Immune aging and how to combat it
With age, the human immune system becomes less effective at tackling infections and less responsive to vaccinations. At the same time, the aging immune system is associated with chronic inflammation, which increases the risk of almost all conditions linked to old age.
The good news is that exercising and adopting the right diet may help a person maintain healthy immunity into older age.
Chimpanzees and gorillas, our closest primate relatives, live for only 10–15 years in the wild once they have reached maturity. After the human evolutionary lineage split from theirs, our ancestors’ life expectancy doubled over the next 5 million years.
Scientists believe that it remained relatively stable into the 18th century. In the 250 years between then and now, however, life expectancy more than doubled again due to improvements in sanitation and healthcare.
We live in a time of high average life expectancies. However, our long evolutionary history has adapted us for different lifestyles (and even life expectancies), and these have changed drastically.
As a result, immunity not only weakens in older age; it also becomes imbalanced. This affects the two branches of the immune system — “innate” immunity and “adaptive” immunity — in a double whammy of “immunosenescence.”
“Innate” immunity, which is our first line of defense against infections, fails to resolve after the initial threat has passed, causing chronic, systemic inflammation.
“Adaptive” immunity, which is responsible for remembering and attacking particular pathogens, steadily loses its ability to defend against viruses, bacteria, and fungi.
Chronic, low-grade inflammation is associated with almost all conditions linked to older age, including type 2 diabetes, cardiovascular disease, cancer, and dementia. It also plays a leading role in certain autoimmune conditions that are more common in older adults, such as rheumatoid arthritis.
Meanwhile, the loss of adaptive immunity that comes with older age not only makes people more susceptible to infections; it can also reactivate dormant pathogens that were previously suppressed.
In addition, the weaker adaptive immunity of older adults means that their bodies respond less strongly to vaccinations, such as the annual flu shot.
Aging and innate immunity
Researchers have dubbed the persistent, low-level inflammation that is implicated in almost all conditions associated with older age as “inflammaging.”
“While inflammation is part of the normal repair response for healing, and essential in keeping us safe from bacterial and viral infections and noxious environmental agents, not all inflammation is good. When inflammation becomes prolonged and persists, it can become damaging and destructive.”
After an initial infection or injury, younger people’s immune systems switch to an anti-inflammatory response. This does not appear to happen as effectively in older adults. This is due to the accumulation of aged, or “senescent,” immune cells.
Senescent cells have shorter telomeres, which are the protective caps at the tips of chromosomes. Just as the plastic caps on the ends of shoelaces prevent them from fraying, telomeres prevent vital genetic material from becoming lost when the chromosome is copied during cell replication.
Telomeres get a little shorter every time a cell divides, until, eventually, division has to stop completely. If the cell survives, it becomes steadily more dysfunctional.
Senescent immune cells produce more immune signaling molecules called cytokines, which promote inflammation. Specifically, they churn out more interleukin 6 (IL-6) and tumor necrosis factor-alpha (TNF-alpha).
Scientists have linked high levels of IL-6 and TNF-alpha to disability and mortality in older adults. They have a particularly strong association with type 2 diabetes, cardiovascular disease, neurodegenerative disease, and cancer.
As the number of pro-inflammatory cells increases, there is an increase in the number of immune cells called M1 macrophages (more pro-inflammatory) and a decrease in the number of M2 macrophages (more immunoregulatory).
These changes in the frequency of M1 and M2 cells seem to be associated with an increased risk of developing plaques comprising fat and debris, which block the arteries in atherosclerosis.
Aging and adaptive immunity
Through adaptive immunity, the immune system learns to recognize and neutralize particular pathogens.
A type of immune cell known as a T cell plays a crucial role in adaptive immunity. In the course of an infection, “naïve” T cells learn to recognize the specific pathogen involved. They then differentiate into cells that are specialized to mount future immune responses against the same pathogen.
The total number of T cells remains constant throughout our lifetime, but the pool of naïve, undifferentiated cells steadily shrinks over the years, as more and more cells commit to tackling specific infections.
As a result, the bodies of older adults become less able to mount effective immune responses to new infections. For the same reason, vaccinations provoke weaker responses from the aging immune system and, therefore, provide less protection.
Ironically, a lifetime of influenza vaccinations may, in itself, diminish the efficacy of the annual vaccine later in life. Indeed, research suggests that repeated influenza immunizations could lead to reduced antibody responses.
Many older adults harbor a latent infection of human cytomegalovirus. This viral infection is very common and persistent, and it usually produces few (if any) symptoms. However, in older adults, this infection may steadily deplete their immune resources, making them more prone to other viral infections and reducing the effect of influenza immunizations.
In addition to this slow decline in immunity with age, senescent T cells also produce more pro-inflammatory cytokines, such as IL-6. These, in turn, stoke the chronic, systemic inflammation of inflammaging.
Holding back the years
Although nothing can prevent aging, there are certain lifestyle changes a person can make to stay healthy into older age.
The sections below will look at these factors in more detail.
Getting regular physical activity
Exercise has a profound effect on the immune system, according to a recent overview of research in the journal Nature Reviews Immunology.
Inevitably, people become less physically active as they age, but there is evidence to suggest that getting as much exercise as possible can slow or even reverse some of the effects of immunosenescence.
Skeletal muscle produces a range of proteins called myokines that reduce inflammation and preserve immune function. Therefore, it makes sense that maintaining muscle mass through exercise protects against infection and conditions such as type 2 diabetes and cardiovascular disease, which are closely linked to chronic inflammation.
One study found that aerobic fitness among 102 healthy males, aged 18–61 years, was inversely proportional to the number of senescent T cells in their blood after adjusting for age. In other words, increased physical fitness was associated with less immunosenescence.
The fittest males not only had fewer senescent T cells but a greater number of naïve T cells.
Another study compared the immune responses of 61 healthy males, aged 65–85 years, to a flu vaccination. Around one-third of the males were intensively active (though participation in running or sports), one-third were moderately active, and one-third were mostly inactive.
After adjusting for their age, the researchers found that the intensively and moderately active males produced more antibodies in response to vaccination than the least active males.
