How and why does diet influence immune function?
We may take it for granted that our diet can influence the way our immune systems work. But how and why does what we eat impact the immune response? In this Honest Nutrition feature, we investigate.
that constantly works to protect the body from antigens, which have associations with pathogens, including bacteria, toxins, parasites, and viruses.
The immune system offers two lines of defense: innate immunity and adaptive immunity.
Innate immunity is the first line of defense and consists of physical barriers, such as the skin and mucous membranes and chemical and cellular defenses. The innate immune system is nonspecific
because it reacts the same way to all foreign invaders.
If the innate immune system is ineffective against a potential threat, the adaptive immune system takes over.
The adaptive immune system consists of specialized blood cells and proteins that target the specific cause of infection. The adaptive immune system has a “memory” which is why a person’s body becomes immune to specific illnesses after initial exposure.
A person’s immune system needs to function well for them to remain healthy. Certain illnesses, medications, and lifestyle choices, such as smoking and excessive drinking, can adversely affect immune function.
Research shows that a person’s diet can impact immune health as well.
Article highlights:
Can diet influence the immune system?
suggest that a person’s diet influences their immune system, like all other aspects of health.
For example, nutrition can affect the microbiome, gut barrier function, inflammatory processes, and white blood cell function, all of which impact immune function.
Dietary patterns and individual foods have associations with increased disease risk, greater risk of allergy, and impaired immune response.
Western-type diets tend to contain high levels of saturated fat, ultra-processed foods, added sugar and salt, and overall calories. This diet is often low in foods associated with better health, such as vegetables, fruits, and fatty fish, and has strong links to an increased risk of chronic disease.
Research suggests that Western-type diets induce inflammation and alter immune system function, promoting disease development.
In contrast, diets rich in whole foods, such as vegetables, fruits, nuts, legumes, and seafood, and low in ultra-processed foods can reduce disease risk and promote healthy immune function.
Additionally, a deficiency or insufficiency of nutrients essential to immune function, including vitamin D, zinc, and vitamin C, can also affect immune response.
Nutrient deficiencies may be more common in those consuming ultra-processed diets low in whole, nutrient-dense foods.
Although it is clear that dietary choices impact overall health, including immune function, the interaction between diet and immune health is highly complex. Scientists are still learning how the foods a person consumes may help or harm immune function.
Adverse effects of unhealthy diets
Western-type diets tend to be high in refined carbohydrates, added sugars, saturated fat, and calories. This pattern of eating affects immune function in several ways.
Most of the foods in Western diets are ultra-processed and contain high levels of added sugar, which can promote inflammatory responses of the immune system.
For example, foods and beverages that significantly impact blood sugar levels, such as soda, candy, sugary cereals, and sugary baked goods, increase levels of inflammatory proteins, including tumor necrosis-alpha (TNF-alpha), C-reactive protein (CRP), and interleukin-6 (IL-6). They also interfere with the function of protective immune cells, including neutrophils and phagocytes.
A 2012 study that included 562 adults aged 85 years and older without diabetes found that the participants who had higher blood sugar levels had lower innate immune responses. They also had higher levels of CRP, which is a marker of inflammation.
Higher blood sugar levels have links to an impaired immune response in people with diabetes as well.
Also, diets high in added sugar and refined carbs may adversely alter gut bacteria, leading to dysbiosis, which involves digestive disturbances, such as bloating.
A healthy microbiome is essential to immune function because gut bacteria play a critical role in the development and function of the immune system.
Experts have also linked Western-type diets to an altered immune response due to high levels of saturated fat and added salt.
Studies indicate that diets high in saturated fat may promote inflammation, modify gut bacteria, and inhibit the functioning of white blood cells.
Diets high in added salt have links to excessive immune response, impaired inflammation regulation in the body, and an increased risk of certain autoimmune diseases, such as rheumatoid arthritis.
Western-type diets have links to an increased risk of developing several chronic diseases, including certain cancers, heart disease, and type 2 diabetes.
Researchers attribute this to the chronic low-grade inflammation and altered immune response that Western-type diets, sedentary lifestyles, and toxin exposure cause.
However, research investigating the relationship between diet and immune function is ongoing, and scientists do not entirely understand this complex relationship.
Diets for healthy immune function
While a diet high in ultra-processed foods, added sugar, and excessive calories may lead to immune dysfunction, dietary patterns rich in whole, nutrient-dense foods are beneficial for immune function.
The Mediterranean diet is rich in vegetables, legumes, nuts, fruits, whole grains, olive oil, and other healthy foods. Research has shown that it can reduce disease risk, lower markers of inflammation, and beneficially modulate gut bacteria.
Diets high in fiber, such as the Mediterranean diet, promote the production of short-chain fatty acids (SCFAs), including acetate, propionate, and butyrate. SCFAs are end products of bacterial fermentation in the gut and have health benefits.
SCFAs act locally and systemically to modulate the immune response. They maintain the health of and improve the immune defensive function of the intestinal epithelium. This is an important part of the immune system that serves as a barrier against microorganisms. It also reduces the production of inflammatory proteins from immune cells.
Diets high in fruits, vegetables, olive oil, nuts, seeds, and fatty fish contain high levels of nutrients, such as vitamin A, vitamin C, zinc, vitamin D, B6, B12, copper, folate, iron, and selenium. The immune system needs these nutrients to function optimally.
