Cardiovascular health most important to reduce diabetes risk
- A recent study investigated the effects of good cardiovascular health (CVH) in preventing type 2 diabetes (T2D) among middle-aged individuals.
- The results suggest that middle-aged adults with a healthy heart have a reduced risk of developing T2D.
- The study also notes that regardless of genetic predisposition, favorable CVH reduces the risk of developing T2D among middle-aged individuals.
The Centers for Disease Control and Prevention (CDC)Trusted Source estimate that more than 34 million people in the United States live with diabetes and that approximately 90–95% of these individuals have T2D.
T2D is characterized by peripheral resistance to insulin. This means that tissues such as the gut, liver, and muscles fail to respond to messages from insulin to take up glucose from the bloodstream.
It also means that the liver, which not only absorbs glucose but also produces it, does not respond to insulin to stop this production. In the early stages, the pancreas secretes additional insulin to overcome the problem, but this corrective process can eventually fail.
Insulin is a hormone that the pancreas produces. It regulates the transport of glucose into the cells of the body, where it serves as a source of energy. Blood glucose levels that remain too high for long periods can damage various organs and systems of the body.
Previous research has shown that multiple factors — both genetic and nongenetic — combine to increase a person’s risk of developing T2D. However, there is also evidence showing that people can significantly reduce this risk by adopting certain lifestyle measures.
Recently, scientists in the Netherlands embarked on a study to evaluate whether a favorable CVH score reduces the lifetime risk of developing T2D. They looked at middle-aged individuals with and without a genetic predisposition to T2D.
The results appear in the European Journal of Preventive Cardiology.
Measuring cardiovascular health
Lead study author Dr. Fariba Ahmadizar, Ph.D., a professor at the Erasmus University Medical Center in the Netherlands, explained the motivation behind the study to Medical News Today:
“Previous studies have shown that cardiovascular risk factors are largely associated with the risk for T2D.”
“However, data on the lifetime risk of incident T2D across different CVH categories was scarce,” she added. “More importantly, the impact of genetic predisposition on the lifetime risk of incident T2D associated with CVH was unknown, [so] this prompted our research into cardiovascular health, genetic predisposition, and lifetime risk of T2D.”
The new study included 5,993 participants without T2D at the start of the study. Data came from the Rotterdam Study — a prospective cohort study of a community-dwelling population aged 55 years and older in Rotterdam.
The average age of the participants was 69 years, and 58% were women. The study participants received CVH scores based on a range of parameters that the scientists measured at baseline. These included body mass index (BMI), smoking behavior, blood pressure, total cholesterol, physical activity, and diet.
The researchers summed up these parameters to create a CVH score between 0 and 12, with higher scores indicating better CVH. Based on the CVH score, they divided the participants into three groups: poor, intermediate, and ideal.
In addition, the team calculated biological CVH, which comprised blood pressure, total cholesterol, and smoking.
Each participant also received a behavioral CVH score, which took into account BMI, smoking, diet, and physical activity.
In assessing genetic predisposition to T2D, the researchers used 403 independent genetic variants associated with the disease to generate a genetic risk score. They used this score to classify the participants as having a low, intermediate, or high genetic risk.
Analyzing the study results
The researchers noted that at 55 years, the lifetime risk of developing T2D varied by CVH score:
- ideal: 22.6%
- intermediate: 28.3%
- poor: 32.6%
When they accounted for genetic risk, the researchers observed that among those in the high genetic risk group, the lifetime risk of T2D was 23.5%, 33.7%, and 38.7% for the ideal, intermediate, and poor CVH groups, respectively.
In comparison with the poor and intermediate CVH groups, the ideal CVH group still had the lowest lifetime risk for T2D, although this pertained to those with an intermediate or low genetic risk.
The scientists also assessed the lifetime risk of T2D using behavioral and biological scores. They noted that for both the behavioral and biological assessments, the risk was lower in the ideal CVH groups than in the poor and intermediate groups.
These findings led the researchers to conclude that, regardless of genetic predisposition, favorable CVH health is most important in preventing T2D among middle-aged individuals.
This conclusion is similar to the sentiments that Dr. Francesca Cortese — a cardiologist in Bari University General Hospital, Italy — has shared. Dr. Cortese says:
“Through very simple tools, such as education for a correct lifestyle, we can significantly contribute to the prevention of T2D and its complications.”
Study limitations and controversy
The authors acknowledge that the study had limitations. Firstly, the team obtained individual CVH parameters at baseline, which was 20–27 years earlier. This could have led to misclassification of the participants across the different categories in the intervening time.
Secondly, some results from the genetic groups were based on relatively small sample sizes, which means that further information may be required.
Lastly, most of the participants were of European ancestry, limiting the generalizability of the results to other populations.
Also, in a potentially contentious twist, the scientists noted that participants decreased their lifetime T2D risk further by adhering to an ideal behavioral CVH rather than an ideal biological CVH. One of the components in the behavioral score was BMI.
As the authors explain, “This is controversial because it may suggest that obesity is a choice.” However, other research underlining the multifactorial nature of obesity concludes that people should consider obesity a health metric just as they would blood pressure or T2D.
Regardless of the study’s limitations and controversy, it has opened up interesting possibilities on which future studies can build.
Medical Myths: 15 breast cancer misconceptions
In 2020, 685,000 people died from breast cancer, and 2.3 million received a diagnosis. It reported:
“As of the end of 2020, there were 7.8 million women alive who were diagnosed with breast cancer in the past 5 years, making it the world’s most prevalent cancer.”
Its prevalence might help explain why there is a wide range of myths attached to it. Here, we will tackle 15 of the most common misunderstandings.