Remarkably, the more active males had higher serum concentrations of antibodies to some flu strains even before they underwent vaccination.
A range of other studies have identified similar benefits, not only from long-term physical activity but also from single bouts of exercise before vaccination.
“Taken together, these studies suggest that the emergence of certain features of immunosenescence and the extent of immune remodeling is likely to be heavily influenced by insufficient physical activity as humans age.”
It is important to note that the majority of the research into the relationship between exercise and immunity in older adults has involved “cross-sectional” studies. This type of study investigates relationships between variables at a single point in time.
To confirm the benefits of physical fitness, the authors of the review above call for more “interventional” studies, which would follow participants over time.
Adopting the Mediterranean diet
For now, there is no direct evidence to suggest that making dietary changes can slow the rate of immunosenescence in older adults. However, there is plenty of indirect evidence.
In particular, research suggests that diet helps determine older adults’ risk of developing sarcopenia. This condition causes a loss of muscle mass, strength, and functionality.
There appears to be a two-way relationship between skeletal muscle and the immune system. Muscles produce anti-inflammatory myokines, but recent evidence suggests that chronic inflammation also accelerates the muscle loss in sarcopenia.
Taking dietary supplements that reduce the risk of sarcopenia — such as vitamin D and polyunsaturated fatty acids — may help, due to their anti-inflammatory properties.
A growing body of evidence also suggests that people who eat a Mediterranean diet are less likely to become “frail” in older age, such as by losing muscle strength, walking slowly, and tiring easily.
The Mediterranean diet comprises:
- large amounts of fruit, leafy vegetables, and olive oil
- moderate amounts of fish, poultry, and dairy
- low amounts of red meat and added sugar
Previous studies have linked this diet to a lower risk of obesity, cardiovascular disease, type 2 diabetes, and cancer.
A 2018 review of observational studies, which Medical News reported on, found that people who adhered the most closely to the Mediterranean diet were less than half as likely to become frail over a 4-year period, compared with those who followed it the least closely.
Among other possible explanations, this may be a result of the diet’s anti-inflammatory properties. The authors write:
“Frail individuals have higher levels of inflammatory markers, and inflammation is considered to be closely associated with frailty. A Mediterranean diet is associated with low levels of inflammatory markers and may reduce frailty risk through this mechanism.”
Maintaining a moderate weight
Although muscle plays a role in reducing inflammation in older adults, fat, or “adipose,” tissue may have the opposite effect.
Normal aging often leads to weight gain, due to an accumulation of adipose tissue beneath the skin and around the organs. According to a roundup of research on the aging immune system, adipose tissue may make a significant contribution to inflammaging.
Up to 30% of the pro-inflammatory cytokine IL-6 in the bloodstream may originate from adipose tissue. Therefore, having obesity or overweight in older age may significantly contribute to chronic inflammation.
In addition, animal and human studies suggest that the immune system of people with obesity may produce fewer antibodies in response to the flu vaccination.
Exercising and eating a healthful diet appear to counter the effects of immune aging. In part, this might be due to the way that these two lifestyle factors prevent excessive weight gain.
Studies have suggested that older adults who exercise regularly and have a moderate weight have fewer senescent T cells and lower levels of pro-inflammatory cytokines in their blood.
However, whether or not diet, exercise, and weight loss can reverse immunosenescence remains an open question for future research.
What causes blackouts?
A blackout is a loss of consciousness or complete or partial memory loss. Possible causes of blackouts include epilepsy and drinking a large volume of alcohol.
If a person notices someone falling unconscious, they should put them in a seated position or help them lie down so that they do not hurt themselves.
What is a blackout?
Some people define blackouts as a temporary loss of consciousness that typically lasts for a few minutes.
However, a 2016 review observes that overconsuming alcohol may lead to alcohol-induced blackouts, which can, in some cases, be due to memory loss rather than a loss of consciousness.
Other possible causes of blackouts include syncope, epilepsy, and stress.
Alcohol blackouts
Two different kinds of blackouts can result from drinking alcohol: en bloc and fragmentary.
When a person consumes a very large volume of alcohol, an en bloc blackout may occur. If this happens, they will not remember anything that they did while they were drinking.
Fragmentary blackouts tend to affect only patches of memory, so a person may be able to piece together a memory on prompting.
Symptoms
If someone has drunk too much alcohol, they may have the following symptoms of alcohol intoxication:
- becoming confused
- difficulty staying awake, or not being able to wake up
- clammy skin and low body temperature
- slow heart rate
- vomiting and seizures
Treatment
If a person is showing symptoms of severe alcohol intoxication, it is important to call the emergency services for treatment.
According to the National Institute on Alcohol Abuse and Alcoholism, a very high blood-alcohol concentration may result in a person struggling to remain conscious. In the most severe cases of alcohol intoxication, they may even fall into a coma. Due to this, it is really important to get someone emergency help if their condition is deteriorating.
In cases where someone who has drunk too much needs first aid, people should:
- lie the person down on their side with their knees up so that they will not choke on their vomit
- check that they are breathing every 15 minutes
- monitor their condition and call 911 immediately if it worsens
Syncope blackouts
The American Heart Association (AHA) describe a syncope blackout as a short temporary loss of consciousness that happens when not enough blood reaches the brain.
People may also refer to this type of blackout as fainting. Low blood pressure typically causes syncope blackouts because the heart cannot pump enough oxygen-rich blood to the brain.
There are two main types of syncope blackouts: neurally mediated and cardiac.
A neurally mediated syncope is usually benign and requires no further treatment. It could occur when a person’s blood pressure drops after they experience pain or dehydration or get up too quickly. This type of syncope tends to occur more in children and young adults.
A cardiac syncope is more serious as it could signal an underlying problem with the heart. Tachycardia, bradycardia, or other types of hypotension could cause a cardiac syncope. If a person does not get treatment, they are at risk of complications or even sudden cardiac death.
Treatment
A doctor may prescribe fludrocortisone to reduce blackouts in people who experience neurally mediated syncope.
If anyone feels as though they are about to faint, they should sit or lie down so that they do not injure themselves if they fall unconscious.