Experts know that vegetarian-based diets reduce markers of chronic inflammation, such as CRP, fibrinogen, and IL-6. This might be partly due to the array of nutrients and nonnutritive components found in fruits and vegetables strengthening the immune system response.
Foods rich in healthy fats, fiber, vitamins, protein, minerals, and beneficial plant compounds help reduce systemic inflammation, promote healthy gut bacteria balance, reduce oxidative stress and cellular damage, and improve blood sugar and insulin sensitivity. All of these activities are essential for healthy immune function.
Additionally, studies show that supplementing the diet with nutrients including vitamin D, zinc, and vitamin C may help optimize immune function and reduce infection risk.
To support immune function, a person should concentrate on following a balanced dietary pattern rich in whole, nutrient-dense foods, especially plant foods, such as vegetables, fruits, legumes, nuts, and seeds. People should avoid or limit ultra-processed foods high in refined grains and added sugar.
The bottom line
It is essential to follow a healthy diet to ensure good immune function.
Studies show that while certain dietary patterns may lead to impaired immune function, other dietary patterns promote optimal immune function.
A dietary pattern low in ultra-processed foods and rich in whole, nutrient-dense foods, such as vegetables, fruits, fish, and legumes, protects against chronic disease risk and supports a healthy immune response.
Following a healthy dietary pattern and leading a lifestyle that includes stress reduction techniques, restful sleep, daily physical activity, and other healthy habits is the best way to support the immune system and reduce disease risk.

What are the symptoms of type 2 diabetes?
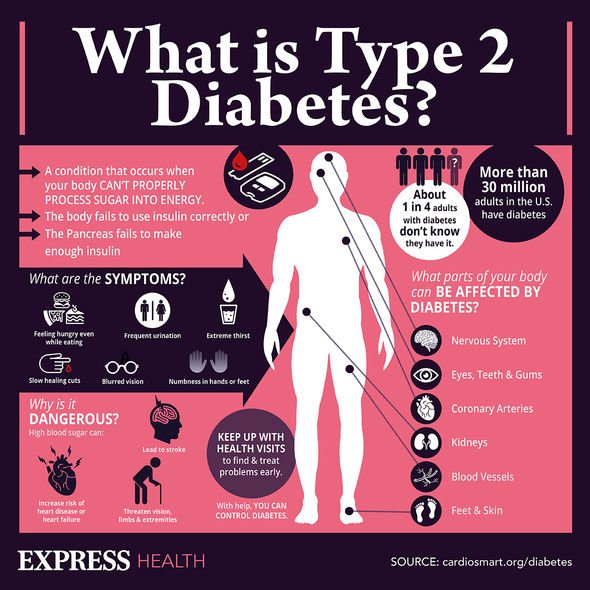
Type 2 diabetes is the most common form of diabetes. It happens when blood sugar levels rise due to problems with the use or production of insulin.
Americans, according to the United States Centers for Disease Control and Prevention (CDC), and it accounts for 90–95 percent of diabetes cases.
This article looks at the early signs and symptoms of type 2 diabetes, the risk factors, and potential complications.
What is type 2 diabetes?
People with type 2 diabetes do not make or use insulin correctly.
Insulin is a hormone that regulates the movement of blood glucose, or sugar, into cells, which use it as energy.
When sugar cannot enter cells, this means:
- too much glucose collects in the blood
- the body’s cells cannot use it for energy
A doctor may diagnose diabetes if a person’s blood sugar levels are 126 milligrams per deciliter (mg/dl) or above after fasting for 8 hours.
Symptoms
The symptoms of high blood sugar in type 2 diabetes tend to appear gradually. Not everyone with type 2 diabetes will notice symptoms in the early stages.
If a person does experience symptoms, they may notice the following:
- Frequent urination and increased thirst: When excess glucose builds up in the bloodstream, the body will extract fluid from tissues. This can lead to excessive thirst and the need to drink and urinate more.
- Increased hunger: In type 2 diabetes, the cells are not able to access glucose for energy. The muscles and organs will be low on energy, and the person may feel more hungry than usual.
- Weight loss: When there is too little insulin, the body may start burning fat and muscle for energy. This causes weight loss.
- Fatigue: When cells lack glucose, the body becomes tired. Fatigue can interfere with daily life when a person has type 2 diabetes.
- Blurred vision: High blood glucose can cause fluid to be pulled from the lenses of the eyes, resulting in swelling, leading to temporarily blurred vision.
- Infections and sores: It takes longer to recover from infections and sores because blood circulation is poor and there may be other nutritional deficits.
If people notice these symptoms, they should see a doctor. Diabetes can lead to a number of serious complications. The sooner a person starts to manage their glucose levels, the better chance they have of preventing complications.
Symptoms in children and teens
Type 2 diabetes is more likely to appear after the age of 45 years, but it can affect children and teens who:
- have excess weight
- do not do much physical activity
- have high blood pressure
- have a family history of type 2 diabetes
- have an African American, Asian American, Hispanic American, or American Indian background
The following symptoms may occur:
- weight loss, despite increased appetite and hunger
- extreme thirst and dry mouth
- frequent urination and urinary tract infections
- fatigue
- blurred vision
- slow healing of cuts or wounds
- numbness or tingling in hands and feet
- itchy skin
If caregivers notice these symptoms, they should take the child to see a doctor. These are also symptoms of type 1 diabetes. Type 1 is less common but more likely to affect children and teenagers than adults. However, type 2 diabetes is becoming more common in young people than it was in the past.
