What is the impact of eating too much sugar?
In the short-term, eating too much sugar may contribute to acne, weight gain, and tiredness. In the long-term, too much sugar increases the risk of chronic diseases, such as type 2 diabetes and heart disease.
According to the Centers for Disease Control and Prevention (CDC), people in the United States consume too much added sugar. Added sugars are sugars that manufacturers add to food to sweeten them.
In this article, we look at how much added sugar a person should consume, the symptoms and impact of eating too much sugar, and how someone can reduce their sugar intake.
How much sugar is too much?
According to the Dietary Guidelines for Americans 2010-2015, on average, Americans consume 17 teaspoons (tsp) of added sugar each day. This adds up to 270 calories.
However, the guidelines advise that people limit added sugars to less than 10% of their daily calorie intake. For a daily intake of 2,000 calories, added sugar should account for fewer than 200 calories.
However, in 2015, the World Health Organization (WHO) advised that people eat half this amount, with no more than 5% of their daily calories coming from added sugar. For a diet of 2,000 calories per day, this would amount to 100 calories, or 6 tsp, at the most.
Symptoms of eating too much sugar
Some people experience the following symptoms after consuming sugar:
- Low energy levels: A 2019 study found that 1 hour after sugar consumption, participants felt tired and less alert than a control group.
- Low mood: A 2017 prospective study found that higher sugar intake increased rates of depression and mood disorder in males.
- Bloating: According to Johns Hopkins Medicine, certain types of sugar may cause bloating and gas in people who have digestive conditions, such as irritable bowel syndrome (IBS) or small intestinal bacterial overgrowth (SIBO).
Risks of eating too much sugar
Consuming too much sugar can also contribute to long-term health problems.
Tooth decay
Sugar feeds bacteria that live in the mouth. When bacteria digest the sugar, they create acid as a waste product. This acid can erode tooth enamel, leading to holes or cavities in the teeth.
People who frequently eat sugary foods, particularly in between mealtimes as snacks or in sweetened drinks, are more likely to develop tooth decay, according to Action on Sugar, part of the Wolfson Institute in Preventive Medicine in the United Kingdom.
Acne
A 2018 study of university students in China showed that those who drank sweetened drinks seven times per week or more were more likely to develop moderate or severe acne.
Additionally, a 2019 study suggests that lowering sugar consumption may decrease insulin-like growth factors, androgens, and sebum, all of which may contribute to acne.
Weight gain and obesity
Sugar can affect the hormones in the body that control a person’s weight. The hormone leptin tells the brain a person has had enough to eat. However, according to a 2008 animal study, a diet high in sugar may cause leptin resistance.
This may mean, that over time, a high sugar diet prevents the brain from knowing when a person has eaten enough. However, researchers have yet to test this in humans.
Diabetes and insulin resistance
A 2013 article in PLOS ONE, indicated that high sugar levels in the diet might cause type 2 diabetes over time.
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) add that other risk factors, such as obesity and insulin resistance, can also lead to type 2 diabetes.
Cardiovascular disease
A large prospective study in 2014 found that people who got 17–21% of their daily calories from added sugar had a 38% higher risk of dying from cardiovascular disease (CVD) than those who consumed 8% added sugars. For those who consumed 21% or more of their energy from added sugars, their risk for CVD doubled.
High blood pressure
In a 2011 study, researchers found a link between sugar-sweetened beverages and high blood pressure, or hypertension. A review in Pharmacological Research states that hypertension is a risk factor for CVD. This may mean that sugar exacerbates both conditions.
Cancer
Excess sugar consumption can cause inflammation, oxidative stress, and obesity. These factors influence a person’s risk of developing cancer.
A review of studies in the Annual Review of Nutrition found a 23–200% increased cancer risk with sugary drink consumption. Another study found a 59% increased risk of some cancers in people who consumed sugary drinks and carried weight around their abdomen.
Aging skin
Excess sugar in the diet leads to the formation of advanced glycation end products (AGEs), which play a role in diabetes. However, they also affect collagen formation in the skin.
According to Skin Therapy Letter, there is some evidence to suggest that a high number of AGEs may lead to faster visible aging. However, scientists need to study this in humans more thoroughly to understand the impact of sugar in the aging process.
How to eat less sugar
A person can reduce the amount of added sugar they eat by:
- checking food labels for sweeteners
- reducing foods with added sugar
- avoiding processed foods in general
Checking food labels
Added sugar and sweeteners come in many forms. Ingredients to look out for on a food label include:
- brown sugar
- fructose
- glucose
- sucrose
- maltose
- honey
- corn sweetener
- corn syrup
- high fructose corn syrup
- raw sugar
- molasses
- malt syrup
- evaporated cane juice
- agave nectar
- maple syrup
- invert sugar
- fruit juice concentrates
- trehalose
- turbinado sugar
Some of these ingredients are natural sources of sugar and are not harmful in small amounts. However, when manufacturers add them to food products, a person might easily consume too much sugar without realizing it.
Reducing foods that contain added sugar
Some food products contain large amounts of added sugars. Reducing or removing these foods is an efficient way to reduce the amount of sugar a person eats.
The Dietary Guidelines for Americans 2010–2015 state that soda and other soft drinks account for around half a person’s added sugar intake in the U.S. The average can of soda or fruit punch provides 10 tsp of sugar.
Another common source of sugar is breakfast cereal. According to EWG, many popular cereals contain over 60% sugar by weight, with some store brands containing over 80% sugar. This is especially true of cereals marketed towards children.
Swapping these foods for unsweetened alternatives will help a person lower their sugar intake, for example:
- swapping soda for water, milk, or herbal teas
- swapping sugary cereals for low sugar cereal, oatmeal, or eggs
Avoiding processed foods
Manufacturers often add sugars to foods to make them more appealing. Often, this means people do not realize how much sugar a food contains.
By avoiding processed foods, a person can get a better sense of what their food contains. Cooking whole foods at home also means someone can control what ingredients they put into their meals.
When to see a doctor
People should see their doctor if they experience the symptoms of high blood sugar. According to the NIDDK, symptoms include:
- increased thirst and urination
- increased hunger
- fatigue
- blurred vision
- numbness or tingling in the hands or feet
- unexplained weight loss
- sores that do not heal
These symptoms may indicate a person has diabetes. A doctor can test for diabetes by taking a urine sample.
People should also speak to a doctor if they experience other symptoms after eating sugar, such as bloating.
Summary
Consuming too much added sugar has many adverse impacts on health, including tiredness and weight gain, and more severe conditions, such as heart disease. Added sugars are present in many processed foods and drinks.