Diagnosis
If a person is experiencing syncope blackouts, a doctor may request an electrocardiogram (EKG) to see whether there are any underlying problems with the heart.
They may also order a tilt test. During this test, a person lies down on a board that moves to change their position while healthcare professionals measure their blood pressure and heart rate.
Epilepsy blackouts
A disturbance of neuronal activity in the brain can cause an epileptic episode. During these episodes, people may experience a seizure. Their muscles may contract, and they could lose consciousness.
However, just because a person has epilepsy, it does not necessarily mean that they will blackout when they have a seizure. The disorder is a spectrum, and it covers many other symptoms.
Symptoms
Many different symptoms could accompany epileptic blackouts, depending on the type of seizure that a person is experiencing.
According to the University of California, San Francisco, one particular type of epileptic seizure that causes blackouts is a tonic-clonic seizure — also known as a grand-mal seizure. During this epileptic episode, people lose consciousness, and the body goes stiff (tonic phase). The muscles then contract, which may result in the jaw clamping shut (clonic phase).
Treatment
The National Institute of Neurological Disorders and Stroke estimate that 70% of people with epilepsy can control their symptoms by taking medication or undergoing surgery.
Since the Food and Drug Administration (FDA) approved them in 2019, doctors have been able to prescribe cenobamate tablets for adults who experience blackouts during seizures. If medication proves ineffective, doctors may recommend surgery.
Some children may be unable to take medication due to the side effects. In these cases, they may benefit from special diets.
Diagnosis
If a doctor suspects that a person has epilepsy, they may request an MRI or CT scan. These imaging techniques help the doctor examine brain activity and rule out other neurological conditions.
Learn more about epilepsy here.
Can stress cause blackouts?
If a person experiences blackouts as a result of stress, this is known as a psychogenic blackout. While these blackouts are similar to syncope and epileptic blackouts, the causes are different.
Experts believe that when people are experiencing a threatening feeling, thought, or memory, it can overwhelm them so much that it induces a seizure.
Some symptoms of psychogenic blackouts include:
- fainting and falling
- jerking movements of the arms and legs
- losing control of the bladder and bowel
- going “blank” and feeling out of touch with the surroundings
- not being able to remember the blackout
Treatment
According to the Epilepsy Society, people who experience psychogenic blackouts may benefit from cognitive behavioral therapy (CBT). CBT helps people identify stressful triggers and put techniques in place to cope when they feel overwhelmed.
Diagnosis
If a person believes that they are experiencing psychogenic blackouts, a doctor may refer them to a neurologist, who may be able to diagnose psychogenic blackouts by ruling out other causes.
Can medication cause blackouts?
According to one 2015 study, vasodilatory medications and diuretics could result in syncope blackouts.
Another 2015 study suggests that overconsuming sedatives could cause memory loss. In one case study, the excessive use of alprazolam (Xanax) led a 50-year-old woman to experience memory loss blackouts. However, more research is necessary to support these findings.
When to see a doctor
A person should speak to a doctor if they believe that they are experiencing symptoms of syncope, epileptic blackouts, or blackouts that are the result of medication. In cases of severe alcohol intoxication, a person may need emergency assistance.
With treatment, most people will be able to continue their daily activities. If a person’s blackouts are related to an underlying medical condition, they should stop once the person receives treatment to manage the condition.
Summary
Excessive alcohol use, stress, medication, and epilepsy can all cause blackouts. While blackouts are a frightening experience, treatment can allow people to lead a normal life without the fear of falling unconscious or losing their memory.

What is the impact of eating too much sugar?
In the short-term, eating too much sugar may contribute to acne, weight gain, and tiredness. In the long-term, too much sugar increases the risk of chronic diseases, such as type 2 diabetes and heart disease.
According to the Centers for Disease Control and Prevention (CDC), people in the United States consume too much added sugar. Added sugars are sugars that manufacturers add to food to sweeten them.
In this article, we look at how much added sugar a person should consume, the symptoms and impact of eating too much sugar, and how someone can reduce their sugar intake.
How much sugar is too much?
According to the Dietary Guidelines for Americans 2010-2015, on average, Americans consume 17 teaspoons (tsp) of added sugar each day. This adds up to 270 calories.
However, the guidelines advise that people limit added sugars to less than 10% of their daily calorie intake. For a daily intake of 2,000 calories, added sugar should account for fewer than 200 calories.
However, in 2015, the World Health Organization (WHO) advised that people eat half this amount, with no more than 5% of their daily calories coming from added sugar. For a diet of 2,000 calories per day, this would amount to 100 calories, or 6 tsp, at the most.
Symptoms of eating too much sugar
Some people experience the following symptoms after consuming sugar:
- Low energy levels: A 2019 study found that 1 hour after sugar consumption, participants felt tired and less alert than a control group.
- Low mood: A 2017 prospective study found that higher sugar intake increased rates of depression and mood disorder in males.
- Bloating: According to Johns Hopkins Medicine, certain types of sugar may cause bloating and gas in people who have digestive conditions, such as irritable bowel syndrome (IBS) or small intestinal bacterial overgrowth (SIBO).
Risks of eating too much sugar
Consuming too much sugar can also contribute to long-term health problems.
Tooth decay
Sugar feeds bacteria that live in the mouth. When bacteria digest the sugar, they create acid as a waste product. This acid can erode tooth enamel, leading to holes or cavities in the teeth.
People who frequently eat sugary foods, particularly in between mealtimes as snacks or in sweetened drinks, are more likely to develop tooth decay, according to Action on Sugar, part of the Wolfson Institute in Preventive Medicine in the United Kingdom.
Acne
A 2018 study of university students in China showed that those who drank sweetened drinks seven times per week or more were more likely to develop moderate or severe acne.
Additionally, a 2019 study suggests that lowering sugar consumption may decrease insulin-like growth factors, androgens, and sebum, all of which may contribute to acne.
Weight gain and obesity
Sugar can affect the hormones in the body that control a person’s weight. The hormone leptin tells the brain a person has had enough to eat. However, according to a 2008 animal study, a diet high in sugar may cause leptin resistance.
This may mean, that over time, a high sugar diet prevents the brain from knowing when a person has eaten enough. However, researchers have yet to test this in humans.