Symptoms in older adults
At least 25.2 percent of people aged 65 and above have type 2 diabetes in the United States. They may have some or all the classic symptoms of type 2 diabetes.
They may also experience one or more of the following:
- flu-like fatigue, which includes feeling lethargic and chronically weak
- urinary tract infections
- numbness and tingling in the hands, arms, legs, and feet due to circulation and nerve damage
- dental problems, including infections of the mouth and red, inflamed gums
Early signs
Most people do not experience symptoms in the early stages, and they may not have symptoms for many years.
A possible early sign of type 2 diabetes is darkened skin on certain areas of the body, including:
- the neck
- the elbows
- the knees
- the knuckles
This is known as acanthosis nigricans.
Other early symptoms include:
- frequent bladder, kidney, or skin infections
- cuts that take longer to heal
- fatigue
- extreme hunger
- increased thirst
- urinary frequency
- blurred vision
A person may have mild or subtle symptoms for many years, but these can become in time. Further health problems can develop.
Prediabetes and diabetes prevention
A person with blood sugar levels of 100–125 mg/dl will receive a diagnosis of prediabetes. This means that their blood sugar levels are high, but they do not have diabetes. Taking action at this stage can prevent diabetes from developing.
According to a 2016 report published in The Journal of the American Board of Family Medicine, 33.6 percent of people aged 45 years and older had prediabetes in 2012.
The CDC estimate that around 84 million
Complications
Diabetes may cause a number of health complications if people do not manage it properly. Many of these are chronic, or long-term, but they can become life-threatening. Others need immediate medical attention as soon as they appear.
Emergency complications
Complications can arise quickly if blood sugar rises or falls too far.
Hypoglycemia
If blood glucose dips below 70 mg/dl, this is hypoglycemia, or low blood sugar.
This can happen if a person who uses insulin takes more than they need for a particular time.
A home blood glucose test can check for hypoglycemia.
It is vital to know the early signs of hypoglycemia, as it can progress quickly, resulting in seizures and a coma. In the early stages, however, it is easy to treat.
Symptoms of hypoglycemia include:
- confusion
- dizziness
- feeling faint
- heart palpitations
- rapid heartbeat
- mood changes
- loss of consciousness
- sweating
- clamminess
If symptoms are mild, a person can often resolve low blood sugar levels by consuming:
- a few pieces of hard candy
- a cup of orange juice
- a teaspoon of honey
- a glucose tablet
The person should then wait 15 minutes, test their blood sugar, and if it is still low, they should take another glucose tablet or sweet.
When levels return to above 70 mg/dl, the person should eat a meal, to stabilize their glucose levels.
If they remain low for 1 hour or longer, or if symptoms worsen, someone should take the person to the emergency room.
Anyone who has frequent or severe hypoglycemic episodes should speak to their doctor, as they may need to adjust their treatment plan.
Hyperglycemia and diabetic ketoacidosis (DKA)
If blood sugar levels rise too far, hyperglycemia can result. If a person notices increased thirst and urination, they should check their blood sugar levels.
It the level is above the target level that their doctor recomends, they take appropriate action.
Without treatment, high a person with hyperglycemia can develop diabetic ketoacidosis (DKA), which happens when high levels of ketones collect in the blood, making it too acidic. For this reason, the person should also test their ketone levels.
Ketoacidosis can lead to:
- difficulty breathing
- a fruity smell on the breath
- a dry mouth
- nausea and vomiting
- coma
It can be life-threatening. A person with these signs and symptoms should seek immediate medical attention.
People who regularly experience high blood sugar should speak to their doctor about adjusting their treatment plan.
Blood glucose testing kits and ketone testing kits are available for purchase online. People should check with their doctor how often they need to test.
Long-term complications
Keeping blood glucose within target levels can prevent complications that can become life-threatening and disabling over time.
Some possible complications of diabetes are:
- heart and blood vessel diseases
- high blood pressure
- nerve damage (neuropathy)
- foot damage
- eye damage and blindness
- kidney disease
- hearing problems
- skin problems
Effective management of blood glucose levels can reduce the risk of complications.
Diagnosis and treatment
A doctor can diagnose type 2 diabetes with blood tests that measure blood glucose levels. Many people discover they have high blood sugar during a routine screening test, but anyone who experiences symptoms should see a doctor.
Treatment aims to keep blood glucose levels stable at a healthy level and prevent complications. The main ways to do this are through lifestyle measures.
These include:
- following a healthful diet
- reaching and maintaining a healthy weight and body mass index (BMI)
- doing physical activity
- getting enough sleep
- avoiding or quitting smoking
- taking medications or insulin as the doctor recommends
Outlook
There is currently no cure for diabetes, but most people with the condition can lead a healthful life by managing their condition properly.
People who maintain a healthy weight, follow a healthful diet, and do regular exercise may not need medication. Taking these steps can help manage blood sugar levels.
Routine screening can alert a person to high blood sugar levels in the early stages, when there is still time to slow, stop, or reverse the progress of diabetes.
Current guidelines recommend regular screening from the age of 45 years, or younger if an individual has other risk factors, such as obesity. A doctor can advise on individual needs.
What to know about melanoma
Melanoma is a type of skin cancer. It is not the most common, but it is the most serious, as it often spreads. When this happens, it can be difficult to treat, and the outlook may be poor. Risk factors for melanoma include overexposure to the sun, having fair skin, and a family history of melanoma, among others.