People can reduce their sugar intake by knowing what to look for on food labels, avoiding or reducing common sources of sugar, such as soda and cereals, and prioritizing unprocessed whole foods.
If a person is concerned about weight gain, symptoms that may indicate diabetes, or other symptoms they experience after eating sugar, they should speak to a doctor.

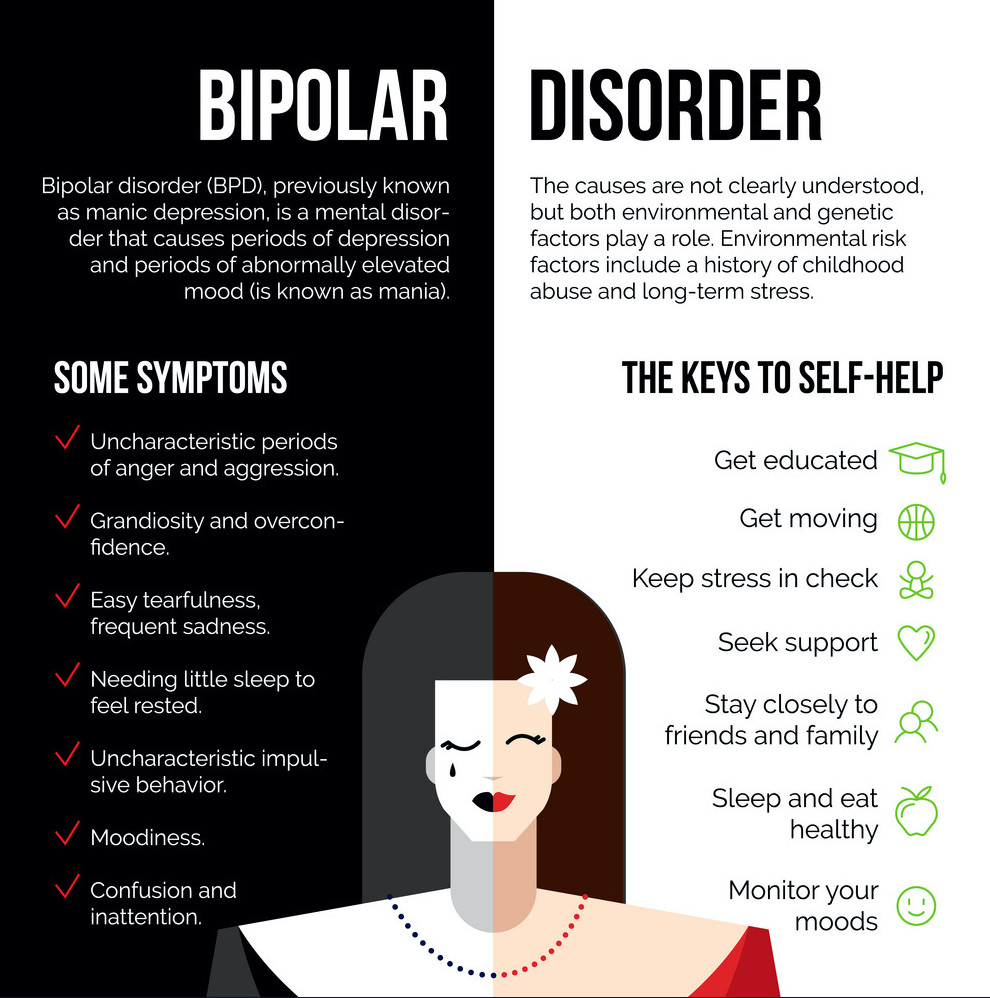
What to know about bipolar disorder?
A person with bipolar disorder will experience changes in mood, energy, and activity levels that can make day-to-day living difficult.
Bipolar disorder can cause severe disruption to a person’s life, but the impact varies between individuals. With appropriate treatment and support, many people with this condition live a full and productive life.
According to the National Alliance on Mental Illness (NAMI), bipolar disorder affects over 10 million people in the United States or around 2.8% of the population.
On average, a person will receive a diagnosis around the age of 25 years, but symptoms can appear during the teenage years or later in life. It affects males and females equally.
What is bipolar disorder?
The National Institute of Mental Health describe the main symptoms of bipolar disorder as alternating episodes of high and low mood. Changes in energy levels, sleep patterns, ability to focus, and other features can dramatically impact a person’s behavior, work, relationships, and other aspects of life.
Most people experience mood changes at some time, but those related to bipolar disorder are more intense than regular mood changes, and other symptoms can occur. Some people experience psychosis, which can include delusions, hallucinations, and paranoia.
Between episodes, the person’s mood may be stable for months or years, especially if they are following a treatment plan.
Treatment enables many people with bipolar disorder to work, study, and live a full and productive life. However, when treatment helps a person feel better, they may stop taking their medication. Then, the symptoms can return.
Some aspects of bipolar disorder can make a person feel good. During an elevated mood, they may find they are more sociable, talkative, and creative.
However, an elevated mood is unlikely to persist. Even if it does, it may be hard to sustain attention or follow through with plans. This can make it difficult to follow a project through to the end.
Symptoms
According to the International Bipolar Association, symptoms vary between individuals. For some people, an episode can last for several months or years. Others may experience “highs” and “lows” at the same time or in quick succession.
In “rapid cycling” bipolar disorder, the person will have four or more episodes within a year.
Mania or hypomania
Hypomania and mania are elevated moods. Mania is more intense than hypomania.
Symptoms can include:
- impaired judgment
- feeing wired
- sleeping little but not feeling tired
- a sense of distraction or boredom
- missing work or school
- underperforming at work or school
- feeling able to do anything
- being sociable and forthcoming, sometimes aggressively so
- engaging in risky behavior
- increased libido
- feeling exhilarated or euphoric
- having high levels of self-confidence, self-esteem, and self-importance
- talking a lot and rapidly
- jumping from one topic to another in conversation
- having “racing” thoughts that come and go quickly, and bizarre ideas that the person may act upon
- denying or not realizing that anything is wrong
Some people with bipolar disorder may spend a lot of money, use recreational drugs, consume alcohol, and participate in dangerous and inappropriate activities.
Depressive symptoms
During an episode of bipolar depression, a person may experience:
- a feeling of gloom, despair, and hopelessness
- extreme sadness
- insomnia and sleeping problems
- anxiety about minor issues
- pain or physical problems that do not respond to treatment
- a sense of guilt, which may be misplaced
- eating more or eating less
- weight loss or weight gain
- extreme tiredness, fatigue, and listlessness
- an inability to enjoy activities or interests that usually give pleasure
- difficulty focusing and remembering
- irritability
- sensitivity to noises, smells, and other things that others may not notice
- an inability to face going to work or school, possibly leading to underperformance
In severe cases, the individual may think about ending their life, and they may act on those thoughts.
