regarding pregnancy and COVID-19 is continually evolving. This article will cover the currently available information relating to pregnancy during the pandemic.
Pregnancy can be an exciting time, but also one of uncertainty. The COVID-19 pandemic understandably adds further stress and may cause anxiety in some people.
During pregnancy, signs and symptoms of high stress include:
- changes in appetite
- frequent feelings of fear and worry about the pregnancy and delivery
- poor quality sleep
- problems concentrating
Pregnant women may wish to try the following stress-relieving practices and tips:
- Refrain from looking at physical media or watching the news around the clock. Instead, limit the news to key times of the day, such as the morning or before dinner, leaving the evenings free for unwinding and promoting sleep.
- Ask a doctor or midwife about online antenatal classes, which are excellent places to meet and talk to other pregnant women.
- Try meditating, deep breathing, or gentle stretching.
- Take care of key relationships by connecting with friends and family over the phone or through video conferences.
- Get enough sleep by going to bed at a consistent time and limiting screen time beforehand.
- Maintain a healthful diet and engage in regular exercise. Eating well and staying active can help the body stay healthy in times of mental ill health.
- Take up a new hobby or rediscover an old one, such as playing an instrument, learning a language, or reading. People may also enjoy making blankets, clothes, or handmade toys for the coming baby, or decorating a nursery.
- Make use of online support groups and forums for pregnant women and new parents.
- Consider online counseling. Therapy can be helpful for anyone experiencing anxiety, depression, or stress.
- Ask for extra help — this may mean that a partner takes a greater share of caring for the children, if applicable, or that a neighbor does the grocery shopping and drops the bags outside the door.
If a woman is experiencing significant mental distress, it is vital to speak to a doctor, midwife, or counselor.
Depression during pregnancy is common but treatable. Even if they are physical distancing, pregnant women do not have to face depression or other mental health concerns alone.
Physical distancing while pregnant
Avoiding contact with others, especially large groups of people, can reduce the transmission of the coronavirus.
Many areas have enacted shelter-at-home or safer-at-home policies that discourage people from going outside except for essential travel, such as going to the grocery store or pharmacy or making other necessary visits.
It is essential to keep attending prenatal appointments, but be aware that some of these appointments may occur over the phone.
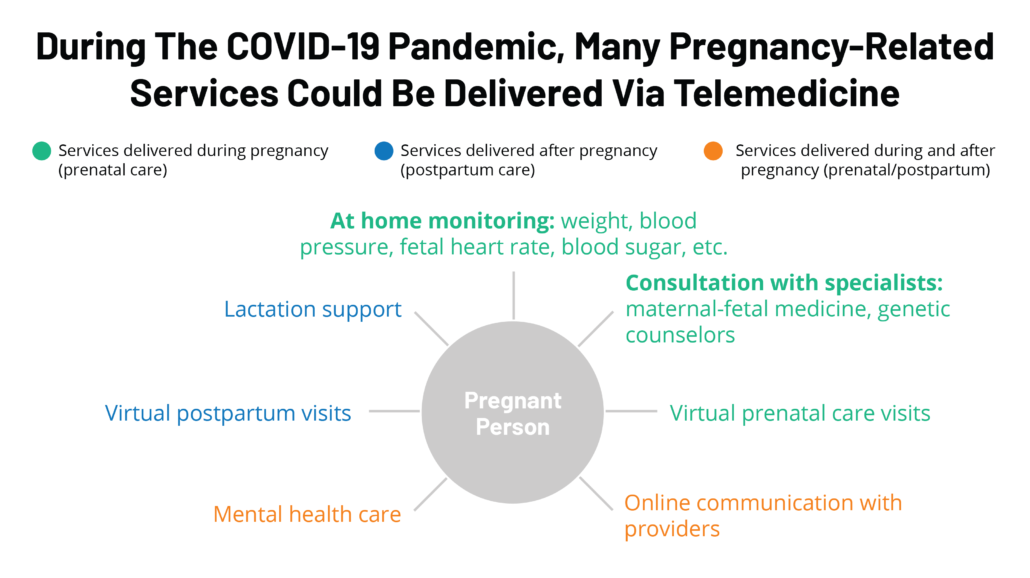
Modern technology enables doctors’ offices to change the way in which they help people, including pregnant women.