Receiving an early diagnosis and getting prompt treatment can improve the outlook for people with melanoma.
For this reason, people should keep track of any changing or growing moles. Using adequate protection against sun exposure can help a person prevent melanoma altogether.
What is melanoma?
Melanoma is a type of skin cancer that occurs when pigment producing cells called melanocytes mutate and begin to divide uncontrollably.
Most pigment cells develop in the skin. Melanomas can develop anywhere on the skin, but certain areas are more at risk than others. In men, it is most likely to affect the chest and back. In women, the legs are the most common site. Other common sites of melanoma include the face.
However, melanoma can also occur in the eyes and other parts of the body, including — on very rare occasions — the intestines.
Melanoma is relatively rare in people with darker skin.
Stages
The stage of a cancer at diagnosis will indicate how far it has already spread and what kind of treatment will be suitable.
One method of assigning a stage to melanoma describes the cancer in five stages, from 0 to 4:
- Stage 0: The cancer is only present in the outermost layer of skin. Doctors refer to this stage as “melanoma in situ.”
- Stage 1: The cancer is up to 2 millimeters (mm) thick. It has not yet spread to lymph nodes or other sites, and it may or may not be ulcerated.
- Stage 2: The cancer is at least 1 mm thick but may be thicker than 4 mm. It may or may not be ulcerated, and it has not yet spread to lymph nodes or other sites.
- Stage 3: The cancer has spread to one or more lymph nodes or nearby lymphatic channels but not distant sites. The original cancer may no longer be visible. If it is visible, it may be thicker than 4 mm and also ulcerated.
- Stage 4: The cancer has spread to distant lymph nodes or organs, such as the brain, lungs, or liver.
The more advanced a cancer is, the harder it is to treat and the worse the outlook becomes.
Types
There are four types of melanoma. Learn more about each type in the sections below.
Superficial spreading melanoma
This is the most common type of melanoma, and it often appears on the trunk or limbs. The cells tend to grow slowly at first before spreading across the surface of the skin.
Nodular melanoma
This is the second most common type of melanoma, appearing on the trunk, head, or neck. It tends to grow quicker than other types, and it may appear as a reddish or blue-black color.
Lentigo maligna melanoma
This is less common and tends to develop in older adults, especially in parts of the body that have had excessive sun exposure over several years, such as the face.
It starts as a Hutchinson’s freckle, or lentigo maligna, which looks like a stain on the skin. It usually grows slowly and is less dangerous than other types of melanoma.
Acral lentiginous melanoma
This is the rarest kind of melanoma. It appears on the palms of the hands, soles of the feet, or under the nails.
Since people with darker skin do not typically get other types of melanoma, these tend to be the most common type of melanoma in those with darker skin types.
Risk factors
Research into the exact causes of melanoma is ongoing.
However, scientists do know that people with certain skin types are more prone to developing melanoma.
The following factors may also contribute to an increased risk of skin cancer:
- a high density of freckles or a tendency to develop freckles following exposure to the sun
- a high number of moles
- five or more atypical moles
- the presence of actinic lentigines, also known as liver spots or age spots
- giant congenital melanocytic nevi, a type of brown birthmark
- pale skin that does not tan easily and tends to burn
- light eyes
- red or light hair
- high sun exposure, particularly if it produces blistering sunburn, and if sun exposure is intermittent rather than regular
- older age
- a family or personal history of melanoma
- a previous organ transplant
Of these risk factors, only sun exposure and sunburn are avoidable. Avoiding overexposure to the sun and preventing sunburn can significantly lower the risk of skin cancer. Tanning beds are also a source of damaging ultraviolet (UV) rays.
Being able to tell the difference between normal moles or freckles and those that indicate skin cancer can support an early diagnosis.
- Superficial spreading melanoma
- Nodular melanoma
- Lentigo maligna melanoma
- Acral lentiginous melanoma
- Skin changes due to cancer
- Normal mole
Symptoms
In its early stages, melanoma can be difficult to detect. It is important to check the skin for any signs of change.
Alterations in the appearance of the skin are vital indicators of melanoma. Doctors use them in the diagnostic process.
The Melanoma Research Foundation offer pictures of melanomas and normal moles to help a person learn how to tell the difference.
They also list some symptoms that should prompt a person to visit the doctor, including:
- any skin changes, such as a new spot or mole or a change in the color, shape, or size of an existing spot or mole
- a skin sore that fails to heal
- a spot or sore that becomes painful, itchy, or tender
- a spot or sore that starts to bleed
- a spot or lump that looks shiny, waxy, smooth, or pale
- a firm, red lump that bleeds or looks ulcerated or crusty
- a flat, red spot that is rough, dry, or scaly
ABCDE examination
The ABCDE examination of moles is an important method for revealing potentially cancerous lesions. It describes five simple characteristics to check for in a mole that can help a person either confirm or rule out melanoma:
- Asymmetric: Noncancerous moles tend to be round and symmetrical, whereas one side of a cancerous mole is likely to look different to the other side.
- Border: This is likely to be irregular rather than smooth and may appear ragged, notched, or blurred.
- Color: Melanomas tend to contain uneven shades and colors, including black, brown, and tan. They may even contain white or blue pigmentation.
- Diameter: Melanoma can cause a change in the size of a mole. For example, if a mole becomes larger than one-quarter of an inch in diameter, it might be cancerous.
- Evolving: A change in a mole’s appearance over weeks or months can be a sign of skin cancer.