To help us reach the truth, we enlisted the help of three experts:
- Dr. Michael Zeidman: an assistant professor of breast surgery at Icahn School of Medicine at Mount Sinai in New York City.
- Dr. Crystal Fancher: a surgical breast oncologist at the Margie Petersen Breast Center at Providence Saint John’s Health Center and assistant professor of surgery at the Saint John’s Cancer Institute in Santa Monica, CA.
- Dr. Richard Reitherman, Ph.D.: the medical director of breast imaging at MemorialCare Breast Center at Orange Coast Medical Center in Fountain Valley, CA.
1. A breast injury can cause breast cancer
“Injury to the breast cannot cause breast cancer,” explained Dr. Zeidman, “however, it can cause changes in the breast that may mimic breast cancer on imaging.”
“This process is called ‘fat necrosis,” he continued, “and it can look like an irregular mass with jagged edges on a mammogram, much like the appearance of a new breast cancer. The best way to distinguish cancer from fat necrosis is with a needle biopsy.”
2. Underwire bras increase the risk of breast cancer
Although underwire bras do not increase breast cancer risk, Dr. Zeidman always recommends bras without a wire. He explains:
“The wire can irritate the skin under the breast, which can lead to skin breakdown. This breakdown may allow bacteria to enter the breast causing infection, [an] abscess, [or both].”
3. IVF increases the risk of breast cancer
As part of the in vitro fertilization (IVF) procedure, doctors often prescribe drugs that stimulate the ovaries to produce eggs. These drugs mimic the activity of estrogen.
Because of this, some experts wondered whether they might encourage the growth of estrogen receptor-positive breast cancer. As the name suggests, these cancer cells have estrogen receptors on their membranes.
“While there are no randomized controlled trials looking to answer this question,” explained Dr. Zeidman, “a recent meta-analysis of all observational studies over the past 30 years concluded that there is no increase in breast cancer risk for women who received ovarian stimulation drugs compared with the general population.”
4. No one in my family had breast cancer, so I won’t develop it
This is a myth that Dr. Zeidman is familiar with, he told Medical News Today: “It is very common for [people] with a new breast cancer diagnosis to tell me how shocked they are considering that they have no family history.”
“I then respond by stating that the vast majority of [people who] I see with a new breast cancer have no risk factors. In fact, the most significant risk factor for developing breast cancer is being a woman. In the United States, 1 in 8 women will develop breast cancer over their lifetime.”
As Dr. Fancher explained to us, “only about 5–10% of breast cancers are caused by a genetic mutation that is passed between family members. This means that the majority of breast cancers are sporadic or have no hereditary cause.”
Because family history is only one factor in the risk of breast cancer, screening is important. As Dr. Reitherman explained:
“The message is that every woman starting at 40 years of age should have a yearly mammogram regardless of a family history of breast cancer. Those women with a family history of breast or ovarian cancer should be evaluated by a genetics counselor by the age of 30. This group of women may need to begin breast cancer screening prior to the age of 40.”
Dr. Zeidman takes the opportunity to stress the importance of checkups:
“If you are a woman and at least 40 years old, please get your screening mammograms!”
5. Being stressed can cause breast cancer
With the ever-present stresses of modern life, it is no surprise that people are concerned about how stress might impact health.
However, as Dr. Zeidman told us, “There is absolutely no evidence to support a link between stress and breast cancer. In fact, there is evidence to support that stress does not increase breast cancer risk.”
That is not to say that stress cannot impact health at all, however. He goes on: “Part of being human is finding effective ways to deal with the stress we all will inevitably face. This can have profound health benefits both mentally and physically, but will do nothing to mitigate breast cancer risk.”
6. A healthy lifestyle eliminates breast cancer risk
“While it is true that postmenopausal women who are overweight are at an increased risk of developing breast cancer, there is nothing that a woman can do to eliminate breast cancer risk,” explained Dr. Zeidman.
“Even women who undergo bilateral mastectomy are still at risk of developing a new breast cancer.”
However, he is not suggesting anyone starts “smoking and eating fast food every day.”
More generally, he believes that “it is of the utmost importance to take care of your body because you only get one. But even world class athletes have been diagnosed with breast cancer.”
7. Breast cancer only happens to older adults
“While it is true that breast cancer risk increases as women age, and the average age of a new breast cancer diagnosis is 61 years, breast cancer can occur much earlier,” Dr. Zeidman told MNT.
“About 5% of new breast cancer diagnoses are in women under the age of 40 years. There, unfortunately, have been reports of women in their early 20s and even teens who were diagnosed. There is typically a strong family history in these young women.”
“If you have a significant lifetime breast cancer risk based on a strong family history, then you may qualify for genetic testing and early screening starting at age 25.”
Dr. Fancher explains that, although breast cancer is rarer in younger people, she encourages people to “bring any concerning findings in your breast to your doctor’s attention and follow their recommended screening guidelines.”
8. All lumps in the breast signal breast cancer
This is a myth — not all lumps in the breast are cancer. Dr. Zeidman explained that the majority
“of new breast lumps are benign. And, if you had a recent mammogram that was normal, then that percentage is likely even higher.”
However, Dr. Zeidman made it clear that any new lump should be “evaluated by a healthcare professional.”
9. Having an abortion increases the risk of breast cancer
“The reason this question comes up is because we know that breast cancer risk is directly related to estrogen exposure,” Dr. Zeidman told us, “and abortion interrupts the normal hormonal cycle of pregnancy.”
“While we can never perform a randomized controlled trial to address this question, there was a very large observational study
in Denmark that included 1.5 million women and found no link between abortion and breast cancer.”
Aside from this analysis, he explained that there have also “been several other large-scale studies that came to the same conclusion.”