The American College of Obstetricians and Gynecologists recommend that pregnant women talk with a doctor to determine how often they should go for in-person visits.
Our doctors offer online video call visits called telemedicine. They may recommend spacing out ultrasound appointments or other in-person visits to reduce a woman’s risk for transmission.
If possible, having a partner or delivery service secure key items can help reduce a pregnant woman’s exposure to the public.
People should always wash their hands when returning from the grocery store or a walk outside.
COVID-19 effects during pregnancy
As COVID-19 is a new and developing health crisis, experts have not yet identified its effects on pregnancy. They remain unsure whether pregnant women are more at risk of getting COVID-19 or experiencing more severe symptoms and whether they might pass the virus to the baby.
According to the World Health Organization (WHO), no evidence currently exists to suggest that pregnant women are at higher risk of experiencing severe COVID-19 symptoms than the general population.
A small study of nine pregnant women in their third trimester with COVID-19 and pneumonia symptoms in Wuhan, China, found that one baby tested positive for the virus 36 hours after birth.
However, tests of the woman’s placenta and umbilical cord were negative, which could mean that the newborn contracted the virus after birth, rather than in the womb. This sample size was very small, which makes drawing conclusions difficult.
Another study of 38 pregnant women testing positive for COVID-19 in China did not find that their symptoms were more severe than those affecting the general population.
The study did not report any maternal deaths or the transmission of COVID-19 to any babies.
When to self-isolate
If a pregnant woman has symptoms that resemble those of COVID-19, such as coughing, fever, or shortness of breath, she should call a doctor.
The doctor can make recommendations about whether or not COVID-19 testing is necessary.
If the woman’s symptoms are mild, a doctor will likely recommend that she self-isolate at home.
Home treatment includes taking acetaminophen for fever relief, resting, and drinking plenty of water.
A high fever or difficulty breathing are signs that urgent care is necessary. Try to call the hospital before arriving at the emergency room so that they can take any necessary precautions.
Do you have to give birth alone in the hospital?
Some hospitals in the United States have prohibited visitors for the foreseeable future — including during childbirth — to protect healthcare staff and other patients from the virus. The number of support people who may enter the delivery room can vary from hospital to hospital, however.
Questions to ask a doctor
The pandemic has resulted in many pregnant women experiencing changes to their birth plan, which can cause stress and uncertainty.
Having all the necessary information may help them feel in control and reduce anxiety.
Questions to ask a doctor include:
- How may your office hours or accessibility change?
- Are there online alternatives to antenatal classes where I can meet and talk to other pregnant women?
- How can I ensure that I am safe when visiting my doctor’s office or going to the hospital?
- How can I expect COVID-19 concerns at the hospital to affect my delivery?
- Will there be changes in terms of the medications that I may receive or the number of people present in the delivery room?
A woman can also ask her doctor about any area-specific or condition-specific changes.
Summary
Pregnant women may feel additional stress, anxiety, or depression during the COVID-19 pandemic. But even if they are self-isolating, they do not have to face these problems alone.
It is best for pregnant women to focus on the elements that they can control, including self-care and physical distancing.
Keeping in regular contact with a doctor or midwife can also help alleviate worries about health and the birth.
Covid-19 patients recovering quickly after getting experimental drug remdesivir
COVID-19 patients on the antiviral remdesivir recovered about 30 percent faster than those on a placebo, the results of a major clinical trial showed Wednesday, as a top US scientist hailed the drug’s “clear-cut” benefit.