Treatment
The treatment of skin cancer is similar to that of other cancers. However, unlike many cancers inside the body, it is easier to access the cancerous tissue and remove it completely. For this reason, surgery is the standard treatment option for melanoma.
Surgery involves removing the lesion and some of the noncancerous tissue around it. When the surgeon removes the lesion, they send it to pathology to determine the extent of the involvement of the cancer, and to make sure that they have removed all of it.
If melanoma covers a large area of skin, a skin graft may be necessary.
If there is a risk that the cancer has spread to the lymph nodes, a doctor may request a lymph node biopsy.
They may also recommend radiation therapy for treating melanoma, especially in the later stages.
Melanoma may metastasize to other organs. If this happens, a doctor will request treatments depending on where the melanoma has spread, including:
- chemotherapy, in which a doctor uses medications that target the cancer cells
- immunotherapy, in which a doctor administers drugs that work with the immune system to help fight the cancer
- targeted therapy, which uses medications that identify and target particular genes or proteins specific to melanoma
Prevention
Avoiding excessive exposure to UV radiation can reduce the risk of skin cancer. People can achieve this by:
- avoiding sunburn
- wearing clothes that protect the body from the sun
- using broad spectrum sunscreen with a minimum sun protection factor (SPF) of 30, preferably a physical blocker such as zinc oxide or titanium dioxide
- liberally applying sunscreen about half an hour before going outside in the sun
- reapplying sunscreen every 2 hours and after swimming or sweating to maintain adequate protection
- avoiding the highest sun intensity by finding shade between the hours of 10 a.m. and 4 p.m.
- keeping children in the shade as much as possible, having them wear protective clothing, and applying SPF 50+ sunscreen
- ]keeping infants out of direct sunlight
Wearing sunscreen is not a reason to spend longer in the sun. People should still take steps to limit sun exposure where possible.
Those who work outdoors should also take precautions to minimize exposure.
Doctors recommend avoiding tanning booths, lamps, and sunbeds.
What about vitamin D?
The American Academy of Dermatology (AAD) do not currently recommend sun exposure (or tanning) for the purpose of obtaining vitamin D.
Instead, they suggest “getting vitamin D from a [healthful] diet that includes foods naturally rich in vitamin D, foods and beverages fortified with vitamin D, and/or vitamin D supplements”
Diagnosis
Most cases of melanoma affect the skin. They usually produce changes in existing moles.
A person can detect the early signs of melanoma themselves by regularly examining existing moles and other colored blemishes and freckles. People should have their backs checked regularly, as it may be harder to see moles in this area.
A partner, family member, friend, or doctor can help check the back and other areas that are hard to see without assistance.
Any changes in the skin’s appearance require further examination by a doctor.
Some apps claim to help a person identify and track changing moles. However, many are not reliable.
Clinical tests
Doctors may use microscopic or photographic tools to examine a lesion in more detail.
If they suspect skin cancer, they will have a dermatologist biopsy the lesion to determine whether or not it is cancerous. A biopsy is a procedure wherein a medical professional takes a sample of a lesion and sends it for examination in the laboratory.
Outlook
Melanoma is an aggressive type of cancer that can be dangerous when it spreads. However, people who identify a lesion early can have a very good outlook.
The ACS have calculated the 5 year relative survival rates for melanoma. These compare the likelihood that a person with melanoma will survive for 5 years with that of a person without cancer.
If a doctor diagnoses and treats melanoma before it spreads, the 5 year relative survival rate is 98%. If it spreads to deeper tissues or nearby lymph nodes, however, the rate drops to 64%.
If it reaches distant organs or tissues, the likelihood of surviving for 5 years reduces to 23%.
For this reason, it is important to monitor any changing moles and seek medical attention for any that are changing, irregular, or growing. Taking preventive steps is also vital when spending long periods of time in the sun.

Medical myths: All about heart disease
This week’s edition of Medical Myths will focus its beams on the many half-truths and misconceptions that surround heart disease. Among other topics, we cover smoking, coughing, exercising, supplements, and statins.
Globally, heart disease is the number one cause of death. It is responsible for 17.9 million deaths each year.
According to the Centers for Disease Control and Prevention (CDC), in the United States, one person dies every 36 seconds from cardiovascular disease. Heart disease accounts for 1 in 4 deaths in the U.S.
1. Young people do not need to worry about heart disease
It is true that heart disease is more likely to affect people over the age of 65, but 4–10% of heart attacks occur in people under the age of 45 years, mainly in men. In addition, it is how we live our lives as children, adolescents, and adults that lays the groundwork for heart health as we age.
For instance, eating a diet that is high in trans and saturated fats or smoking tobacco slowly increases the risk of heart disease as we age. Changes to lifestyle today build the foundation for a healthier heart in later life.
In the U.S. as a whole, heart disease mortality has slowly dropped since the 1970s , although the trend seems to be slowing. However, in some regions, rates have increased.
One study that investigated heart disease mortality in different age groups in the U.S. found that “over 50% of counties experienced increases in heart disease mortality from 2010 through 2015 among adults aged 35–64 years.”
2. People should avoid exercise if they have heart disease
This is a myth. Exercise helps strengthen the heart muscle and improve blood flow around the body.
In August 2020, the European Society of Cardiology published guidelines on exercise in patients with cardiovascular disease. Prof. Sanjay Sharma, who was involved in creating the guidelines, explains:
“The chance of exercise triggering a cardiac arrest or heart attack is extremely low.” However, he also adds a note of caution: “People who are completely inactive and those with advanced heart disease should consult their doctor before taking up sports.”