Diabetes and insulin resistance
A 2013 article in PLOS ONE, indicated that high sugar levels in the diet might cause type 2 diabetes over time.
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) add that other risk factors, such as obesity and insulin resistance, can also lead to type 2 diabetes.
Cardiovascular disease
A large prospective study in 2014 found that people who got 17–21% of their daily calories from added sugar had a 38% higher risk of dying from cardiovascular disease (CVD) than those who consumed 8% added sugars. For those who consumed 21% or more of their energy from added sugars, their risk for CVD doubled.
High blood pressure
In a 2011 study, researchers found a link between sugar-sweetened beverages and high blood pressure, or hypertension. A review in Pharmacological Research states that hypertension is a risk factor for CVD. This may mean that sugar exacerbates both conditions.
Cancer
Excess sugar consumption can cause inflammation, oxidative stress, and obesity. These factors influence a person’s risk of developing cancer.
A review of studies in the Annual Review of Nutrition found a 23–200% increased cancer risk with sugary drink consumption. Another study found a 59% increased risk of some cancers in people who consumed sugary drinks and carried weight around their abdomen.
Aging skin
Excess sugar in the diet leads to the formation of advanced glycation end products (AGEs), which play a role in diabetes. However, they also affect collagen formation in the skin.
According to Skin Therapy Letter, there is some evidence to suggest that a high number of AGEs may lead to faster visible aging. However, scientists need to study this in humans more thoroughly to understand the impact of sugar in the aging process.
How to eat less sugar
A person can reduce the amount of added sugar they eat by:
- checking food labels for sweeteners
- reducing foods with added sugar
- avoiding processed foods in general
Checking food labels
Added sugar and sweeteners come in many forms. Ingredients to look out for on a food label include:
- brown sugar
- fructose
- glucose
- sucrose
- maltose
- honey
- corn sweetener
- corn syrup
- high fructose corn syrup
- raw sugar
- molasses
- malt syrup
- evaporated cane juice
- agave nectar
- maple syrup
- invert sugar
- fruit juice concentrates
- trehalose
- turbinado sugar
Some of these ingredients are natural sources of sugar and are not harmful in small amounts. However, when manufacturers add them to food products, a person might easily consume too much sugar without realizing it.
Reducing foods that contain added sugar
Some food products contain large amounts of added sugars. Reducing or removing these foods is an efficient way to reduce the amount of sugar a person eats.
The Dietary Guidelines for Americans 2010–2015 state that soda and other soft drinks account for around half a person’s added sugar intake in the U.S. The average can of soda or fruit punch provides 10 tsp of sugar.
Another common source of sugar is breakfast cereal. According to EWG, many popular cereals contain over 60% sugar by weight, with some store brands containing over 80% sugar. This is especially true of cereals marketed towards children.
Swapping these foods for unsweetened alternatives will help a person lower their sugar intake, for example:
- swapping soda for water, milk, or herbal teas
- swapping sugary cereals for low sugar cereal, oatmeal, or eggs
Avoiding processed foods
Manufacturers often add sugars to foods to make them more appealing. Often, this means people do not realize how much sugar a food contains.
By avoiding processed foods, a person can get a better sense of what their food contains. Cooking whole foods at home also means someone can control what ingredients they put into their meals.
When to see a doctor
People should see their doctor if they experience the symptoms of high blood sugar. According to the NIDDK, symptoms include:
- increased thirst and urination
- increased hunger
- fatigue
- blurred vision
- numbness or tingling in the hands or feet
- unexplained weight loss
- sores that do not heal
These symptoms may indicate a person has diabetes. A doctor can test for diabetes by taking a urine sample.
People should also speak to a doctor if they experience other symptoms after eating sugar, such as bloating.
Summary
Consuming too much added sugar has many adverse impacts on health, including tiredness and weight gain, and more severe conditions, such as heart disease. Added sugars are present in many processed foods and drinks.
People can reduce their sugar intake by knowing what to look for on food labels, avoiding or reducing common sources of sugar, such as soda and cereals, and prioritizing unprocessed whole foods.
If a person is concerned about weight gain, symptoms that may indicate diabetes, or other symptoms they experience after eating sugar, they should speak to a doctor.

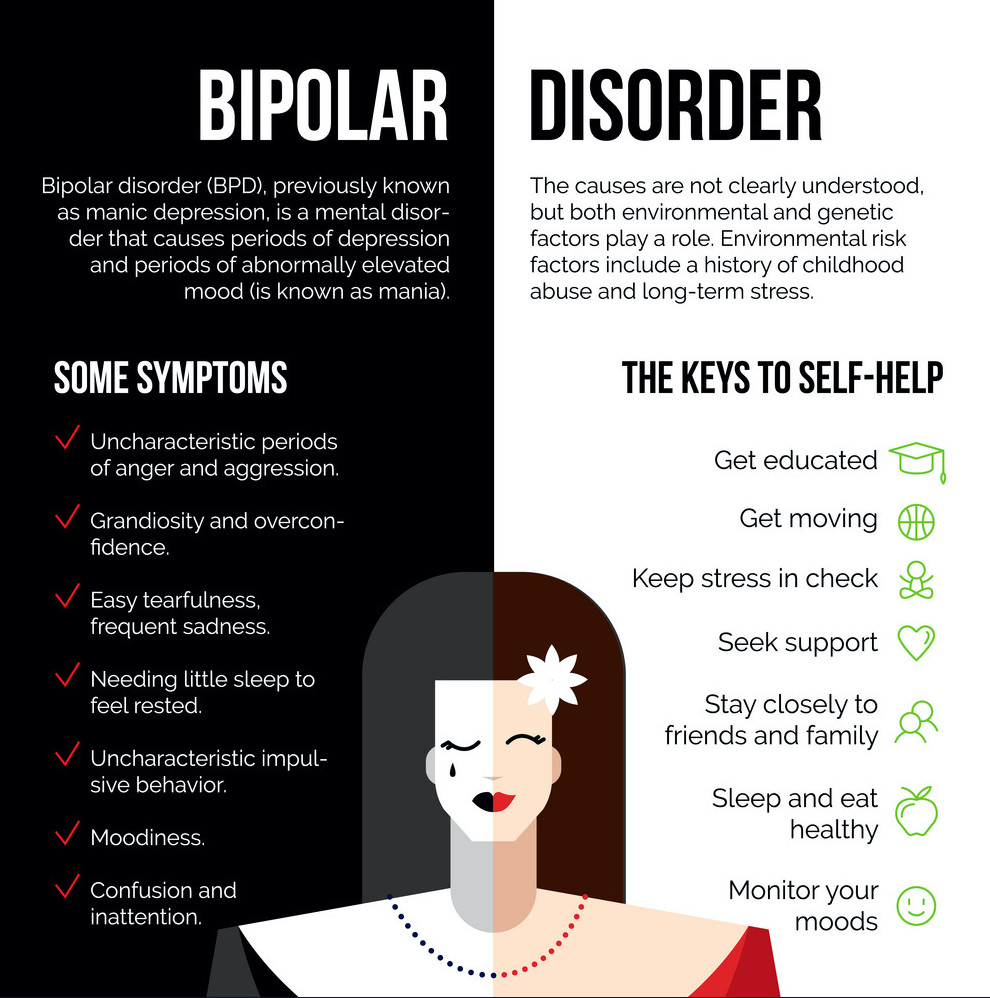
What to know about bipolar disorder?