The patients taking part in a clinical trial of the drug have all had severe respiratory symptoms and fever, but were able to leave the hospital after less than a week of treatment, STAT quoted the doctor leading the trial as saying.
“The best news is that most of our patients have already been discharged, which is great.
“Partial data from an ongoing clinical trial is by definition incomplete and should never be used to draw conclusions about the safety or efficacy of a potential treatment that is under investigation.
There is no approved therapy for the Covid-19, which can cause severe pneumonia and acute respiratory distress syndrome in some patients. But the National Institutes of Health is organizing trials of several drugs and other treatments, among them remdesivir.
The drug, made by Gilead Sciences, was tested against Ebola with little success, but multiple studies in animals showed the drug could both prevent and treat coronaviruses related to Covid-19, including SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome).
Back in February, the World Health Organization said remdesivir showed potential against Covid-19.
Most of our patients are severe and most of them are leaving at six days, so that tells us duration of therapy doesn’t have to be 10 days.
However, the trial does not include what’s known as a control group, so it will be difficult to say whether the drug is truly helping patients recover better. With a control arm, some patients do not receive the drug being tested so that doctors can determine whether it’s the drug that is really affecting their condition.
Trials of the drug are ongoing at dozens of other clinical centers, as well. Gilead is sponsoring tests of the drug in 2,400 patients with severe Covid-19 symptoms in 152 trial sites around the world. It’s also testing the drug in 1,600 patients with moderate symptoms at 169 hospitals and clinics around the world.
Gilead said it expected results from the trial by the end of the month.
“We understand the urgent need for a COVID-19 treatment and the resulting interest in data on our investigational antiviral drug remdesivir,” the company said in a statement. But it said a few stories about patients are just that.
“The totality of the data need to be analyzed in order to draw any conclusions from the trial. Anecdotal reports, while encouraging, do not provide the statistical power necessary to determine the safety and efficacy profile of remdesivir as a treatment for Covid-19.

Who is at higher risk of CoronaVirus?
WEarly information out of China, where COVID-19 first started, shows that some people are at higher risk of getting very sick from this illness. This includes:
- Older adults
- People who have serious chronic medical conditions like:
- Heart disease
- Diabetes
- Lung disease
Get ready for COVID-19 now
Take actions to reduce your risk of getting sick
If you are at higher risk for serious illness from COVID-19 because of your age or because you have a serious long-term health problem, it is extra important for you to take actions to reduce your risk of getting sick with the disease.
- Stock up on supplies.
- Take everyday precautions to keep space between yourself and others.
- When you go out in public, keep away from others who are sick, limit close contact and wash your hands often.
- Avoid crowds as much as possible.
- Avoid cruise travel and non-essential air travel.
- During a COVID-19 outbreak in your community, stay home as much as possible to further reduce your risk of being exposed.
Have supplies on hand
- Contact your healthcare provider to ask about obtaining extra necessary medications to have on hand in case there is an outbreak of COVID-19 in your community and you need to stay home for a prolonged period of time.
- If you cannot get extra medications, consider using mail-order for medications.
- Be sure you have over-the-counter medicines and medical supplies (tissues, etc.) to treat fever and other symptoms. Most people will be able to recover from COVID-19 at home.
- Have enough household items and groceries on hand so that you will be prepared to stay at home for a period of time.
Are children actually ‘as likely’ to get COVID-19 as adults?
So far, reports have maintained that children appear to be less susceptible to infection with the new coronavirus, SARS-CoV-2, than adults. But some researchers now claim that this is not the case.
Researchers are still uncertain how susceptible children are to SARS-CoV-2.
As the new coronavirus continues to spread, the public still wonders who is most at risk of infection.
Children are a primary concern: How susceptible are they to SARS-CoV-2 infection, really?
Until now, reports in peer-reviewed journals — such as this one featured in JAMA Network last month — have suggested that children appear to be less likely to develop COVID-19 than adults.