3. I take cholesterol-lowering drugs, so I can eat whatever I like
Some drugs, such as statins, reduce the level of cholesterol in the blood. However, this does not mean that a person who is taking statins can consume foods containing saturated fats with abandon.
Cholesterol is either consumed in the food that you eat or produced in the liver. Statins block an enzyme in the liver that is necessary for producing cholesterol, reducing overall blood cholesterol levels. However, this means that ingested cholesterol can still make it into the blood.
In short, statins may just be able to override the adverse effects of a poor diet, but a poor diet will increase risk of other independent risk factors for heart disease, such as obesity, hypertension, and diabetes.
4. Heart disease runs in my family, so there is nothing I can do to stop it
If close family members have experienced heart disease, it could mean that you have an increased risk. However, it is not set in stone, and there are a number of ways to reduce the risk, even for people with a genetic susceptibility.
These include eating a healthful diet, stopping smoking, managing blood pressure, and exercising regularly.
It is also worth noting that if heart disease runs in the family, it may not be a sign of genetic susceptibility. Families tend to share lifestyle factors, such as diet and exercise habits, both of which can impact the risk of heart disease.
5. Vitamins can prevent heart disease
Although most vitamins, taken at the recommended doses, are unlikely to be bad for heart health, there is no evidence that taking any vitamin supplements can reduce the risk of heart disease. And they certainly cannot replace a healthful diet and regular exercise.
For instance, a systematic review and meta-analysis looked for associations between multivitamin and mineral supplements and a number of cardiovascular outcomes, including coronary heart disease and stroke.
The analysis, published in 2018, took data from 18 existing studies, including 2,019,862 participants.
The authors concluded that multivitamin and mineral “supplementation does not improve cardiovascular outcomes in the general population.”
According to Victoria Taylor, the nutrition lead at the British Heart Foundation: “There are no shortcuts when it comes to nutrition — supplements are not a replacement for healthy food. You might be prescribed a vitamin or mineral supplement by a health professional for other reasons, but we do not recommend people take multivitamins to help prevent heart and circulatory diseases.”
6. I have smoked for years, there is no point stopping now
This is a myth. Smoking tobacco is a major cause of heart disease. As soon as a person stops smoking, the health benefits begin. The National Institute on Aging write:
“It doesn’t matter how old you are or how long you’ve been smoking, quitting smoking at any time improves your health. When you quit, you are likely to add years to your life, breathe more easily, have more energy, and save money.”
They also explain that you will lower the risk of heart attack and stroke and have better circulation.
7. Heart disease only really affects men
This is a myth, as heart disease is the leading cause of death in both men and women. In 2017 in the U.S., 24.2% of men and 21.8% of women died from heart disease.
However, when strokes, which have similar risk factors, are added in, the figures are even more similar between men and women: 28.7% of men and 28% of women died from heart disease or stroke.
It is a common misconception that only men are affected by heart disease. It is true that men tend to develop cardiovascular disease at an earlier age than women and have a greater risk of coronary heart disease. However, women have a higher risk of stroke.
One paper explains, “Although the incidence of [cardiovascular disease] in women is usually lower than in men, women have a higher mortality and worse prognosis after acute cardiovascular events.”
8. Cardiac arrest and heart attack are the same
Heart attacks and cardiac arrests are not the same thing. A heart attack is a circulation problem. It occurs when the coronary artery, which carries oxygenated blood to the muscles of the heart, becomes blocked.
A cardiac arrest is an “electrical problem,” where the heart stops pumping blood around the body effectively. Cardiac arrests are often caused by a heart attack.
During a heart attack, an individual is likely to be conscious. During a cardiac arrest, they are almost always unconscious. Both are a medical emergency.
9. Coughing during a heart attack can save your life
According to some sources, coughing vigorously during a heart attack — so-called cough CPR — can save your life.
This is an internet distortion of a paper published over 40 years ago, which showed that patients who had a cardiac arrest during arteriography in hospital and who coughed every 1–3 seconds stayed conscious for an additional 39 seconds.
There is no evidence that this technique works in the community for heart attacks that are not induced by medical procedures.
According to Christopher Allen, a senior cardiac nurse:
“The absolute priority when you think you or someone else is having a heart attack is to call [the emergency services]. This way, paramedics can assess and aid you, and you’ll get to hospital as fast as possible. There is no medical evidence to support ‘cough CPR.’”
10. People with heart disease should avoid eating all fat
A person with cardiovascular disease certainly should reduce their intake of saturated fats — which are found in foods such as butter, biscuits, bacon, and sausages — and partially hydrogenated and trans fats, which are found in foods such as baked goods, frozen pizzas, and microwave popcorn.
However, unsaturated fats can provide benefits. For instance, there is some evidence that omega-3, which is a polyunsaturated fat, might protect heart health.
The American Heart Association recommend “that all adults eat fish (particularly fatty fish) at least 2 times a week. Fish is a good source of protein and is low in saturated fat. Fish, especially oily species like mackerel, lake trout, herring, sardines, albacore tuna, and salmon, provide significant amounts of the two kinds of omega-3 fatty acids shown to be cardioprotective, eicosapentaenoic acid and docosahexaenoic acid.”
They also recommend eating plant-derived omega-3 fatty acids. These can be found in tofu and other forms of soybeans; walnuts, flaxseeds, and their oils; and canola oil.