10. Carrying a phone in your bra can cause cancer
According to Dr. Zeidman: “There is no evidence to support that cell phones cause cancer, period.”
“However, we do not have any long-term studies, so we may find this to be the case in the future. For now, why can’t you just put your phone in your pocket or bag?”
11. Nipple piercings increase breast cancer risk
Dr. Zeidman told MNT that this is a myth — nipple piercings do not increase breast cancer risk.
“However,” he elaborated, “they can lead to complications, such as infection, abscess, difficulty breastfeeding due to blocked ducts from scar tissue, nerve damage, keloids, cysts, and more rare but serious illness from HIV and hepatitis B and C.”
“For these reasons,” he said, “I always recommend against nipple piercing. If the deed is done, I recommend removing it.”
12. Sugar causes breast cancer
Dr. Zeidman maintains a firm stance on sugar: “Sugar should be avoided in general. It is addictive.”
“It can cause mood swings,” he continued, “It leads to spikes in insulin, which puts the body in a pro-inflammatory state. This, in turn, can lead to heart disease, diabetes, and other chronic inflammatory diseases.”
“Too much sugar can result in obesity, which is a risk factor for breast cancer.”
However, he explained that studies investigating links between sugar and breast cancer have been “mixed and inconsistent.”
While discussing sugar, it is worth busting a related myth: that sugar helps tumors grow. This myth arose because cancer cells divide rapidly and, therefore, need a lot of energy.
“While there is no concrete evidence to support this,” stated Dr. Zeidman, “I still recommend abstaining from added sugar as much as possible for overall well-being.”
13. Men do not get breast cancer
“Men have breasts… so yes, they too get breast cancer,” said Dr. Zeidman. “In fact, 1%
of all breast cancer diagnoses in the U.S. are in men.”
According to the Centers for Disease Control and Prevention (CDC), there were 2,300 new cases of male breast cancer in 2017 and 500 deaths.
“While breast cancer is more common in women than men, there are still men who get breast cancer,” explained Dr. Fancher, “It’s important for men also to be aware of any changes in their breast since there are no recommended screening guidelines for men.”
“Any lump, pain, or changes should be brought to your doctor’s attention, even if you don’t have a strong family history.”
– Dr. Fancher
Dr. Reitherman added, “Men are diagnosed with breast cancer rarely the most common risk factor is a family history of breast cancer. The BRCA2
genetic mutation markedly increased the risk of breast cancer in males who carry this gene.”
14. Mammograms cause breast cancer to spread
“This is a common misconception that I hear from my patients,” Dr. Zeidman told us.
“The thinking is that squeezing the cancer with compression during mammography, or performing a needle biopsy on the cancer, will cause the cancer to seed other parts of the breast.” However, he confirms:
“There is absolutely no evidence to support this.”
Dr. Reitherman agrees: “There is absolutely no evidence that mammograms cause breast cancer. The performance of a mammogram uses a very low dose of radiation and compression and has no documented or theoretical relationship to causing breast cancer.”
15. If there is no lump, there is no cancer
“If this were true, then we would not need mammograms,” said Dr. Zeidman. “Mammograms have been proven to save lives because they allow us to catch the cancer before it becomes palpable,”
In this context, “palpable” means that a person can feel the lump with their fingers.
“If we diagnose and treat a breast cancer while it is stage 1, survival approaches 100%. Survival drops as the stage advances. In fact, the cancer may never be palpable and still spread to other parts of the body,” Dr. Zeidman added.
According to Dr. Fancher, “Many breast cancers are found on screening mammograms and may not be felt. This is especially true for noninvasive breast cancer or ductal carcinoma in situ, which may only show up as calcifications on a screening mammogram.”
The take-home
Breast cancer is common, and while a healthy lifestyle might reduce the risk to a certain extent, vigilance is key. The earlier a doctor catches breast cancer, the higher the chances of surviving it.
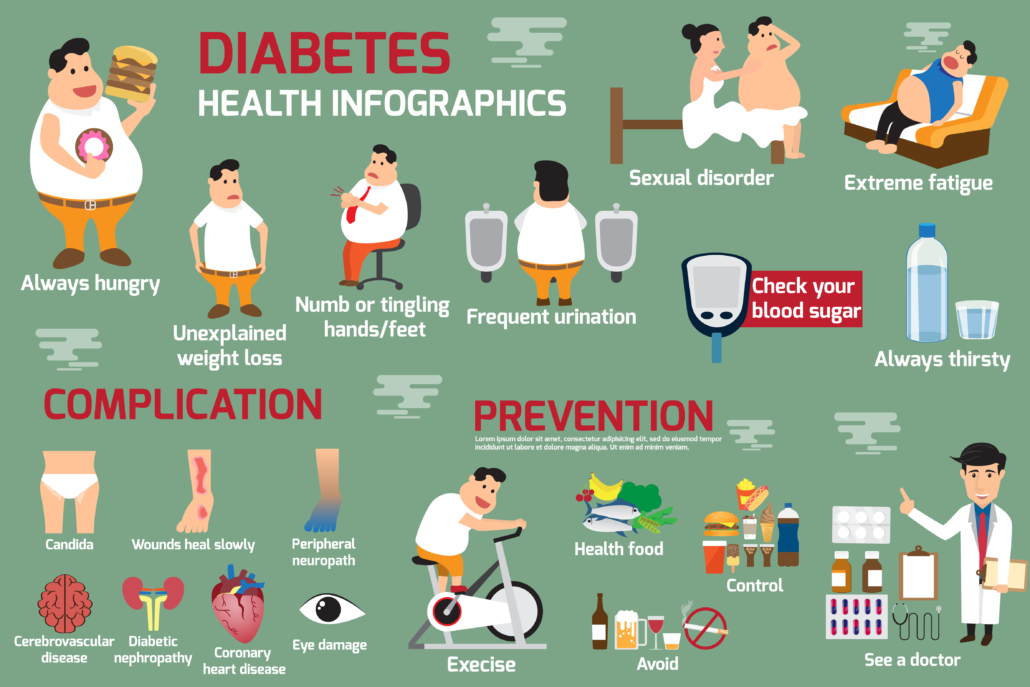
What are the symptoms of type 2 diabetes?