Now, an international team of researchers — many from the Shenzhen Center for Disease Control and Prevention and Peng Cheng Laboratory, both in China — has conducted a study and reached a different conclusion.
This study is preliminary and has not yet been published in a peer-reviewed journal. This means that it has not yet undergone a thorough quality and accuracy assessment from specialists in the field.
Nevertheless, the authors have made their findings available online in preprint form.
Kids’ infection rate similar to adults’
The researchers analyzed data from people in Shenzhen, China with confirmed SARS-CoV-2 infections and data from their close contacts.
In total, they looked at 391 people with confirmed COVID-19 and 1,286 individuals who were in close contact.
The researchers’ aim was to find out whether close contacts of people with COVID-19 would test positive for SARS-CoV-2, even when they presented no obvious symptoms of the infection.
The investigators found that children under 10 who were in close contact with people who had COVID-19 demonstrated a 7.4% infection rate — very similar to the 7.9% infection rate in adults.
However, the researchers also determined that children were less likely to develop symptoms, even though they seemed just as likely as adults to contract the virus.
“Kids are just as likely to get infected [as grownups] and they’re not getting sick,” notes co-author Justin Lessler, Ph.D., from the Johns Hopkins Bloomberg School of Public Health, in Baltimore, MD.
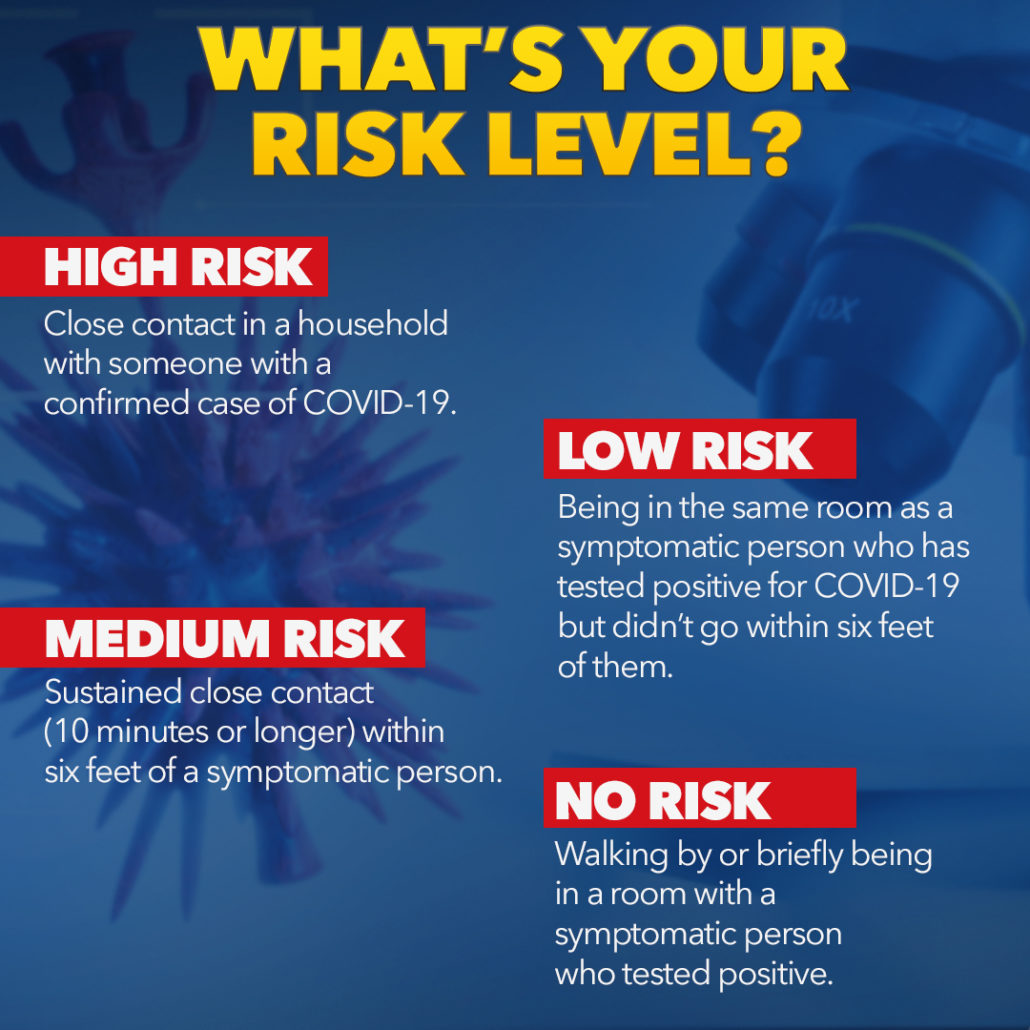
In the study paper, the researchers also report that people who lived with individuals who had diagnosed COVID-19 were more likely to develop the infection than other close contacts.