Psychosis
If a “high” or “low” episode is very intense, the person may experience psychosis. They may have trouble differentiating between fantasy and reality.
According to the International Bipolar Foundation, psychosis symptoms during a high include hallucinations, which involve hearing or seeing things that are not there and delusions, which are false but strongly felt beliefs. A person who experiences delusions may believe they are famous, have high-ranking social connections, or have special powers.
During a depressive or “low” episode, they may believe they have committed a crime or are ruined and penniless.
It is possible to manage all these symptoms with appropriate treatment.
Types of bipolar disorder
A person may receive a diagnosis of one of three broad types of bipolar disorder. According to NAMI, symptoms occur on a spectrum, and the distinction between the types is not always clear-cut.
Bipolar I disorder
For a diagnosis of bipolar I disorder:
- The individual must have experienced at least one manic episode.
- The person may have had a previous major depressive episode.
- The doctor must rule out other disorders, such as schizophrenia and delusional disorder.
Bipolar II disorder
Bipolar II disorder involves periods of hypomania, but depression is often the dominant state.
For a diagnosis of bipolar II disorder, a person must have had:
- one or more episodes of depression
- at least one hypomanic episode
- no other diagnosis to explain the mood shifts
A person with hypomania may feel good and function well, but their mood will not be stable, and there is a risk that depression will follow.
People sometimes think of bipolar II disorder as a milder version. For many, however, it is simply different. As NAMI indicate, people with bipolar II disorder may experience more frequent episodes of depression than people with bipolar I disorder.
Cyclothymia
The National Health Service (NHS) in the United Kingdom note that cyclothymia has similar features to bipolar disorder, but the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) classifies it separately. It involves hypomania and depression, but the changes are less intense.
Nevertheless, cyclothymia can impact a person’s daily life, and a doctor can provide treatment.
Diagnosis
A medical professional will diagnose bipolar disorder using criteria set out in the DSM-5.
The National Institue of Mental Health (NIMH) explain that in order to receive a diagnosis of bipolar I disorder, a person must have had symptoms for at least 7 days, or less if symptoms were severe enough to need hospitalization. They may also have had a depressive episode lasting at least 2 weeks.
To receive a diagnosis of bipolar II, a person will have experienced at least one cycle of hypomania and depression.
A doctor may carry out a physical examination and some diagnostic tests, including blood and urine tests, to help rule out other causes.
It can be challenging for a doctor to diagnose bipolar disorder, as people are more likely to seek help with a low mood than a high mood. As a result, it can be hard for them to distinguish it from depression.
If the person has psychosis, a doctor may misdiagnose their condition as schizophrenia.
Other complications that may occur with bipolar disorder are:
- use of drugs or alcohol to cope with symptoms
- post-traumatic stress disorder (PTSD)
- anxiety disorder
- attention-deficit hyperactivity disorder (ADHD)
NIMH urge healthcare providers to look for signs of mania in the person’s history, to prevent misdiagnosis. Some antidepressants can trigger mania in susceptible people.
A person who receives a diagnosis of bipolar disorder has a lifelong diagnosis. They may enjoy long periods of stability, but they will always live with the condition.
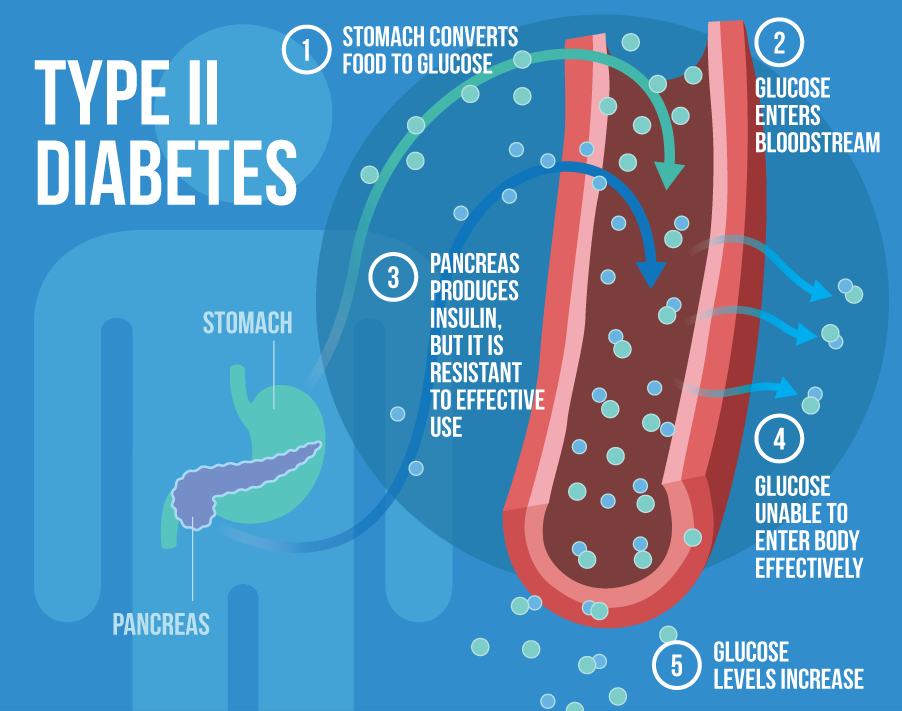
What are the symptoms of type 2 diabetes?
Type 2 diabetes is the most common form of diabetes. It happens when blood sugar levels rise due to problems with the use or production of insulin.
It can appear at any age, but it is more likely to occur after the age of 45 years.
It affects over 30 million Americans, according to the United States Centers for Disease Control and Prevention (CDC), and it accounts for 90–95 percent of diabetes cases.
What is type 2 diabetes?
People with type 2 diabetes do not make or use insulin correctly.
Insulin is a hormone that regulates the movement of blood glucose, or sugar, into cells, which use it as energy.
When sugar cannot enter cells, this means:
- too much glucose collects in the blood
- the body’s cells cannot use it for energy
A doctor may diagnose diabetes if a person’s blood sugar levels are 126 milligrams per deciliter (mg/dl) or above after fasting for 8 hours.
Symptoms
The symptoms of high blood sugar in type 2 diabetes tend to appear gradually. Not everyone with type 2 diabetes will notice symptoms in the early stages.