Type 2 diabetes is the most common form of diabetes. It happens when blood sugar levels rise due to problems with the use or production of insulin.
It can appear at any age, but it is more likely to occur after the age of 45 years.
It affects over 30 million Americans, according to the United States Centers for Disease Control and Prevention (CDC), and it accounts for 90–95 percent of diabetes cases.
This article looks at the early signs and symptoms of type 2 diabetes, the risk factors, and potential complications.
What is type 2 diabetes?
People with type 2 diabetes do not make or use insulin correctly.
Insulin is a hormone that regulates the movement of blood glucose, or sugar, into cells, which use it as energy.
When sugar cannot enter cells, this means:
- too much glucose collects in the blood
- the body’s cells cannot use it for energy
A doctor may diagnose diabetes if a person’s blood sugar levels are 126 milligrams per deciliter (mg/dl) or above after fasting for 8 hours.
Symptoms
The symptoms of high blood sugar in type 2 diabetes tend to appear gradually. Not everyone with type 2 diabetes will notice symptoms in the early stages.
If a person does experience symptoms, they may notice the following:
- Frequent urination and increased thirst: When excess glucose builds up in the bloodstream, the body will extract fluid from tissues. This can lead to excessive thirst and the need to drink and urinate more.
- Increased hunger: In type 2 diabetes, the cells are not able to access glucose for energy. The muscles and organs will be low on energy, and the person may feel more hungry than usual.
- Weight loss: When there is too little insulin, the body may start burning fat and muscle for energy. This causes weight loss.
- Fatigue: When cells lack glucose, the body becomes tired. Fatigue can interfere with daily life when a person has type 2 diabetes.
- Blurred vision: High blood glucose can cause fluid to be pulled from the lenses of the eyes, resulting in swelling, leading to temporarily blurred vision.
- Infections and sores: It takes longer to recover from infections and sores because blood circulation is poor and there may be other nutritional deficits.
If people notice these symptoms, they should see a doctor. Diabetes can lead to a number of serious complications. The sooner a person starts to manage their glucose levels, the better chance they have of preventing complications.
Symptoms in children and teens
Type 2 diabetes is more likely to appear after the age of 45 years, but it can affect children and teens who:
- have excess weight
- do not do much physical activity
- have high blood pressure
- have a family history of type 2 diabetes
- have an African American, Asian American, Hispanic American, or American Indian background
The following symptoms may occur:
- weight loss, despite increased appetite and hunger
- extreme thirst and dry mouth
- frequent urination and urinary tract infections
- fatigue
- blurred vision
- slow healing of cuts or wounds
- numbness or tingling in hands and feet
- itchy skin
If caregivers notice these symptoms, they should take the child to see a doctor. These are also symptoms of type 1 diabetes. Type 1 is less common but more likely to affect children and teenagers than adults. However, type 2 diabetes is becoming more common in young people than it was in the past.
Symptoms in older adults
At least 25.2 percent of people aged 65 and above have type 2 diabetes in the United States. They may have some or all the classic symptoms of type 2 diabetes.
They may also experience one or more of the following:
- flu-like fatigue, which includes feeling lethargic and chronically weak
- urinary tract infections
- numbness and tingling in the hands, arms, legs, and feet due to circulation and nerve damage
- dental problems, including infections of the mouth and red, inflamed gums
Sexual health
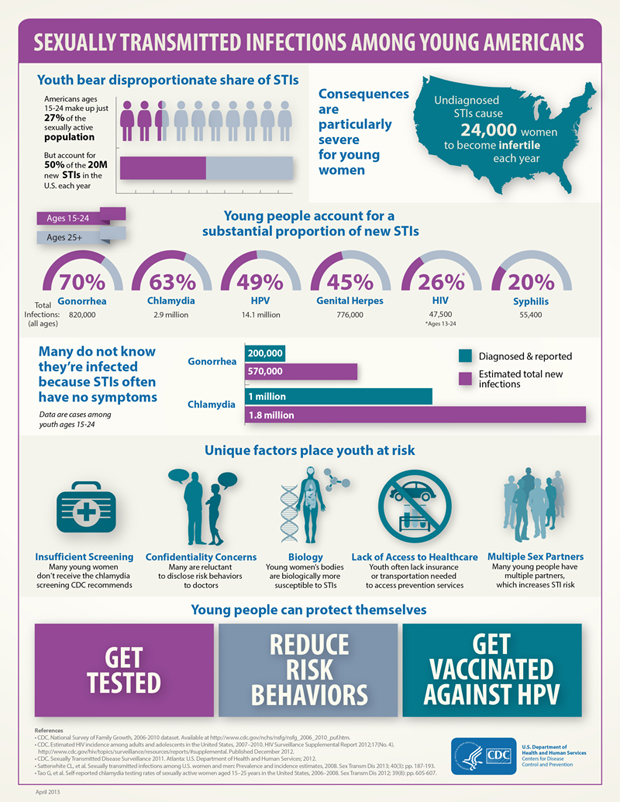
Sexually transmitted infections (STIs) have been on the rise in the United States. In April 2021, the Centers for Disease Control and Prevention (CDC) announced that, in 2019, STIs had reached an all-time high for the sixth consecutive year.