A person with bipolar disorder will experience changes in mood, energy, and activity levels that can make day-to-day living difficult.
Bipolar disorder can cause severe disruption to a person’s life, but the impact varies between individuals. With appropriate treatment and support, many people with this condition live a full and productive life.
According to the National Alliance on Mental Illness (NAMI), bipolar disorder affects over 10 million people in the United States or around 2.8% of the population.
On average, a person will receive a diagnosis around the age of 25 years, but symptoms can appear during the teenage years or later in life. It affects males and females equally.
What is bipolar disorder?
The National Institute of Mental Health describe the main symptoms of bipolar disorder as alternating episodes of high and low mood. Changes in energy levels, sleep patterns, ability to focus, and other features can dramatically impact a person’s behavior, work, relationships, and other aspects of life.
Most people experience mood changes at some time, but those related to bipolar disorder are more intense than regular mood changes, and other symptoms can occur. Some people experience psychosis, which can include delusions, hallucinations, and paranoia.
Between episodes, the person’s mood may be stable for months or years, especially if they are following a treatment plan.
Treatment enables many people with bipolar disorder to work, study, and live a full and productive life. However, when treatment helps a person feel better, they may stop taking their medication. Then, the symptoms can return.
Some aspects of bipolar disorder can make a person feel good. During an elevated mood, they may find they are more sociable, talkative, and creative.
However, an elevated mood is unlikely to persist. Even if it does, it may be hard to sustain attention or follow through with plans. This can make it difficult to follow a project through to the end.
Symptoms
According to the International Bipolar Association, symptoms vary between individuals. For some people, an episode can last for several months or years. Others may experience “highs” and “lows” at the same time or in quick succession.
In “rapid cycling” bipolar disorder, the person will have four or more episodes within a year.
Mania or hypomania
Hypomania and mania are elevated moods. Mania is more intense than hypomania.
Symptoms can include:
- impaired judgment
- feeing wired
- sleeping little but not feeling tired
- a sense of distraction or boredom
- missing work or school
- underperforming at work or school
- feeling able to do anything
- being sociable and forthcoming, sometimes aggressively so
- engaging in risky behavior
- increased libido
- feeling exhilarated or euphoric
- having high levels of self-confidence, self-esteem, and self-importance
- talking a lot and rapidly
- jumping from one topic to another in conversation
- having “racing” thoughts that come and go quickly, and bizarre ideas that the person may act upon
- denying or not realizing that anything is wrong
Some people with bipolar disorder may spend a lot of money, use recreational drugs, consume alcohol, and participate in dangerous and inappropriate activities.
Depressive symptoms
During an episode of bipolar depression, a person may experience:
- a feeling of gloom, despair, and hopelessness
- extreme sadness
- insomnia and sleeping problems
- anxiety about minor issues
- pain or physical problems that do not respond to treatment
- a sense of guilt, which may be misplaced
- eating more or eating less
- weight loss or weight gain
- extreme tiredness, fatigue, and listlessness
- an inability to enjoy activities or interests that usually give pleasure
- difficulty focusing and remembering
- irritability
- sensitivity to noises, smells, and other things that others may not notice
- an inability to face going to work or school, possibly leading to underperformance
In severe cases, the individual may think about ending their life, and they may act on those thoughts.
Psychosis
If a “high” or “low” episode is very intense, the person may experience psychosis. They may have trouble differentiating between fantasy and reality.
According to the International Bipolar Foundation, psychosis symptoms during a high include hallucinations, which involve hearing or seeing things that are not there and delusions, which are false but strongly felt beliefs. A person who experiences delusions may believe they are famous, have high-ranking social connections, or have special powers.
During a depressive or “low” episode, they may believe they have committed a crime or are ruined and penniless.
It is possible to manage all these symptoms with appropriate treatment.
Types of bipolar disorder
A person may receive a diagnosis of one of three broad types of bipolar disorder. According to NAMI, symptoms occur on a spectrum, and the distinction between the types is not always clear-cut.
Bipolar I disorder
For a diagnosis of bipolar I disorder:
- The individual must have experienced at least one manic episode.
- The person may have had a previous major depressive episode.
- The doctor must rule out other disorders, such as schizophrenia and delusional disorder.
Bipolar II disorder
Bipolar II disorder involves periods of hypomania, but depression is often the dominant state.
For a diagnosis of bipolar II disorder, a person must have had:
- one or more episodes of depression
- at least one hypomanic episode
- no other diagnosis to explain the mood shifts
A person with hypomania may feel good and function well, but their mood will not be stable, and there is a risk that depression will follow.
People sometimes think of bipolar II disorder as a milder version. For many, however, it is simply different. As NAMI indicate, people with bipolar II disorder may experience more frequent episodes of depression than people with bipolar I disorder.