If a person does experience symptoms, they may notice the following:
- Frequent urination and increased thirst: When excess glucose builds up in the bloodstream, the body will extract fluid from tissues. This can lead to excessive thirst and the need to drink and urinate more.
- Increased hunger: In type 2 diabetes, the cells are not able to access glucose for energy. The muscles and organs will be low on energy, and the person may feel more hungry than usual.
- Weight loss: When there is too little insulin, the body may start burning fat and muscle for energy. This causes weight loss.
- Fatigue: When cells lack glucose, the body becomes tired. Fatigue can interfere with daily life when a person has type 2 diabetes.
- Blurred vision: High blood glucose can cause fluid to be pulled from the lenses of the eyes, resulting in swelling, leading to temporarily blurred vision.
- Infections and sores: It takes longer to recover from infections and sores because blood circulation is poor and there may be other nutritional deficits.
If people notice these symptoms, they should see a doctor. Diabetes can lead to a number of serious complications. The sooner a person starts to manage their glucose levels, the better chance they have of preventing complications.
Symptoms in children and teens
Type 2 diabetes is more likely to appear after the age of 45 years, but it can affect children and teens who:
- have excess weight
- do not do much physical activity
- have high blood pressure
- have a family history of type 2 diabetes
- have an African American, Asian American, Hispanic American, or American Indian background
The following symptoms may occur:
- weight loss, despite increased appetite and hunger
- extreme thirst and dry mouth
- frequent urination and urinary tract infections
- fatigue
- blurred vision
- slow healing of cuts or wounds
- numbness or tingling in hands and feet
- itchy skin
If caregivers notice these symptoms, they should take the child to see a doctor. These are also symptoms of type 1 diabetes. Type 1 is less common but more likely to affect children and teenagers than adults. However, type 2 diabetes is becoming more common in young people than it was in the past.
Symptoms in older adults
At least 25.2 percent of people aged 65 and above have type 2 diabetes in the United States. They may have some or all the classic symptoms of type 2 diabetes.
They may also experience one or more of the following:
- flu-like fatigue, which includes feeling lethargic and chronically weak
- urinary tract infections
- numbness and tingling in the hands, arms, legs, and feet due to circulation and nerve damage
- dental problems, including infections of the mouth and red, inflamed gums
Early signs
Most people do not experience symptoms in the early stages, and they may not have symptoms for many years.
A possible early sign of type 2 diabetes is darkened skin on certain areas of the body, including:
- the neck
- the elbows
- the knees
- the knuckles
This is known as acanthosis nigricans.
Other early symptoms include:
- frequent bladder, kidney, or skin infections
- cuts that take longer to heal
- fatigue
- extreme hunger
- increased thirst
- urinary frequency
- blurred vision
A person may have mild or subtle symptoms for many years, but these can become in time. Further health problems can develop.
Prediabetes and diabetes prevention
A person with blood sugar levels of 100–125 mg/dl will receive a diagnosis of prediabetes. This means that their blood sugar levels are high, but they do not have diabetes. Taking action at this stage can prevent diabetes from developing.
According to a 2016 report published in The Journal of the American Board of Family Medicine, 33.6 percent of people aged 45 years and older had prediabetes in 2012.
The CDC estimate that around 84 million American adults have prediabetes, but most do not know they have it.
Complications
Diabetes may cause a number of health complications if people do not manage it properly. Many of these are chronic, or long-term, but they can become life-threatening. Others need immediate medical attention as soon as they appear.
Emergency complications
Complications can arise quickly if blood sugar rises or falls too far.
Hypoglycemia
If blood glucose dips below 70 mg/dl, this is hypoglycemia, or low blood sugar.
This can happen if a person who uses insulin takes more than they need for a particular time.
A home blood glucose test can check for hypoglycemia.
It is vital to know the early signs of hypoglycemia, as it can progress quickly, resulting in seizures and a coma. In the early stages, however, it is easy to treat.
Symptoms of hypoglycemia include:
- confusion
- dizziness
- feeling faint
- heart palpitations
- rapid heartbeat
- mood changes
- loss of consciousness
- sweating
- clamminess
If symptoms are mild, a person can often resolve low blood sugar levels by consuming:
- a few pieces of hard candy
- a cup of orange juice
- a teaspoon of honey
- a glucose tablet
The person should then wait 15 minutes, test their blood sugar, and if it is still low, they should take another glucose tablet or sweet.
When levels return to above 70 mg/dl, the person should eat a meal, to stabilize their glucose levels.
If they remain low for 1 hour or longer, or if symptoms worsen, someone should take the person to the emergency room.
Anyone who has frequent or severe hypoglycemic episodes should speak to their doctor, as they may need to adjust their treatment plan.
Hyperglycemia and diabetic ketoacidosis (DKA)
If blood sugar levels rise too far, hyperglycemia can result. If a person notices increased thirst and urination, they should check their blood sugar levels.
It the level is above the target level that their doctor recomends, they take appropriate action.
Without treatment, high a person with hyperglycemia can develop diabetic ketoacidosis (DKA), which happens when high levels of ketones collect in the blood, making it too acidic. For this reason, the person should also test their ketone levels.
Ketoacidosis can lead to:
- difficulty breathing
- a fruity smell on the breath
- a dry mouth
- nausea and vomiting
- coma
It can be life-threatening. A person with these signs and symptoms should seek immediate medical attention.
People who regularly experience high blood sugar should speak to their doctor about adjusting their treatment plan.
People should check with their doctor how often they need to test.
Long-term complications
Keeping blood glucose within target levels can prevent complications that can become life-threatening and disabling over time.
Some possible complications of diabetes are:
- heart and blood vessel diseases
- high blood pressure
- nerve damage (neuropathy)
- foot damage
- eye damage and blindness
- kidney disease
- hearing problems
- skin problems
Effective management of blood glucose levels can reduce the risk of complications.
Diagnosis and treatment
A doctor can diagnose type 2 diabetes with blood tests that measure blood glucose levels. Many people discover they have high blood sugar during a routine screening test, but anyone who experiences symptoms should see a doctor.
Treatment aims to keep blood glucose levels stable at a healthy level and prevent complications. The main ways to do this are through lifestyle measures.
These include:
- following a healthful diet
- reaching and maintaining a healthy weight and body mass index (BMI)
- doing physical activity
- getting enough sleep
- avoiding or quitting smoking
- taking medications or insulin as the doctor recommends
Outlook
There is currently no cure for diabetes, but most people with the condition can lead a healthful life by managing their condition properly.