In 2019, the CDC received reports of over 2.5 million cases of chlamydia, gonorrhea, and syphilis.
The World Health Organization (WHO) estimates that 1 million STIs are acquired worldwide each day.
Despite rising rates, there is still significant stigma attached to STIs. For some, this might mean individuals are less willing to speak about sexual health concerns or raise questions with a doctor.
This unwillingness to speak openly about sexual health can breed misinformation.
Of course, the internet is a convenient first port of call when someone has a question they would like to ask anonymously. Sadly, not all information that appears on the web can be trusted.
Here, Medical News Today approached some common myths associated with sexual health and asked for input from an expert:
Dr. Sue Mann, a consultant in sexual and reproductive health and a medical expert in reproductive health at Public Health England.
Increasing understanding of sexual health helps people make informed, safe decisions. Although one article cannot brush away deeply ingrained falsehoods, the more trustworthy information that is available, the better.
1. When someone is taking ‘the pill,’ they cannot contract an STI
This is a myth. Oral contraception cannot protect against contracting an STI.
As Dr. Mann explained to MNT, “oral contraception […] only works to prevent pregnancy. The only way to protect yourself from getting an STI when using oral contraception is by wearing a condom.”
Mirroring this, the CDC states: “Birth control methods like the pill, patch, ring, and intrauterine device (IUD) are very effective at preventing pregnancy, but they do not protect against [STIs] and HIV.”
2. The ‘withdrawal method’ prevents pregnancy
The so-called withdrawal method, also called coitus interruptus or the pull-out method, is when the penis is pulled out of the vagina before ejaculation. Although it may reduce the chance of pregnancy, “the withdrawal method is not a reliable way to prevent pregnancy,” said Dr. Mann.
When used accurately, it can reduce the risk of pregnancy, but accuracy can be difficult in the heat of the moment.
Additionally, the penis releases pre-ejaculate, or pre-cum, before ejaculation. In some cases, sperm can be present in this fluid.
In one study, for instance, scientists examined samples of pre-ejaculate from 27 participants. The scientists identified viable sperm in 10 of the participant’s pre-ejaculate.
Each volunteer provided a maximum of five samples. Interestingly, the researchers found sperm in either all or none of their samples. In other words, some people tend to have sperm in their pre-ejaculate, while others do not. The authors concluded:
“[C]ondoms should continue to be used from the first moment of genital contact, although it may be that some men, less likely to leak spermatozoa in their pre-ejaculatory fluid, are able to practice coitus interruptus more successfully than others.”
4. Using two condoms doubles the protection
It is understandable why people might assume two condoms would provide twice the protection, but this is a myth.
“It is actually more risky to use two or more condoms when having sex,” said Dr. Mann. “The likelihood of the condom breaking is higher due to the amount of friction the condom is enduring. A single condom is the best option.”
5. You can contract STIs from a toilet seat
This is perhaps one of the most persistent myths associated with STIs. Yet, despite being repeatedly debunked, it remains a myth. Dr. Mann told MNT:
“STIs are spread through unprotected vaginal, anal, or oral sex, and by genital contact and sharing sex toys.”
She also explained that the viruses that cause “STIs cannot survive for long outside the human body, so they generally die quickly on surfaces like toilet seats.”
Similarly, the bacteria responsible for STIs, such as chlamydia, gonorrhea, and syphilis, cannot survive outside the body’s mucous membranes for a significant amount of time. For that reason, they would not survive on a toilet seat.
6. There are no treatments for STIs
This is not true. However, although they can be treated, not all can be cured. The WHO explains that eight pathogens make up the vast majority of STIs.
Four of the eight are curable: the bacterial infections syphilis, gonorrhea, and chlamydia, and the parasitic infection trichomoniasis.
The remaining four are viral: hepatitis B, herpes simplex virus (HSV), HIV, and human papillomavirus (HPV). These cannot yet be cured. However, it is worth noting that HPV infections are often cleared by the body naturally.
7. You can’t contract an STI unless you have penetrative sex
“Penetrative sex isn’t the only way someone can contract an STI. Oral sex, genital contact, and sharing sex toys are other ways that STIs can be spread,” Dr. Mann told MNT.
Beyond sexual contact, it is also possible to contract an STI from exposure to blood that contains the infectious pathogen, including through sharing needles.
8. Only gay males contract HIV
This is another longstanding and entirely incorrect assumption. According to Dr. Mann:
“Anyone, regardless of sexual orientation, race, ethnicity, age, or gender, can contract HIV. If you have HIV and don’t know it, you’re more likely to pass it on. But if you know your status, you can make sure you and your partner(s) are taking steps to stay healthy.”
Dr. Mann underscores the importance of testing, explaining that in many countries, “testing is free, easy, and confidential. You can even do a test in the comfort of your own home.”
9. You can only transmit an STI if you have symptoms
“A lot of people pass on STIs to others without even knowing,” said Dr. Mann. “STIs can be spread with symptoms or without.”
Indeed, the WHO explains that “[t]he majority of STIs have no symptoms or only mild symptoms that may not be recognized as an STI.”
“That is why,” Dr. Mann explained, “it is important to be tested regularly and to use a condom to prevent STIs as much as possible.”
Medical myths: All about skin
Our skin plays multiple roles. For instance, it helps keep our insides inside and blocks the path of pathogens. It also helps us stay warm when it is cold and cool down when it is hot.
Importantly, the skin provides a home for sensory neurons, which let us sense the world around us.
Despite the wide range of physiological functions this organ plays, it is arguably most famous for being the largest organ of the body, although some scientists disagree. The skin is also our most visible organ.