Still, they write that “Even in this group, less than 1 in 6 contacts were infected; and, overall, we observed far less than one (0.4) onward transmission per primary case.”
The researchers caution that their study “has numerous limitations,” since the data were collected by different teams following different protocols, and while definitions of what qualified as SARS-CoV-2 infection changed as understanding of the outbreak evolved.

Meditation vs Medication
Even a brief introduction to meditation can ease pain
New research has found that a 30-minute introduction to mindfulness can significantly reduce negative emotions and ease physical pain — even for those who have never practiced the technique before.
Research has shown that mindfulness and mindful acceptance have multiple benefits for physical and emotional health.
Medical News Today have covered studies showcasing the many benefits of mindfulness, from lowering blood pressure to coping with phobias.
There are two other areas that mindfulness can be helpful with: pain and emotion regulation.
Neuroscientific experiments have found that participants felt less physical pain as a result of practicing mindfulness, and researchers have suggested that this may have implications for managing chronic pain.
Further studies using brain scans have showed that mindfulness helps control emotions, which may help people overcome addiction or lower their stress levels.
However, is it possible that someone who has never meditated before can reap these benefits? This is what a group of researchers — led by Hedy Kober, an associate professor of psychiatry and psychology at Yale University in New Haven, CT — has set out to examine.
Specifically, Kober and colleagues wanted to see whether or not people with no previous mindfulness experience could benefit from a 30-minute introduction to the technique.
The results — which now appear in the journal Social, Cognitive, and Affective Neuroscience — do seem to suggest that a brief introduction to mindfulness can help ease pain and reduce negative emotions.
Mindfulness, pain, and negative emotions
Kober and team tested 17 “meditation-naïve” participants, aged 18–45, under two experimental conditions.
In one condition, the participants had to look at 30 negative images vs. 30 neutral images. In the other, they experienced painful vs. warm temperature stimuli 30 times each.
Before the experiments, the researchers trained the participants in mindfulness and how to complete the tasks for a period of 30 minutes.
During this time, the researchers instructed the participants to “react naturally, whatever [their] response might be” in the control condition, so that the scientists could establish a baseline measure of emotional response.
The researchers achieved this by performing brain imaging scans of the participants as they were completing the tasks.
Then, they asked the participants “to attend to and accept their experience as it is.” This was the mindful acceptance mindset, which consisted of two components: “attention to present moment sensation” and “non-judgmental acceptance of the sensation as it is, allowing it to exist without trying to avoid it or react to it.”
For example, in the experiments that involved the physical application of heat to the participants’ forearms, the researchers instructed them to accept the sensation in a non-judgmental way.
“[P]participants were told ‘if you feel a sensation of warmth on your forearm, you should simply attend to what is felt, without making any judgment of the ‘goodness’ or ‘badness’ of that sensation,” explain the study authors in their paper.