People who maintain a healthy weight, follow a healthful diet, and do regular exercise may not need medication. Taking these steps can help manage blood sugar levels.
Routine screening can alert a person to high blood sugar levels in the early stages, when there is still time to slow, stop, or reverse the progress of diabetes.
Current guidelines recommend regular screening from the age of 45 years, or younger if an individual has other risk factors, such as obesity. A doctor can advise on individual needs.
It is important to have support from people who understand what it is like to receive a diagnosis and live with type 2 diabetes.
What is shingles?
Shingles is a viral infection that results from the varicella-zoster virus (VZV), the same virus that causes chickenpox. It typically affects a single sensory nerve ganglion and the skin surface that the nerve supplies.
Anyone who has had chickenpox can later develop shingles.
In fact, according to the Centers for Disease Control and Prevention (CDC), an estimated 1 in 3 people in the United States develop shingles during their lifetime.
However, a person can only develop shingles if they have had chickenpox or exposure to the virus that causes it. This virus can lie dormant for years.
Most adults with the dormant virus never develop shingles, but for some, the virus reactivates several times.
Shingles is most common after the age of 50 years, but it can appear at any age if a person has previously had chickenpox.
In this article, learn more about shingles, including symptoms, complications, and treatments.
Symptoms
Shingles usually affects one side of the body. This is most often the waist, chest, abdomen, or back. Symptoms can also appear on the face and in the eyes, mouth, ears. The virus can also affect some internal organs.
Shingles typically affects a single sensory nerve ganglion near the spinal cord, called a dorsal root ganglion. This is why the symptoms occur in specific areas of the body, rather than all over it. The pain results from nerve involvement, rather than the rash itself.
In fact, some people have pain but no rash. Others, meanwhile, may have a rash with pain that is accompanied by other symptoms, such as fever, chills, or headache.
Symptoms can vary in nature, depending on where on the body they appear.
Common symptoms
Some of the most common symptoms of shingles include:
- a constant dull, burning, or gnawing pain, or a sharp, stabbing pain that comes and goes
- a skin rash that resembles a chickenpox rash but only affects certain areas
- fluid-filled blisters that develop as part of the rash
Symptoms on the body
A blistering skin rash may appear in one or more distinct bands with sensory nerves of the skin, called dermatomes.
Common locations for this include:
- the chest
- the abdomen
- the back
- around the waist
It usually occurs only on one side of the body.
The location of the symptoms will depend on which dermatome distribution the virus affects.
Facial symptoms
If the rash affects the face, symptoms usually appear on one side only — usually around one eye and the forehead.
They can include:
- pain over the affected dermatome
- a rash
- muscle weakness
- headache
Eye symptoms
If the virus affects an ophthalmic nerve, it means that a person has herpes zoster ophthalmicus.
This can cause pain, redness, and swelling in and around the eye, as well as temporary or permanent loss of vision.
Ear symptoms
Shingles can also occur in or around the ear, leading to problems with balance and hearing, as well as muscle weakness on the affected side of the face.
These changes can be long term or even permanent. A person who develops symptoms in or around the ears and eyes should seek immediate medical attention to reduce the risk of complications.
Mouth symptoms
If shingles affects the mouth, a person may experience:
- facial tenderness
- pain in the mouth
- toothache
- lesions in hard and soft palate tissues
The pain and discomfort of these symptoms can make it difficult to eat or drink.
Internal shingles
Shingles can also affect the internal organs. There will not be a rash, but other problems can arise.
For example, researchers have found evidence of shingles in the digestive system, which can lead to gastrointestinal dysfunction, and in the arteries in the brain, which may increase the risk of stroke and dementia.
Other symptoms
There may also be other symptoms, including:
- fever
- fatigue
- chills
- headache
- upset stomach
Symptom progression
Symptoms typically progress as follows:
- Pain, tingling, numbness, and itching start to affect a specific part of the skin.
- After up to 2 weeks, a rash appears.
- Red blotches and itchy, fluid-filled blisters develop and continue to do so for 3-5 days.
- The blisters may merge, forming a solid red band that looks similar to a severe burn. The gentlest touch may be painful.
- Inflammation may affect the soft tissue under and around the rash.
- After 7–10 days, the blisters gradually dry up and form scabs or crusts. As the blisters disappear, they may leave minor scarring.
Shingles usually lasts around 2–4 weeks. It is contagious until the blisters dry up and crust over.
Most people will only have an episode of shingles once, but it can recur in some people.
Complications
Rarely, complications can arise — especially in people with an impaired immune system.
Possible complications of shingles include:
- postherpetic neuralgia (PHN)
- inflammation of the brain or spinal cord, increasing the risk of stroke, encephalitis, and meningitis
- eye and vision problems
- weakness
- problems with balance and hearing
- damage to blood vessels, which could lead to stroke
- pneumonia
According to the CDC, around 10–18% of people who have shingles will develop PHN, a long term complication wherein the pain of a shingles rash lasts long beyond the rash itself.
It is more likely to occur if a person develops shingles after the age of 40 years, and the risk continues to increase with age.
In people with weak immune systems
People with a weakened immune system will have a higher risk of developing shingles and of experiencing severe symptoms and complications.
This include people who:
- have cancer, especially leukemia or lymphoma
- have HIV
- have undergone an organ transplant
- are taking medications to suppress the immune system, including chemotherapy drugs
These people should seek medical attention as soon as possible if they have concerns about shingles-related symptoms.
Is shingles contagious?
It is not possible to directly transmit shingles to another person. However, a person who has never had chickenpox can contract VZV by coming into direct contact with the fluid in the blisters of a person who currently has shingles.
If this happens and the person has not received vaccination against chickenpox, they would develop chickenpox first, not shingles.
Shingles does not spread through coughing or sneezing. Only direct contact with fluid from the blisters can spread the virus. Therefore, covering the blisters reduces the risk of contagion.
It is important to note that the virus is only active from when the blisters first appear to when they dry up and crust over. Transmission is not possible before the blisters develop and after the crusts form. If a person does not develop blisters, the virus cannot spread in the traditional sense.
Taking the following precautions can help prevent the transmission of the virus:
- Cover the rash.
- Wash the hands often.
- Avoid touching or scratching the rash.
It is also important to avoid contact with:
- infants who are preterm or have a low birth weight
- pregnant women who have never had chickenpox or the vaccine for it
- those with a weakened immune system
Treatment
A doctor may prescribe antiviral drugs to stop the virus from multiplying.