The take-home
Heart disease is common, but it is not inevitable. There are lifestyle changes that we can all implement to reduce the risk of developing cardiovascular problems, whatever our age.

What is music therapy, and how does it work?
Music therapy involves using a person’s responses and connections to music to encourage positive changes in mood and overall well-being. Music therapy can include creating music with instruments of all types, singing, moving to music, or just listening to it.
Music has powerful effects on the mind. Different styles of music can have a significant effect on a person’s mood very quickly, and it can help them experience and process a wide range of emotions, from happiness to excitement, as well as sadness, calmness, and thoughtfulness.
Making music can also be as beneficial as listening to music, and music therapy encourages people to actively create the music they find helpful to them.
This article explains what music therapy is, how it can help improve mental health, and its effects on different mental health conditions.
What is music therapy?
Music therapy uses the powerful abilities of music to improve a person’s well-being. It is an alternative to other types of therapy, such as counseling or cognitive behavioral therapy (CBT).
Music therapists use a person’s responses and connections to music to encourage positive changes in mood and overall mental mindset. Music therapy can include listening to music or creating music with instruments of all types. It may also involve singing or moving to music.
It can help improve confidence, communication skills, independence, self-awareness and awareness of others, and concentration and attention skills.
Live musical interaction between a person and their therapist is important during music therapy.
Improvisation can also be a key part of music therapy. This involves making music up on the spot in response to a mood or a theme, such as making the sound of a storm using drums and a rainstick.
How does music therapy work?
The way that music affects the brain is very complex. All aspects of music — including pitch, tempo, and melody — are processed by different areas of the brain.
For instance, the cerebellum processes rhythm, the frontal lobes decode the emotional signals created by the music, and a small portion of the right temporal lobe helps understand pitch.
The reward center of the brain, called the nucleus accumbens, can even produce strong physical signs of pleasure, such as goosebumps, when it hears powerful music.
Music therapy can use these deep physical reactions the body has to music to help people with mental health conditions.
History and origins
Music has been a part of human life for thousands of years. Specifically, experts have found instruments dating back to over 40,000 years ago, suggesting that humans’ desire to express themselves or communicate through music is deep rooted.
The use of music for therapy and healing dates back to Ancient Greece, but its therapeutic use today began in the 20th century, after World War II had ended. The earliest reference to music therapy comes from a 1789 article called “Music physically considered.”
The 1800s saw medical research into the therapeutic nature of music grow, and by the 1940s, universities were offering music therapy programs. E. Thayer Gaston, one of three men who pioneered the use of music as a therapeutic tool, had organized and promoted the practice so that it would become an accepted type of therapy.
Now, there are many music therapy associations around the world, and music therapists work in private care, education, and social care.
Music therapy vs. other forms of therapy
Music therapy does not rely on verbal communication, so it can be better for people who struggle to communicate verbally. This could be due to a disability, a neurodegenerative condition such as dementia, an acquired brain injury, or a mental health condition.
As CBT and counseling are both talking therapies, they may not be suitable for people who find verbal communication difficult. This is where music therapy can be beneficial.
Additionally, mental health practitioners can bring music therapy directly to a person, such as if they cannot get out of bed or are unable to get to a therapist’s office. Enjoying music therapy at home can also benefit children who want to be in a familiar environment during their sessions.
This is not specific to music therapy, though, as many other types of psychotherapy can take place in the home.
The skills a person learns in music therapy can be useful in their everyday life, too. They may even take up learning an instrument as a new hobby, which they can use as a tool for improving their mental health and coping with difficult situations throughout their life.
Benefits
There are extra benefits to listening or creating music that talking therapies may not be able to offer.
For instance, learning and practicing a piece of music can improve memory skills, coordination, reading, comprehension, and math skills, and it can also give lessons in responsibility and perseverance.
People can also enjoy a great sense of achievement from creating a piece of music, which can help improve their mood and self-esteem.
Music therapy can also introduce people to many different cultures, as clients can explore any type and genre of music during therapy. Understanding the history behind a piece of music can help people connect with the music they are hearing or playing.
Although self-expression is a part of talking therapy, music therapy allows people to express themselves in a creative way, which can be a more enjoyable way of exploring difficult emotions.
Lyric analysis is another accessible way for people to explore and process difficult emotions, experiences, or memories through music.
For example, a person can find themes and meanings within lyrics and offer alternative lyrics that apply to their life and experiences, which can help them find the words that represent how they are feeling if they are finding it hard to express this themselves.
Some of the documented benefits of music therapy include:
- improved self-esteem
- decreased anxiety
- increased motivation
- successful and safe emotional release
- increased verbalization
- stronger connections with other people
How it helps with anxiety
Many studies suggest that music therapy can reduce feelings of anxiety, including in people with cancer, those undergoing surgery, and individuals going into intensive care units. Some studies also suggest that music can reduce blood pressure and the heartbeat, which can have a direct impact on how stressed a person feels.
There is also evidence to suggest that those undergoing music therapy experience reduced anxiety immediately after the session, which indicates that music therapy could be a convenient way to reduce symptoms quickly.
Music affects the amount of stress hormones, such as adrenaline and cortisol, that the body releases, and reducing these hormones can help relieve symptoms of anxiety.

Everything you need to know about inflammation
Inflammation is part of the body’s defense mechanism and plays a role in the healing process.