The effect of 30 minutes of mindfulness
The experiments revealed that the participants reported less physical pain and negative emotions in the mindfulness condition.
This coincided with changes in their brains. According to the study authors, “Emotion regulation using mindful acceptance was associated with reductions in reported pain and negative affect, reduced amygdala responses to negative images, and reduced heat-evoked responses in medial and lateral pain systems.”
Referring to the physical pain experiments, Kober explains, “It’s as if the brain was responding to warm temperature, not very high heat.”
Kober goes on to comment on the clinical significance of the findings:
“The ability to stay in the moment when experiencing pain or negative emotions suggests there may be clinical benefits to mindfulness practice in chronic conditions as well — even without long meditation practice.”
– Hedy Kober
Eating red meat and processed meat hikes heart disease, death risk: study
Drop the steak knife. After a controversial study last fall recommending that it was not necessary for people to change their diet in terms of red meat and processed meat, a large, carefully analyzed new study links red and processed meat consumption with slightly higher risk of heart disease and death, according to a new study from Northwestern Medicine and Cornell University.
Eating two servings of red meat, processed meat or poultry—but not fish—per week was linked to a 3 to 7% higher risk of cardiovascular disease, the study found. Eating two servings of red meat or processed meat—but not poultry or fish—per week was associated with a 3% higher risk of all causes of death.
“It’s a small difference, but it’s worth trying to reduce red meat and processed meat like pepperoni, bologna and deli meats,” said senior study author Norrina Allen, associate professor of preventive medicine at Northwestern University Feinberg School of Medicine. “Red meat consumption also is consistently linked to other health problems like cancer.”
“Modifying intake of these animal protein foods may be an important strategy to help reduce the risk of cardiovascular disease and premature death at a population level,” said lead study author Victor Zhong, assistant professor of nutritional sciences at Cornell, who did the research when he was a postdoctoral fellow in Allen’s lab.
The paper will be published Feb. 3 in JAMA Internal Medicine.
The new findings come on the heels of a controversial meta-analysis published last November that recommended people not reduce the amount of red meat and processed meat they eat. “Everyone interpreted that it was OK to eat red meat, but I don’t think that is what the science supports,” Allen said.
“Our study shows the link to cardiovascular disease and mortality was robust,” Zhong said.
What should we eat?
“Fish, seafood and plant-based sources of protein such as nuts and legumes, including beans and peas, are excellent alternatives to meat and are under-consumed in the U.S.,” said study coauthor Linda Van Horn, professor of preventive medicine at Feinberg who also is a member of the 2020 U.S. Dietary Guidelines Advisory committee.
The study found a positive association between poultry intake and cardiovascular disease, but the evidence so far isn’t sufficient to make a clear recommendation about poultry intake, Zhong said. Still, fried chicken is not recommended.
The new study pooled together a large diverse sample from six cohorts, included long follow-up data up to three decades, harmonized diet data to reduce heterogeneity, adjusted a comprehensive set of confounders and conducted multiple sensitivity analyses. The study included 29,682 participants (mean age of 53.7 years at baseline, 44.4% men and 30.7% non-white). Diet data were self-reported by participants, who were asked a long list of what they ate for the previous year or month.
Key findings:
- A 3 to 7% higher risk of cardiovascular disease and premature death for people who ate red meat and processed meat two servings a week.
- A 4% higher risk of cardiovascular disease for people who ate two servings per week of poultry, but the evidence so far is not sufficient to make a clear recommendation about poultry intake. And the relationship may be related to the method of cooking the chicken and consumption of the skin rather than the chicken meat itself.
- No association between eating fish and cardiovascular disease or mortality.
Limitations of the study are participants’ dietary intake was assessed once, and dietary behaviors may have changed over time. In addition, cooking methods were not considered. Fried chicken, especially deep fat-fried sources that contribute trans-fatty acids, and fried fish intake have been positively linked to chronic diseases, Zhong said.