Antiviral treatment
Antiviral treatment can help:
- reduce the severity and duration of symptoms
- prevent complications from developing
- lower the risk of the rash coming back
Managing symptoms
Tips for managing symptoms include:
- using pain relief medication
- reducing stress as much as possible
- eating regular, nutritious meals
- getting some gentle exercise
- wearing loose fitting clothes, for comfort
To relieve itching, the CDC recommend:
- applying calamine lotion
- taking a lukewarm, oatmeal bath
- placing a cool, damp washcloth on the blisters
Most people will recover with home treatment, but a person should seek medical help if other symptoms appear, such as a fever. Around 1–4% of people will need to spend time in the hospital due to complications.

Abortion
Abortion, sometimes known as a ‘termination of pregnancy,’ is the medical process of ending a pregnancy to ensure that it does not end in the birth of a baby. Women have abortions for many reasons, including personal circumstances, a risk to the mother or a high chance that the baby will have a serious genetic or physical abnormality.
There are a number of types of abortion, and options depend on the duration of the pregnancy. An abortion is a medical means of ending a pregnancy.
Worldwide, around half of all reported unintended pregnancies end in abortion. Abortion is legal throughout the majority of the United States and in many other countries.
When can a woman have an abortion?
Where abortion is legal in the U.S., doctors usually perform them in the first trimester or the early part of the second trimester.
The first trimester lasts from conception to week 12 of pregnancy. The second trimester is from week 13 to week 28. Some states allow abortion in the latter part of the second trimester. In 2015, two-thirds (65.4%) of reported abortions in the country took place when the pregnancy had lasted fewer than 8 weeks.
In the first trimester, options for abortion commonly include:
- medical abortion
- vacuum aspiration
A woman can usually access medical abortion until about 10 weeks after her last period. It involves taking two types of medication.
Surgical options, such as vacuum aspiration and dilation and evacuation, are more common after 10 weeks.
In the second trimester, a woman may undergo:
- dilation and evacuation
- labor induction abortion
Abortion is rare during the third trimester, but a doctor may perform it after 29 weeks of pregnancy if a woman’s life is in danger. They may use the same methods that are used during the second trimester.
Medical abortion
A medical abortion requires a woman to take pills at separate times.This type of abortion involves taking two medications, mifepristone and misoprostol.
A doctor or nurse will advise about the timing, but a woman should take the second medication, misoprostol, no more than 48 hours after taking the first, mifepristone.
Mifepristone stops the pregnancy from developing. Misoprostol triggers the uterus to empty, which will begin 1–4 hours after taking the pill.
A woman will experience cramping and bleeding as the uterus empties, which may feel like having an unusually heavy period. Some women feel more severe cramping than others.
Within around 4–5 hours, the pregnancy tissue will likely have passed from the body, but it can take longer.
Advantages
Some advantages of a medical abortion are:
- It does not involve surgery.
- It is available in the first trimester.
- It does not require an anesthetic.
Disadvantages
Some disadvantages of a medical abortion are:
- It is not available in the second trimester.
- Only part of the treatment takes place in a clinic.
- It may cause painful cramping.
- Rarely, it is not effective.
It may be a good idea to have a partner or friend close by for support while the tissue is passing.
Recovery
Recovery from a medical abortion involves:
- some bleeding and spotting that may last for several weeks
- a check-up with the doctor to monitor recovery
Risks
Some women experience side effects of the medications. These can include:
- nausea
- heavy vaginal bleeding
- dizziness
- fatigue
- diarrhea
- mild fever
Vacuum aspiration
Vacuum aspiration is a type of surgical abortion that involves using gentle suction to end a pregnancy. Doctors typically recommend this during the first trimester.
How it works
A doctor begins the vacuum aspiration procedure by inserting a speculum into the woman’s vagina. They then apply medication or use an injection to numb the area.
Next, they use thin rods called dilators to open the cervix, then insert a tube into the uterus. Then, they use either a manual or mechanic suction device to empty the uterus.
Advantages
The advantages of vacuum aspiration are:
- It is available in the first 12 weeks of pregnancy.
- It is quick, with the procedure only taking 5–10 minutes.
- It is relatively pain-free, though some women experience cramping, sweating, nausea, or a combination.
- It does not require a general anesthetic.
Disadvantages
The main disadvantage of vacuum aspiration is that it is not available in the second trimester.
Recovery
Recovery from vacuum aspiration involves:
- resting for up to 1 hour after treatment
- taking antibiotics to prevent infection
- avoiding sex for 1 week after treatment
Also, some women experience cramping for a few days following the procedure, and irregular bleeding or spotting can occur for several weeks.
Risks
The potential complications of vacuum aspiration include bleeding and infection. However, the risk of these complications is low.
Speak to the doctor right away if signs of bleeding or new symptoms occur.
Dilation and evacuation
Dilation and evacuation is a type of surgical abortion that doctors commonly use during the second trimester.
How it works
A doctor may give a general anesthetic before performing a dilation and evacuation. This type of anesthetic ensures that a person does not feel anything during the procedure.
The doctor begins by inserting a speculum into the woman’s vagina. Then, they use dilators to open the cervix.
Next, they remove the pregnancy tissue with small forceps. Finally, they use suction to remove any remaining tissue.
Advantages
The advantages of dilation and evacuation are:
- It is available in the second trimester.
- It is a safe and effective way to end a pregnancy.
Disadvantages
The disadvantage of dilation and evacuation is that it can require a general anesthetic.
Recovery
Recovery from dilation and evacuation involves resting.
Mild pain and cramping can occur for a few days after the procedure, and there may be some bleeding for up to 2 weeks.
Risks
Potential complications of dilation and evacuation include:
- infection
- heavy bleeding
- injury to the uterus
The risk of injury to the uterus or other organs during a second-trimester abortion is less than 1 in 1,000, according to The American College of Obstetricians and Gynecologists.
Labor induction abortion
Labor induction abortion is a late-term method of ending a pregnancy in the second or third trimester.
This type of abortion is rare, and a doctor may recommend it if a woman’s life is in danger.
How it works
Labor induction involves using medications to start labor, which causes the uterus to empty over a period of around 12–24 hours. A woman can take these medications by mouth or the doctor may place them into the vagina or inject them into the uterus.
Doctors usually also administer pain relief medication or a local anesthetic, as intense cramping occurs during this type of abortion.
Recovery
After the abortion is complete, a woman tends to remain in the clinic or hospital for anywhere from a few hours to 1–2 days, depending on health and other factors.
The doctor can help determine the length of the stay, and they may be able to estimate it before the abortion.