Cyclothymia
The National Health Service (NHS) in the United Kingdom note that cyclothymia has similar features to bipolar disorder, but the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) classifies it separately. It involves hypomania and depression, but the changes are less intense.
Nevertheless, cyclothymia can impact a person’s daily life, and a doctor can provide treatment.
Diagnosis
A medical professional will diagnose bipolar disorder using criteria set out in the DSM-5.
The National Institue of Mental Health (NIMH) explain that in order to receive a diagnosis of bipolar I disorder, a person must have had symptoms for at least 7 days, or less if symptoms were severe enough to need hospitalization. They may also have had a depressive episode lasting at least 2 weeks.
To receive a diagnosis of bipolar II, a person will have experienced at least one cycle of hypomania and depression.
A doctor may carry out a physical examination and some diagnostic tests, including blood and urine tests, to help rule out other causes.
It can be challenging for a doctor to diagnose bipolar disorder, as people are more likely to seek help with a low mood than a high mood. As a result, it can be hard for them to distinguish it from depression.
If the person has psychosis, a doctor may misdiagnose their condition as schizophrenia.
Other complications that may occur with bipolar disorder are:
- use of drugs or alcohol to cope with symptoms
- post-traumatic stress disorder (PTSD)
- anxiety disorder
- attention-deficit hyperactivity disorder (ADHD)
NIMH urge healthcare providers to look for signs of mania in the person’s history, to prevent misdiagnosis. Some antidepressants can trigger mania in susceptible people.
A person who receives a diagnosis of bipolar disorder has a lifelong diagnosis. They may enjoy long periods of stability, but they will always live with the condition.
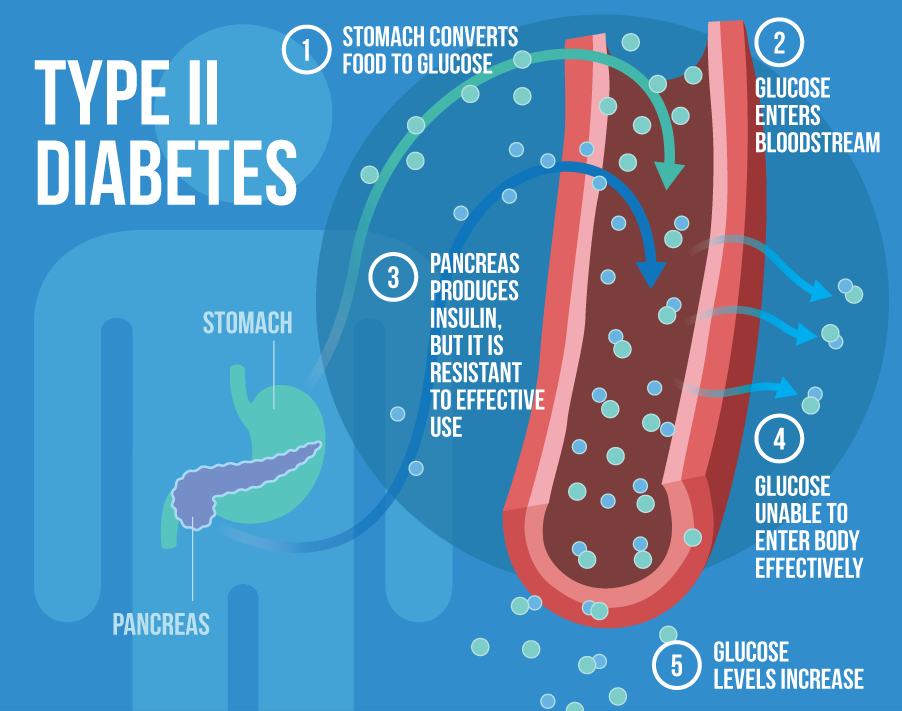
What are the symptoms of type 2 diabetes?
Type 2 diabetes is the most common form of diabetes. It happens when blood sugar levels rise due to problems with the use or production of insulin.
It can appear at any age, but it is more likely to occur after the age of 45 years.
It affects over 30 million Americans, according to the United States Centers for Disease Control and Prevention (CDC), and it accounts for 90–95 percent of diabetes cases.
What is type 2 diabetes?
People with type 2 diabetes do not make or use insulin correctly.
Insulin is a hormone that regulates the movement of blood glucose, or sugar, into cells, which use it as energy.
When sugar cannot enter cells, this means:
- too much glucose collects in the blood
- the body’s cells cannot use it for energy
A doctor may diagnose diabetes if a person’s blood sugar levels are 126 milligrams per deciliter (mg/dl) or above after fasting for 8 hours.
Symptoms
The symptoms of high blood sugar in type 2 diabetes tend to appear gradually. Not everyone with type 2 diabetes will notice symptoms in the early stages.
If a person does experience symptoms, they may notice the following:
- Frequent urination and increased thirst: When excess glucose builds up in the bloodstream, the body will extract fluid from tissues. This can lead to excessive thirst and the need to drink and urinate more.
- Increased hunger: In type 2 diabetes, the cells are not able to access glucose for energy. The muscles and organs will be low on energy, and the person may feel more hungry than usual.
- Weight loss: When there is too little insulin, the body may start burning fat and muscle for energy. This causes weight loss.
- Fatigue: When cells lack glucose, the body becomes tired. Fatigue can interfere with daily life when a person has type 2 diabetes.
- Blurred vision: High blood glucose can cause fluid to be pulled from the lenses of the eyes, resulting in swelling, leading to temporarily blurred vision.
- Infections and sores: It takes longer to recover from infections and sores because blood circulation is poor and there may be other nutritional deficits.
If people notice these symptoms, they should see a doctor. Diabetes can lead to a number of serious complications. The sooner a person starts to manage their glucose levels, the better chance they have of preventing complications.