And because it is so visible, skin has also become the target organ for a wide range of products, many of which promise clearer, healthier, more youthful skin.
Because the skin, for many of us, is the poster child of our face, it is no wonder that scientists, doctors, and charlatans have paid it a great deal of attention over the years.
With this heady cocktail of high visibility and multiple physiological roles, it is no wonder that public dermatological perceptions are a mixed bag of myths and misunderstandings.
In this article, we will address 12 common confusions. To help us wrestle fact from fiction, we enlisted the help of three experts:
- Prof. Hywel C. Williams, OBE, D.Sc.: a Fellow of the Academy of Medical Sciences and a National Institute for Health Research Senior Investigator Emeritus. Prof. Williams is also a professor of dermato-epidemiology and co-director of the Center of Evidence-Based Dermatology at Queen’s Medical Centre at Nottingham University Hospitals National Health Service (NHS) Trust.
- Dr. Derrick Phillips: a dermatologist and spokesperson for the British Skin Foundation.
- Dr. Beth G. Goldstein: Founder at Get Mr. and Central Dermatology Center.
1. Expensive skin cream can keep your skin ‘young’ forever
The skin cream industry is huge. For instance, in the United States in 2020, “prestige skin care” sales totaled $1.1 billion from April to June. And that marked an 18% drop from 2019 sales.
However, despite their lucrative popularity and regardless of cost, no skin creams can protect skin against aging indefinitely. “This is a marketing ploy and is certainly not true,” said Dr. Phillips.
As Prof. Williams explained to Medical News Today, “Simple moisturizers can achieve quite a lot. Creams containing topical retinoids can improve photoaging effects.” He dryly notes, however, that he is “not aware of any cream that keeps skin young forever.”
Dr. Goldstein informed us that “90% of skin aging is from photodamage. So all of the creams that state they can prevent wrinkles and aging are missing the mark.”
In agreement, Dr. Phillips wrote: “The most important intervention in slowing down the process is using a sunscreen with broadband UV cover.” Notably, he also notes that “these needn’t be expensive.”
2. Drinking water keeps your skin hydrated
This is a half-truth. According to Prof. Williams, drinking water only keeps your skin hydrated “in the sense that water keeps the body hydrated and skin is the largest organ of the body.”
It is only at certain, rare times when this might be the case. “There is no evidence that drinking water directly impacts your skin unless in extremes, such as heat stroke or severe dehydration,” said Dr. Goldstein.
3. Antibacterial soap is best for the skin
This is a myth. The skin’s natural microbiome is vital for maintaining healthy skin. “Using antibacterial soaps can upset that natural balance,” explained Prof. Williams. “They can also be harsher on the skin than pH neutral soaps.”
“Removing both the good and bad bacteria on a regular basis is not always the best idea,” added Dr. Goldstein, “unless you are in a situation where this is important, for instance, if you work in healthcare, food handling, or of course, during a pandemic.”
4. Having a dirty face causes acne
In Prof. Williams’s professional opinion, this is “nonsense.” Unless, he explained, the dirt “is contamination with oily substances such as hair pomade, oily make-up, or occupational oil exposure.”
Standard dirt will not produce acne.
“Acne is caused by a complex interaction of hormones and the skin, not dirt. People will use scrubs, toners, and many products to clean their faces to address or prevent acne, but often this can just result in irritation. The pores are plugged by keratin, a protein produced by the skin cells, not dirt.”
– Dr. Goldstein
Diving into the details, Dr. Phillips told MNT that, although the skin’s microbiome may differ in people who have acne compared with those who do not, this is not due to cleanliness.
He also adds an interesting note about a rather modern dermatological condition:
“In the past year, there has been a rise in ‘cell phone’ acne, where people get acne spots on the side of their face that presses against their mobile phones. It is thought to be related to a combination of short-wavelength visible light from smartphones, sweat, dust, heat, friction, and bacteria on the surface of the phones. Flares may be prevented by regularly cleaning phone screens.”
5. Chocolate causes acne
Simply put, Prof. Williams writes that this is “another myth.” For the reasons outlined above, this has no basis in fact.
6. All sun exposure is bad for the skin
“All sun exposure causes some degree of photodamage,” explained Prof. Williams, “but some sun exposure is essential for boosting vitamin D synthesis,” especially for people in regions that are further from the equator and those with darker skin who receive lower sun exposure.
Similarly, Dr. Philips told MNT that “The sun is a major source of vitamin D, which is important for bone health and may play a role in the immune system. We also know that UV exposure from the sun has anti-inflammatory properties that can be beneficial in some skin conditions, such as psoriasis, eczema, and pruritus.”
However, he also explained that “these benefits must be counterbalanced against the risk of skin cancer, which we know in white populations is directly related to UV exposure.” He recommends using high-factor sunscreen, wearing appropriate clothing, and staying in the shade between 11 a.m. and 3 p.m. on sunny days.
As someone who focuses on skin cancer surgery, Dr. Goldstein took a firmer line:
“There is a skin cancer epidemic with at least five million new cancers treated each year in the U.S. The majority of these cancers are due to sun exposure.”
Although vitamin D is essential, she explained that we can also derive it from foods and supplements,“1 in 5 Americans will get skin cancer, and melanoma is set to be the most common cancer among men, and only second to breast cancer in women by 2040.”
7. A spray tan protects against UV rays
A spray tan will not protect against sun damage unless it contains added UV protectants. “Just spraying color onto the skin does not protect against UV rays,” said Prof. Williams.
Dr. Phillips reiterates the message: “They do not provide any protection against UV radiation and should not be used as an alternative to sunscreen.”