Risks
The medications that induce labor can cause side effects, such as:
- nausea and vomiting
- fever
- diarrhea
Complications are rare but can include:
- hemorrhage
- cervical injury
- infection
- rupture of the uterus
- incomplete release of the pregnancy tissue
What to know about breast cancer
Breast cancer is the most common invasive cancer in women and the second leading cause of cancer death in women after lung cancer.
Advances in screening and treatment for breast cancer have improved survival rates dramatically since 1989. According to the American Cancer Society (ACS), there are more than 3.1 million breast cancer survivors in the United States. The chance of any woman dying from breast cancer is around 1 in 38 (2.6%).
Awareness of the symptoms and the need for screening are important ways of reducing the risk. In rare instances, breast cancer can also affect men, but this article will focus on breast cancer in women.
Symptoms
The first symptoms of breast cancer usually appear as an area of thickened tissue in the breast or a lump in the breast or an armpit.
Other symptoms include:
- pain in the armpits or breast that does not change with the monthly cycle
- pitting or redness of the skin of the breast, similar to the surface of an orange
- a rash around or on one of the nipples
- discharge from a nipple, possibly containing blood
- a sunken or inverted nipple
- a change in the size or shape of the breast
- peeling, flaking, or scaling of the skin on the breast or nipple
Most breast lumps are not cancerous. However, women should visit a doctor for an examination if they notice a lump on the breast.
Stages
A doctor stages cancer according to the size of the tumor and whether it has spread to lymph nodes or other parts of the body.
There are different ways of staging breast cancer. One way is from stage 0–4, with subdivided categories at each numbered stage. Descriptions of the four main stages are listed below, though the specific substage of a cancer may also depend on other specific characteristics of the tumor, such as HER2 receptor status.
- Stage 0: Known as ductal carcinoma in situ (DCIS), the cells are limited to within the ducts and have not invaded surrounding tissues.
- Stage 1: At this stage, the tumor measures up to 2 centimeters (cm) across. It has not affected any lymph nodes, or there are small groups of cancer cells in the lymph nodes.
- Stage 2: The tumor is 2 cm across, and it has started to spread to nearby nodes, or is 2–5 cm across and has not spread to the lymph nodes.
- Stage 3: The tumor is up to 5 cm across, and it has spread to several lymph nodes or the tumor is larger than 5 cm and has spread to a few lymph nodes.
- Stage 4: The cancer has spread to distant organs, most often the bones, liver, brain, or lungs.
Causes
After puberty, a woman’s breast consists of fat, connective tissue, and thousands of lobules. These are tiny glands that produce milk for breastfeeding. Tiny tubes, or ducts, carry the milk toward the nipple.
Cancer causes the cells to multiply uncontrollably. They do not die at the usual point in their life cycle. This excessive cell growth causes cancer because the tumor uses nutrients and energy and deprives the cells around it.
Breast cancer usually starts in the inner lining of milk ducts or the lobules that supply them with milk. From there, it can spread to other parts of the body.
Risk factors
The exact cause of breast cancer remains unclear, but some risk factors make it more likely. It is possible to prevent some of these risk factors.
1. Age
The risk of breast cancer increases with age. At 20 years, the chance of developing breast cancer in the next decade is 0.06%. By the age of 70 years, this figure goes up to 3.84%.
2. Genetics
Women who carry certain mutations in the BRCA1 and BRCA2 genes have a higher chance of developing breast cancer, ovarian cancer, or both. People inherit these genes from their parents.
Mutations in the TP53 gene also have links to increased breast cancer risk.
If a close relative has or has had breast cancer, a person’s chance of developing breast cancer increases.
Current guidelines recommend that people in the following groups seek genetic testing:
- those with a family history of breast, ovarian, fallopian tube, or peritoneal cancer
- those in whose ancestry there is a history of breast cancer related to BRCA1 or BRCA2 gene mutations, for example, people with Ashkenazi Jewish ancestry
3. A history of breast cancer or breast lumps
Women who have previously had breast cancer are more likely to have it again than those who have no history of the disease.
Having some types of noncancerous breast lump increases the chance of developing cancer later on. Examples include atypical ductal hyperplasia or lobular carcinoma in situ.
Individuals with a history of breast, ovarian, fallopian tube, or peritoneal cancer should ask their doctors about genetic testing.
4. Dense breast tissue
Women with more dense breasts are more likely to receive a diagnosis of breast cancer.
5. Estrogen exposure and breastfeeding
Extended exposure to estrogen appears to increase the risk of breast cancer.
This could be due to a person starting their periods earlier or entering menopause at a later than average age. Between these times, estrogen levels are higher.
Breastfeeding, especially for over 1 year, appears to reduce the chance of developing breast cancer. This is possibly due to the drop in estrogen exposure that follows pregnancy and breastfeeding.
6. Body weight
Women who become overweight or develop obesity after menopause may also have a higher chance of developing breast cancer, possibly due to increased estrogen levels. High sugar intake may also be a factor.
7. Alcohol consumption
A higher rate of regular alcohol consumption appears to play a role in breast cancer development.
According to the National Cancer Institute (NCI), studies have consistently found that women who consume alcohol have a higher risk of breast cancer than those who do not. Those who drink moderate to heavy levels of alcohol have a higher risk than light drinkers.
8. Radiation exposure
Undergoing radiation treatment for a different cancer may increase the risk of developing breast cancer later in life.
9. Hormone treatments
According to the NCI, studies have shown that oral contraceptives may slightly increase the risk of breast cancer
According to the ACS, studies have found that hormone replacement therapy (HRT), specifically estrogen-progesterone therapy (EPT), is related to an increased risk of breast cancer.
Cosmetic implants and breast cancer survival
A 2013 review found that women with cosmetic breast implants who received a diagnosis of breast cancer also had a higher risk of dying from the disease.
This could be due to the implants masking cancer during screening or because the implants bring about changes in breast tissue.
However, a 2015 review published in Aesthetic Surgery Journal found that having cosmetic breast implant surgery did not increase the risk of breast cancer.
Scientists need to carry out more research to confirm the link.
Types
There are several different types of breast cancer, including:
- Ductal carcinoma: This begins in the milk duct and is the most common type.
- Lobular carcinoma: This starts in the lobules.
Invasive breast cancer occurs when the cancer cells break out from inside the lobules or ducts and invade nearby tissue. This increases the chance of cancer spreading to other parts of the body.
Noninvasive breast cancer develops when the cancer remains inside its place of origin and has not yet spread. However, these cells can sometimes progress to invasive breast cancer.
Diagnosis
A doctor often diagnoses breast cancer as the result of routine screening or when a woman approaches her doctor after detecting symptoms.