When the body detects an intruder, it launches a biological response to try to remove it.
The attacker could be a foreign body, such as a thorn, an irritant, or a pathogen. Pathogens include bacteria, viruses, and other organisms, which cause infections.
Sometimes, the body mistakenly perceives its own cells or tissues as harmful. This reaction can lead to autoimmune diseases, such as type 1 diabetes.
Experts believe inflammation may contribute to a wide range of chronic diseases. Examples of these are metabolic syndrome, which includes type 2 diabetes, heart disease, and obesity.
People with these conditions often have higher levels of inflammatory markers in their bodies.
Types and symptoms
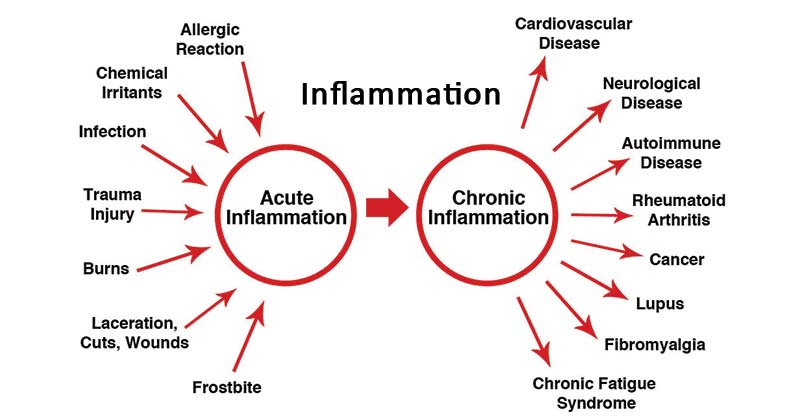
There are two main types of inflammation: acute and chronic.
Acute inflammation
An injury or illness can involve acute, or short-term, inflammation.
There are five key signs of acute inflammation:
- Pain: This may occur continuously or only when a person touches the affected area.
- Redness: This happens because of an increase in the blood supply to the capillaries in the area.
- Loss of function: There may be difficulty moving a joint, breathing, sensing smell, and so on.
- Swelling: A condition call edema can develop if fluid builds up.
- Heat: Increased blood flow may leave the affected area warm to the touch.
These signs are not always present. Sometimes inflammation is “silent,” without symptoms. A person may also feel tired, generally unwell, and have a fever.
Symptoms of acute inflammation last a few days. Subacute inflammation lasts 2–6 weeks.
Chronic inflammation can continue for months or years. It either has or may have links to various diseases, such as:
- diabetes
- cardiovascular disease (CVD)
- arthritis and other joint diseases
- allergies
- chronic obstructive pulmonary disease (COPD)
- psoriasis
- rheumatoid arthritis
The symptoms will depend on the disease, but they may include pain and fatigue.
Measuring inflammation
When inflammation is present in the body, there will be higher levels of substances known as biomarkers.
An example of a biomarker is C-reactive protein (CRP). If a doctor wants to test for inflammation, they may assess CRP levels.
CRP levels tend to be higher in older people and those with conditions such as cancer and obesity. Even diet and exercise may make a difference.
Causes
Inflammation happens when a physical factor triggers an immune reaction. Inflammation does not necessarily mean that there is an infection, but an infection can cause inflammation.
Acute inflammation
Acute inflammation can result from:
- exposure to a substance, such as a bee sting or dust
- an injury
- an infection
When the body detects damage or pathogens, the immune system triggers a number of reactions:
- Tissues accumulate plasma proteins, leading to a buildup of fluid that results in swelling.
- The body releases neutrophils, a type of white blood cell, or leukocyte, which move toward the affected area. Leukocytes contain molecules that can help fight pathogens.
- Small blood vessels enlarge to enable leukocytes and plasma proteins to reach the injury site more easily.
Signs of acute inflammation can appear within hours or days, depending on the cause. In some cases, they can rapidly become severe. How they develop and how long they last will depend on the cause, which part of the body they affect, and individual factors.
Some factors and infections that can lead to acute inflammation include:
- acute bronchitis, appendicitis and other illnesses ending in “-itis”
- an ingrown toenail
- a sore throat from a cold or flu
- physical trauma or wound
Chronic inflammation
Chronic inflammation can develop if a person has:
Sensitivity: Inflammation happens when the body senses something that should not be there. Hypersensitivity to an external trigger can result in an allergy.
Exposure: Sometimes, long-term, low-level exposure to an irritant, such as an industrial chemical, can result in chronic inflammation.
Autoimmune disorders: The immune system mistakenly attacks normal healthy tissue, as in psoriasis.
Autoinflammatory diseases: A genetic factor affects the way the immune system works, as in Behçet’s disease.
Persistent acute inflammation: In some cases, a person may not fully recover from acute inflammation. Sometimes, this can lead to chronic inflammation.
Factors that may increase the risk of chronic inflammation include:
- older age
- obesity
- a diet that is rich in unhealthful fats and added sugar
- smoking
- low sex hormones
- stress
- sleep problems
Long-term diseases that doctors associate with inflammation include:
- asthma
- chronic peptic ulcer
- tuberculosis
- rheumatoid arthritis
- periodontitis
- ulcerative colitis and Crohn’s disease
- sinusitis
- active hepatitis
Inflammation plays a vital role in healing, but chronic inflammation may increase the risk of various diseases, including some cancers, rheumatoid arthritis, atherosclerosis, periodontitis, and hay fever.