8. Vitamin E helps get rid of scars
Over the years, many scientists have investigated whether vitamin E reduces the appearance of scars, but our experts were unanimous in their responses. To date, Prof Williams says, the evidence is “unconvincing.”
Dr. Goldstein agreed that “current data do not support the use of vitamin E to help get rid of scars.”
Dr. Phillips goes one step further, writing that “in some instances, it can be detrimental.” However, as an alternative approach, he told us that “silicone gel products have been consistently shown to prevent scar overgrowth and improve the appearance of mature scars.”
9. ’Natural’ products are better for the skin
Products that are marketed as “natural” are popular among consumers. However, the term “natural” says nothing about a product’s effectiveness or safety.
“Arsenic is natural after all,” Prof. Williams reminded us. “Many natural products, such as moisturizers, are very expensive and have no additional benefit over cheaper, refined products.”
He also noted that “natural products can have just as many side effects as well-tested medical products — they may not be as effective, and they may suffer from stability issues. But it is a personal choice — if people like the sound of the word ‘natural’ as a euphemism for ‘gentle’ or ‘safe’ and want to pay for the product, that is up to them.”
“Poison ivy is all-natural,” said Dr. Goldstein, “but you would not rub it all over your skin.” She also explained that all-natural products can still have “serious environmental impacts.” Importantly, according to Dr. Phillips, natural ingredients, especially in high quantities, can trigger allergies and irritate the skin.
10. Wounds need air to heal
This is a long-standing and pervasive myth, but, as Prof. Williams explained succinctly, it is “not true — wounds heal better with a clean, moist environment.”
In agreement, Dr. Goldstein said, “Research has shown that cells migrate better to initiate and continue healing in a moist environment in the early stages of healing in particular. Keeping a wound covered with Aquaphor or similar ointment and a bandage is ideal [if there is no infection].”
She also noted that, toward the end of the healing process, once new connective tissue and microscopic blood vessels have formed, air can aid the healing process.
11. Exfoliating daily is essential for healthy skin
Skin exfoliation is the process of removing dead cells from the surface of the skin. This can be achieved by using an exfoliation tool, a granular surface, or chemicals.
Although popular, exfoliation is not essential. As Prof. Williams explained to MNT, “the skin feels smoother after exfoliating, but repeated exfoliation is damaging the natural skin barrier.”
12. Black salve is a safe treatment for skin cancer
Over recent years, so-called black salve, a derivative of the bloodroot plant, has entered the marketplace. Unscrupulous companies market it as a way to treat skin cancer. In reality, black salve can be dangerous.
Prof. Williams told us that “sanguinarine — the active ingredient in black salve — can cause severe tissue necrosis and may not kill all skin cancer cells. Always see a dermatologist to get suspected skin cancer diagnosed properly first and discuss treatment options if then confirmed.”
He also sent us a link to a recent article discussing black salve. The authors explain that “clinical data concerning the efficacy of bloodroot primarily come from case studies with unfavorable outcomes involving patients who self-treated with bloodroot-containing black salves.”
Dr. Goldstein mirrors these findings, explaining that “I have seen sad outcomes of people trying this treatment.” She also reiterated that black salve damages healthy tissue without effectively curing cancer.
Dr. Phillips confirms the negative consequences of black salve: “The Food and Drug Administration (FDA) has listed black salve as a fake cancer cure, and it should be avoided!”
How can we prevent the spread of SARS-CoV-2 in children?
Children are being hospitalized with COVID-19 in record numbers across the United States. As most children are not old enough to get vaccinated, hospitalizations could further increase as schools reopen. Doctors and epidemiologists are thus calling for the use of safety precautions, such as masks and ventilation, during class.
The rise in cases of COVID-19 among children in the U.S. is primarily linked to the Delta variant. Cases are rising especially quickly in communities with low rates of COVID-19 vaccinations.
Although the Centers for Disease Control and Prevention (CDC) recommend universal indoor masking and physical distancing in schools, mask-wearing is optional in North Dakota and Ohio.
Rapidly increasing infection rates among children and teachers have forced many schools in the U.S. to halt in-person learning and turn to hybrid models of education. This comes despite 175 pediatric disease experts agreeing earlier this year that elementary schools could open full-time for in-person instruction.
Although children generally have milder COVID-19 symptoms than adults, the fact that few studies have investigated how the disease affects children means that many questions remain unanswered. For example, why are so many children being hospitalized with COVID-19? Which children are most at risk? And what can parents and authorities do so that children can return to school safely?
To answer these questions and more, we spoke with seven doctors and researchers who specialize in pediatrics and infectious diseases and have worked directly with children with COVID-19.
Why are COVID-19 hospitalizations among children increasing?
The Delta variant of COVID-19 is more than two times as contagious as previous variants. Alongside school reopenings, this may partially explain the increase in pediatric hospitalizations due to COVID-19.
The Delta variant that is circulating widely is more contagious, and children are getting infected more often than previously during the pandemic.
Now, you have a more contagious variant with fewer mitigation measures in place. With the rising number of cases, unfortunately, you will see more hospitalizations. As an example, if 2% of children need hospitalization, then it’s a big difference between 2% of 10,000 cases vs. 2% of 100,000 cases.
Another reason for rising COVID-19 hospitalizations among children may be that those under the age of 12 years cannot get the vaccination yet.
Vaccines remain effective at preventing severe illness, hospitalization, and death from [SARS-CoV-2] infection, even Delta strain infection,” Kristin Moffitt, M.D., an infectious disease expert at Boston Children’s Hospital, MA. “This is consistent with reports that the overwhelming majority of hospitalizations and deaths during the recent surge are occurring in unvaccinated individuals.