Several diagnostic tests and procedures help to confirm a diagnosis.
Breast exam
The doctor will check the breasts for lumps and other symptoms.
During the examination, the person may need to sit or stand with their arms in different positions, such as above their head or by their sides.
Imaging tests
Several tests can help detect breast cancer.
Mammogram: This is a type of X-ray that doctors commonly use during an initial breast cancer screening. It produces images that can help a doctor detect any lumps or abnormalities.
A doctor will usually follow any suspicious results with further testing. However, mammography sometimes shows a suspicious area that turns out not to be cancer.
Ultrasound: This scan uses sound waves to help a doctor differentiate between a solid mass and a fluid-filled cyst.
MRI: Magnetic Resonance Imaging (MRI) combines different images of the breast to help a doctor identify cancer or other abnormalities. A doctor may recommend an MRI as a follow-up to a mammogram or ultrasound. Doctors sometimes use them as a screening tool for those at higher risk of breast cancer.
Biopsy
In a biopsy, the doctor extracts a sample of tissue and sends it for laboratory analysis.
This shows whether the cells are cancerous. If they are, a biopsy indicates which type of cancer has developed, including whether or not the cancer is hormone sensitive.
Diagnosis also involves staging the cancer to establish:
- the size of a tumor
- how far it has spread
- whether it is invasive or noninvasive
Staging provides a picture of a person’s chances of recovery and their ideal course of treatment.
Treatment
Treatment will depend on several factors, including:
- the type and stage of the cancer
- the person’s sensitivity to hormones
- the age, overall health, and preferences of the individual
The main treatment options include:
radiation therapy
- surgery
- biological therapy, or targeted drug therapy
- hormone therapy
- chemotherapy
Factors affecting the type of treatment a person has will include the stage of the cancer, other medical conditions, and their individual preference.
Surgery
If surgery is necessary, the type will depend on both the diagnosis and individual preference. Types of surgery include:
Lumpectomy: This involves removing the tumor and a small amount of healthy tissue around it.
A lumpectomy can help prevent the spread of the cancer. This may be an option if the tumor is small and easy to separate from its surrounding tissue.
Mastectomy: A simple mastectomy involves removing the lobules, ducts, fatty tissue, nipple, areola, and some skin. In some types, a surgeon will also remove the lymph nodes and muscle in the chest wall.
Sentinel node biopsy: If breast cancer reaches the sentinel lymph nodes, which are the first nodes to which a cancer can spread, it can spread into other parts of the body through the lymphatic system. If the doctor does not find cancer in the sentinel nodes, then it is usually not necessary to remove the remaining nodes.
Axillary lymph node dissection: If a doctor finds cancer cells in the sentinel nodes, they may recommend removing several lymph nodes in the armpit. This can prevent the cancer from spreading.
Reconstruction: Following mastectomy, a surgeon can reconstruct the breast to look more natural. This can help a person cope with the psychological effects of breast removal.
The surgeon can reconstruct the breast at the same time as performing a mastectomy or at a later date. They may use a breast implant or tissue from another part of the body.
Radiation therapy
A person may undergo radiation therapy around a month after surgery. Radiation involves targeting the tumor with controlled doses of radiation that kill any remaining cancer cells.
Chemotherapy
A doctor may prescribe cytotoxic chemotherapy drugs to kill cancer cells if there is a high risk of recurrence or spread. When a person has chemotherapy after surgery, doctors call it adjuvant chemotherapy.
Sometimes, a doctor may choose to administer chemotherapy before surgery to shrink the tumor and make its removal easier. Doctors call this neoadjuvant chemotherapy.
Hormone blocking therapy
Doctors use hormone blocking therapy to prevent hormone sensitive breast cancers from returning after treatment. Hormone therapy may be used to treat estrogen receptor (ER)-positive and progesterone receptor (PR)-positive cancers.
They usually administer hormone blocking therapy after surgery but might sometimes use it beforehand to shrink the tumor.
Hormone blocking therapy may be the only option for people who are not suitable candidates for surgery, chemotherapy, or radiotherapy.
Doctors may recommend a person has hormone therapy for 5–10 years after surgery. However, the treatment will not affect cancers that are not sensitive to hormones.
Examples of hormone blocking therapy medications may include:
- tamoxifen
- aromatase inhibitors
- ovarian ablation or suppression
- Goserelin, which is a luteinizing hormone-releasing agonist drug that suppresses the ovaries
Hormone treatment may affect fertility.
Biological treatment
Targeted drugs can destroy specific types of breast cancer. Examples include:
- trastuzumab (Herceptin)
- lapatinib (Tykerb)
- bevacizumab (Avastin)
Treatments for breast and other cancers can have severe adverse effects. When deciding on a treatment, people should discuss the potential risks with a doctor and look at ways to minimize the side effects.
Outlook
A person’s outlook with breast cancer depends on the staging. Early detection and treatment usually lead to a positive outlook.
According to the ACS, a person who receives treatment for stage 0 or stage 1 breast cancer has a 99% chance of surviving for at least 5 years after being diagnosed, when compared to women who do not have cancer.
If breast cancer reaches stage 4, the chance of surviving another 5 years reduces to around 27%.
Regular checks and screening can help detect symptoms early. Women should discuss their options with a doctor.
Regular screening
There are several different guidelines for how often women should have breast cancer screening.
The American College of Physicians (ACP) recommend that women aged 40–49 years with an average risk of breast cancer should discuss the benefits and risks of regular screenings with a doctor.
Between 50 and 74 years of age, women who have an average risk should undertake screenings every 2 years. Beyond 75 years of age, doctors only recommend screenings for women with a life expectancy of 10 or more years.
The ACS suggest that women of average risk can choose to have yearly scans from the age of 40 years onward. Those who have not should start annual screening at 45 years of age. They may decide to switch to screenings every other year when they reach 55 years of age.
The American College of Radiologists recommend screenings every year, starting from 40 years of age.
Despite the different recommendations, most experts agree that women should talk to their doctors about breast cancer screening from 40 years of age onward.
Prevention
There is no way to prevent breast cancer. However, certain lifestyle decisions can significantly reduce the risk of breast cancer as well as other types.
These include:
- avoiding excessive alcohol consumption
- following a healthful diet containing plenty of fresh fruit and vegetables
- getting enough exercise
- maintaining a healthy body mass index (BMI)
Women should consider their options for breastfeeding and the use of HRT following menopause, as these can also increase the risk.
Preventive surgery is also an option for women at high risk of breast cancer.