Symptoms in children and teens
Type 2 diabetes is more likely to appear after the age of 45 years, but it can affect children and teens who:
- have excess weight
- do not do much physical activity
- have high blood pressure
- have a family history of type 2 diabetes
- have an African American, Asian American, Hispanic American, or American Indian background
The following symptoms may occur:
- weight loss, despite increased appetite and hunger
- extreme thirst and dry mouth
- frequent urination and urinary tract infections
- fatigue
- blurred vision
- slow healing of cuts or wounds
- numbness or tingling in hands and feet
- itchy skin
If caregivers notice these symptoms, they should take the child to see a doctor. These are also symptoms of type 1 diabetes. Type 1 is less common but more likely to affect children and teenagers than adults. However, type 2 diabetes is becoming more common in young people than it was in the past.
Symptoms in older adults
At least 25.2 percent of people aged 65 and above have type 2 diabetes in the United States. They may have some or all the classic symptoms of type 2 diabetes.
They may also experience one or more of the following:
- flu-like fatigue, which includes feeling lethargic and chronically weak
- urinary tract infections
- numbness and tingling in the hands, arms, legs, and feet due to circulation and nerve damage
- dental problems, including infections of the mouth and red, inflamed gums
Early signs
Most people do not experience symptoms in the early stages, and they may not have symptoms for many years.
A possible early sign of type 2 diabetes is darkened skin on certain areas of the body, including:
- the neck
- the elbows
- the knees
- the knuckles
This is known as acanthosis nigricans.
Other early symptoms include:
- frequent bladder, kidney, or skin infections
- cuts that take longer to heal
- fatigue
- extreme hunger
- increased thirst
- urinary frequency
- blurred vision
A person may have mild or subtle symptoms for many years, but these can become in time. Further health problems can develop.
Prediabetes and diabetes prevention
A person with blood sugar levels of 100–125 mg/dl will receive a diagnosis of prediabetes. This means that their blood sugar levels are high, but they do not have diabetes. Taking action at this stage can prevent diabetes from developing.
According to a 2016 report published in The Journal of the American Board of Family Medicine, 33.6 percent of people aged 45 years and older had prediabetes in 2012.
The CDC estimate that around 84 million American adults have prediabetes, but most do not know they have it.
Complications
Diabetes may cause a number of health complications if people do not manage it properly. Many of these are chronic, or long-term, but they can become life-threatening. Others need immediate medical attention as soon as they appear.
Emergency complications
Complications can arise quickly if blood sugar rises or falls too far.
Hypoglycemia
If blood glucose dips below 70 mg/dl, this is hypoglycemia, or low blood sugar.
This can happen if a person who uses insulin takes more than they need for a particular time.
A home blood glucose test can check for hypoglycemia.
It is vital to know the early signs of hypoglycemia, as it can progress quickly, resulting in seizures and a coma. In the early stages, however, it is easy to treat.
Symptoms of hypoglycemia include:
- confusion
- dizziness
- feeling faint
- heart palpitations
- rapid heartbeat
- mood changes
- loss of consciousness
- sweating
- clamminess
If symptoms are mild, a person can often resolve low blood sugar levels by consuming:
- a few pieces of hard candy
- a cup of orange juice
- a teaspoon of honey
- a glucose tablet
The person should then wait 15 minutes, test their blood sugar, and if it is still low, they should take another glucose tablet or sweet.
When levels return to above 70 mg/dl, the person should eat a meal, to stabilize their glucose levels.
If they remain low for 1 hour or longer, or if symptoms worsen, someone should take the person to the emergency room.
Anyone who has frequent or severe hypoglycemic episodes should speak to their doctor, as they may need to adjust their treatment plan.
Hyperglycemia and diabetic ketoacidosis (DKA)
If blood sugar levels rise too far, hyperglycemia can result. If a person notices increased thirst and urination, they should check their blood sugar levels.
It the level is above the target level that their doctor recomends, they take appropriate action.
Without treatment, high a person with hyperglycemia can develop diabetic ketoacidosis (DKA), which happens when high levels of ketones collect in the blood, making it too acidic. For this reason, the person should also test their ketone levels.
Ketoacidosis can lead to:
- difficulty breathing
- a fruity smell on the breath
- a dry mouth
- nausea and vomiting
- coma
It can be life-threatening. A person with these signs and symptoms should seek immediate medical attention.
People who regularly experience high blood sugar should speak to their doctor about adjusting their treatment plan.
People should check with their doctor how often they need to test.
Long-term complications
Keeping blood glucose within target levels can prevent complications that can become life-threatening and disabling over time.
Some possible complications of diabetes are:
- heart and blood vessel diseases
- high blood pressure
- nerve damage (neuropathy)
- foot damage
- eye damage and blindness
- kidney disease
- hearing problems
- skin problems
Effective management of blood glucose levels can reduce the risk of complications.
Diagnosis and treatment
A doctor can diagnose type 2 diabetes with blood tests that measure blood glucose levels. Many people discover they have high blood sugar during a routine screening test, but anyone who experiences symptoms should see a doctor.
Treatment aims to keep blood glucose levels stable at a healthy level and prevent complications. The main ways to do this are through lifestyle measures.
These include:
- following a healthful diet
- reaching and maintaining a healthy weight and body mass index (BMI)
- doing physical activity
- getting enough sleep
- avoiding or quitting smoking
- taking medications or insulin as the doctor recommends
Outlook
There is currently no cure for diabetes, but most people with the condition can lead a healthful life by managing their condition properly.
People who maintain a healthy weight, follow a healthful diet, and do regular exercise may not need medication. Taking these steps can help manage blood sugar levels.
Routine screening can alert a person to high blood sugar levels in the early stages, when there is still time to slow, stop, or reverse the progress of diabetes.
Current guidelines recommend regular screening from the age of 45 years, or younger if an individual has other risk factors, such as obesity. A doctor can advise on individual needs.
It is important to have support from people who understand what it is like to receive a diagnosis and live with type 2 diabetes.
What is shingles?
Shingles is a viral infection that results from the varicella-zoster virus (VZV), the same virus that causes chickenpox. It typically affects a single sensory nerve ganglion and the skin surface that the nerve supplies.
Anyone who has had chickenpox can later develop shingles.
In fact, according to the Centers for Disease Control and Prevention (CDC), an estimated 1 in 3 people in the United States develop shingles during their lifetime.
However, a person can only develop shingles if they have had chickenpox or exposure to the virus that causes it. This virus can lie dormant for years.