“Since children under 12 aren’t yet able to be vaccinated, and many adolescents and young adults remain unvaccinated relative to older individuals, this age group is making up a bigger proportion of those at risk for severe illness based on their unvaccinated status,” she added.
Dr. Karen Ravin, M.D., chief of infectious diseases at Nemours Children’s Hospital in Delaware, agreed. “Children under 12 years of age make up a substantial proportion of the unvaccinated population in the U.S., so they are the population at highest risk,” she said. “Early in the pandemic, schools were closed, and children had a lower risk of exposure in the community. Contrast this to now, schools are open for in-person instruction so children are at greater risk for being exposed, becoming infected, and, unfortunately, being hospitalized.”
“Overall, children are at lower risk for severe illness, hospitalization, and death due to COVID-19, but they are not at no risk.”
– Dr. Karen Ravin
“Early in the pandemic, those over 65 accounted for more severe disease and hospitalization. Now that this age group has a higher percentage of vaccinated persons, the disease burden will be seen in the younger, unvaccinated population,” noted Dr. Adriana Cadilla, an infectious diseases pediatric specialist at Nemours Children’s Hospital in Orlando, FL. “[In Florida,] there has been over a four-fold increase in child [SARS-CoV-2] infections in the past month,” Dr. Cadilla added.
Is the Delta variant more severe than earlier strains?
Although the number of COVID-19 cases among children is increasing more quickly now than at any other time in the pandemic, it is unclear whether the Delta variant of SARS-CoV-2 is more severe for children than previous variants.
“We don’t know if the Delta variant causes more severe disease for kids than previous variants, but it’s definitely more contagious,” said Dr. Chang.
Due to low testing and hospital admissions among children from previous variants, the data to compare the outcome of COVID-19 strains are sparse. As schools reopen, however, and safety precautions such as mask-wearing wane, more children are becoming infected with SARS-CoV-2 at the same time, leading to higher numbers of children developing severe COVID-19.
There are some indications to suggest that COVID-19 from the Delta variant is more severe in children than with earlier strains,” Dr. Allison Ross Eckard, M.D., professor of pediatrics and medicine at the Medical University of South Carolina.
“We are seeing a greater number of children, particularly unvaccinated adolescents, with more severe COVID-19 resulting in respiratory failure that is requiring intubation and sometimes ECMO (heart-lung bypass machine), ARDS (a very serious lung condition that develops as a result of the inflammation associated with COVID-19), and other COVID-related problems — all complications we more commonly see in adults,” she continued.
“It may be that the increased number of hospitalizations among children is a result of both of these factors — more cases combined with a higher chance of severe disease. More data is needed to determine the exact reason(s) behind what we are seeing,” she added.
Which children are at higher risk of adverse outcomes from COVID-19?
The CDC says that children with underlying medical conditions, such as congenital heart disease or genetic, neurologic, or metabolic conditions, could have an increased risk of severe outcomes from COVID-19.
The CDC states that this higher risk also applies to children with obesity, diabetes, asthma, chronic lung disease, sickle cell disease, or immunosuppression.
“Children who are at higher risk of adverse outcomes from COVID-19 are those under 1 year of age, those with underlying conditions, and those with immunocompromising conditions, including those on immunocompromising medications,” Dr. Tina Q. Tan, M.D., medical director at Ann & Robert H. Lurie Children’s Hospital of Chicago.
“Other children may also develop more severe disease, resulting in the need for hospitalization, but at a lower rate than those with underlying or immunocompromising conditions,” she added.
“Anecdotally, most of our hospitalized patients with COVID-19 are unvaccinated teenagers. Many of these teens are quite ill, and their only risk factors are obesity and/or asthma,” Dr. Danielle Zerr, M.D., M.P.H., professor and division chief of pediatric infectious disease and adjunct professor of epidemiology, University of Washington.
Dr. Chang echoed these statements, saying that teenagers with a body mass index of 25 or above and infants under the age of 1 year have a higher risk of hospitalization.
“Many families think their children are healthy and, therefore, not at risk of severe COVID-19,” said Dr. Eckard. “While that is true statistically, we cannot always predict which children will develop severe disease, and children [without underlying conditions] sometimes do develop severe disease.”
“In addition, some children are healthy but perhaps require an inhaler a couple of times per year, or some children’s families don’t even realize they are overweight. So, there is sometimes a misconception about a child’s risk. Therefore, it is very important for every family to discuss their child’s health with their primary care physicians to ensure that all children are appropriately protected.”
– Dr. Allison Eckard
“We are still learning what causes some children to develop more severe COVID-19 than others, but it is important to know that perfectly healthy children can develop severe COVID-19,” Elizabeth Mack, M.D., M.S., medical director of pediatric critical care medicine at the Medical University of South Carolina, told MNT.
Dr. Mack also noted that the risk of death from severe COVID-19 remains a possibility even for children without underlying conditions.
Race, ethnicity, and socioeconomic conditions may also play a role in adverse outcomes from COVID-19 among children. Dr. Cadilla noted, “Hospitalization rates are higher among Hispanic [and] Latino children and non-Hispanic Black children, mirroring adult data.”
While more data are necessary to confirm why this is the case among children, among adults, research highlights deep-seated inequities that put these populations at higher risk.
For example, Hispanic, Latinx, and non-Hispanic Black populations are more likely to be uninsured, working in jobs that do not offer remote working, and living in conditions that make it difficult to practice physical distancing and self-isolation. These populations also have higher rates of underlying health conditions, such as diabetes and obesity.
For live updates on the latest developments regarding the novel coronavirus and COVID-19, click here.
All data and statistics are based on publicly available data at the time of publication. Some information may be out of date. Visit our coronavirus hub and follow our live updates page for the most recent information on the COVID-19 pandemic.