Most adults with the dormant virus never develop shingles, but for some, the virus reactivates several times.
Shingles is most common after the age of 50 years, but it can appear at any age if a person has previously had chickenpox.
In this article, learn more about shingles, including symptoms, complications, and treatments.
Symptoms
Shingles usually affects one side of the body. This is most often the waist, chest, abdomen, or back. Symptoms can also appear on the face and in the eyes, mouth, ears. The virus can also affect some internal organs.
Shingles typically affects a single sensory nerve ganglion near the spinal cord, called a dorsal root ganglion. This is why the symptoms occur in specific areas of the body, rather than all over it. The pain results from nerve involvement, rather than the rash itself.
In fact, some people have pain but no rash. Others, meanwhile, may have a rash with pain that is accompanied by other symptoms, such as fever, chills, or headache.
Symptoms can vary in nature, depending on where on the body they appear.
Common symptoms
Some of the most common symptoms of shingles include:
- a constant dull, burning, or gnawing pain, or a sharp, stabbing pain that comes and goes
- a skin rash that resembles a chickenpox rash but only affects certain areas
- fluid-filled blisters that develop as part of the rash
Symptoms on the body
A blistering skin rash may appear in one or more distinct bands with sensory nerves of the skin, called dermatomes.
Common locations for this include:
- the chest
- the abdomen
- the back
- around the waist
It usually occurs only on one side of the body.
The location of the symptoms will depend on which dermatome distribution the virus affects.
Facial symptoms
If the rash affects the face, symptoms usually appear on one side only — usually around one eye and the forehead.
They can include:
- pain over the affected dermatome
- a rash
- muscle weakness
- headache
Eye symptoms
If the virus affects an ophthalmic nerve, it means that a person has herpes zoster ophthalmicus.
This can cause pain, redness, and swelling in and around the eye, as well as temporary or permanent loss of vision.
Ear symptoms
Shingles can also occur in or around the ear, leading to problems with balance and hearing, as well as muscle weakness on the affected side of the face.
These changes can be long term or even permanent. A person who develops symptoms in or around the ears and eyes should seek immediate medical attention to reduce the risk of complications.
Mouth symptoms
If shingles affects the mouth, a person may experience:
- facial tenderness
- pain in the mouth
- toothache
- lesions in hard and soft palate tissues
The pain and discomfort of these symptoms can make it difficult to eat or drink.
Internal shingles
Shingles can also affect the internal organs. There will not be a rash, but other problems can arise.
For example, researchers have found evidence of shingles in the digestive system, which can lead to gastrointestinal dysfunction, and in the arteries in the brain, which may increase the risk of stroke and dementia.
Other symptoms
There may also be other symptoms, including:
- fever
- fatigue
- chills
- headache
- upset stomach
Symptom progression
Symptoms typically progress as follows:
- Pain, tingling, numbness, and itching start to affect a specific part of the skin.
- After up to 2 weeks, a rash appears.
- Red blotches and itchy, fluid-filled blisters develop and continue to do so for 3-5 days.
- The blisters may merge, forming a solid red band that looks similar to a severe burn. The gentlest touch may be painful.
- Inflammation may affect the soft tissue under and around the rash.
- After 7–10 days, the blisters gradually dry up and form scabs or crusts. As the blisters disappear, they may leave minor scarring.
Shingles usually lasts around 2–4 weeks. It is contagious until the blisters dry up and crust over.
Most people will only have an episode of shingles once, but it can recur in some people.
Complications
Rarely, complications can arise — especially in people with an impaired immune system.
Possible complications of shingles include:
- postherpetic neuralgia (PHN)
- inflammation of the brain or spinal cord, increasing the risk of stroke, encephalitis, and meningitis
- eye and vision problems
- weakness
- problems with balance and hearing
- damage to blood vessels, which could lead to stroke
- pneumonia
According to the CDC, around 10–18% of people who have shingles will develop PHN, a long term complication wherein the pain of a shingles rash lasts long beyond the rash itself.
It is more likely to occur if a person develops shingles after the age of 40 years, and the risk continues to increase with age.
In people with weak immune systems
People with a weakened immune system will have a higher risk of developing shingles and of experiencing severe symptoms and complications.
This include people who:
- have cancer, especially leukemia or lymphoma
- have HIV
- have undergone an organ transplant
- are taking medications to suppress the immune system, including chemotherapy drugs
These people should seek medical attention as soon as possible if they have concerns about shingles-related symptoms.
Is shingles contagious?
It is not possible to directly transmit shingles to another person. However, a person who has never had chickenpox can contract VZV by coming into direct contact with the fluid in the blisters of a person who currently has shingles.
If this happens and the person has not received vaccination against chickenpox, they would develop chickenpox first, not shingles.
Shingles does not spread through coughing or sneezing. Only direct contact with fluid from the blisters can spread the virus. Therefore, covering the blisters reduces the risk of contagion.
It is important to note that the virus is only active from when the blisters first appear to when they dry up and crust over. Transmission is not possible before the blisters develop and after the crusts form. If a person does not develop blisters, the virus cannot spread in the traditional sense.
Taking the following precautions can help prevent the transmission of the virus:
- Cover the rash.
- Wash the hands often.
- Avoid touching or scratching the rash.
It is also important to avoid contact with:
- infants who are preterm or have a low birth weight
- pregnant women who have never had chickenpox or the vaccine for it
- those with a weakened immune system
Treatment
A doctor may prescribe antiviral drugs to stop the virus from multiplying.
Antiviral treatment
Antiviral treatment can help:
- reduce the severity and duration of symptoms
- prevent complications from developing
- lower the risk of the rash coming back
Managing symptoms
Tips for managing symptoms include:
- using pain relief medication
- reducing stress as much as possible
- eating regular, nutritious meals
- getting some gentle exercise
- wearing loose fitting clothes, for comfort
To relieve itching, the CDC recommend:
- applying calamine lotion
- taking a lukewarm, oatmeal bath
- placing a cool, damp washcloth on the blisters
Most people will recover with home treatment, but a person should seek medical help if other symptoms appear, such as a fever. Around 1–4% of people will need to spend time in the hospital due to complications.

