Of all the modern medical interventions we have at our disposal, few have been victim to as much falsehood as vaccines. As the world battles a pandemic, stripping the truth from the lies is more urgent than ever.
According to the World Health Organization (WHO), between 2010 and 2015, vaccines prevented an estimated 10 million deaths.
Scientists have worked tirelessly to create safe and effective vaccines to protect us against SARS-CoV-2. Now, as many governments roll out COVID-19 vaccines, scientists and medical experts are facing a new challenge: misinformation and associated vaccine hesitancy.
Some anti-vaxxers — individuals who believe vaccines cause a range of medical ills — dedicate their entire lives to railing against vaccines. In reality, vaccines have saved lives of millions of people.
Vaccine hesitancy is nothing new and, in many ways, perfectly reasonable. For instance, misinformation about the vaccines’ safety and potential effects on the body is rife on the internet. Also, the COVID-19 vaccines were developed unusually swiftly and use relatively new technology.
Today, a significant percentage of the United States population, and the world at large, are nervous to take a shot that could save their lives.
In this article, we tackle some of the most common myths associated with the COVID-19 vaccines. Although it will not convince dyed-in-the-wool anti-vaxxers, we hope that this information will prove useful for those who are hesitant.
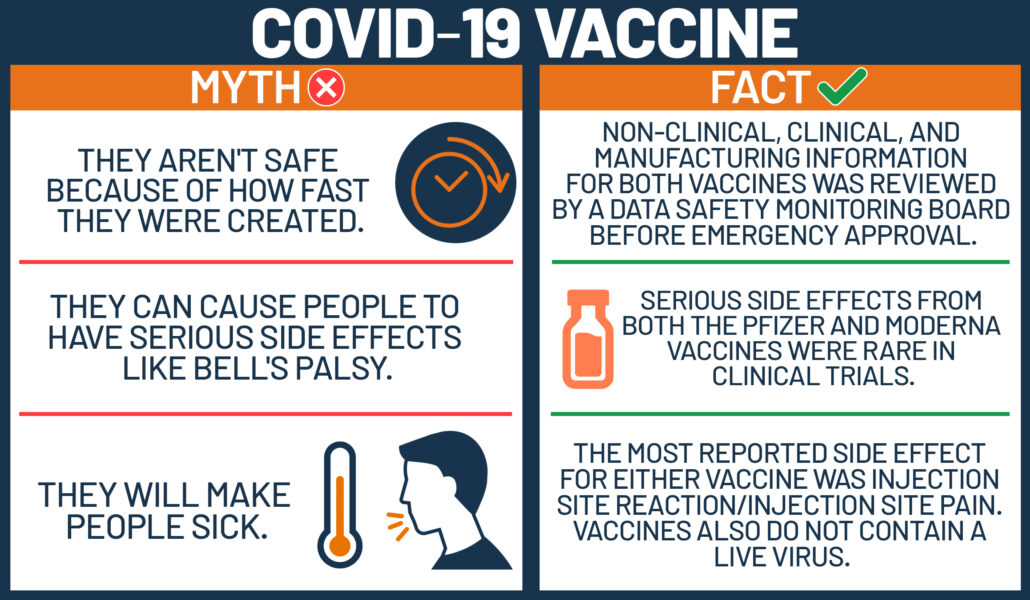
1. The vaccines are not safe, because they were developed so fast
It is true that scientists developed the COVID-19 vaccines faster than any other vaccine to date — under 1 year. The previous record breaker was the mumps vaccine, which was developed in 4 years.
There are a number of reasons the COVID-19 vaccines were developed more quickly, none of which reduces its safety profile.
For instance, scientists were not starting from scratch. Although SARS-CoV-2 was new to science, researchers have been studying coronaviruses for decades.
Also, because COVID-19 has touched every continent on earth, the process of vaccine development involved an unprecedented worldwide collaboration. And, while many scientific endeavors face funding difficulties, COVID-19 researchers received funding from a wide range of sponsors.
Another factor that slows vaccine development is recruiting volunteers. In the case of COVID-19, there was no shortage of people who wanted to help.
Also, under normal circumstances, clinical trials are run sequentially. But in this instance, scientists could run some trials simultaneously, which saved a great deal of time.
These factors and more meant that the vaccine could be developed swiftly without compromising safety.
In short: identifying the virus was quicker; we already had experience with similar pathogens; technology has moved on since the 1980s; every government on earth had a vested interest; and there were few financial restraints.
2. The vaccine will alter my DNA
Some COVID-19 vaccines, including the Pfizer-BioNTech and Moderna vaccines, are based on messenger RNA (mRNA) technology. These vaccines work differently to traditional types of vaccine.
Classical vaccines introduce an inactivated pathogen or part of a pathogen to the body to “teach” it how to produce an immune response.
By contrast, an mRNA vaccine delivers the instructions for making a pathogen’s protein to our cells. Once the protein is created, the immune system responds to it, priming it to respond to future attacks by the same pathogen.
However, the mRNA does not hang around in the body, and it is not integrated into our DNA. Once it has provided the instructions, the cell breaks it down.
In fact, the mRNA will not even reach the cell’s nucleus, which is where our DNA is housed.
3. COVID-19 vaccines can give you COVID-19
The COVID-19 vaccines cannot give an individual COVID-19. Regardless of the type of vaccine, none contains the live virus. Any side effects, such as headache or chills, are due to the immune response and not an infection.
4. The vaccine contains a microchip
A YouGov poll conducted in the U.S. last year asked 1,640 people a range of questions about COVID-19. An incredible 28% of respondents believe that Bill Gates plans to use the COVID-19 vaccinations as a vehicle to implant microchips into the population.
According to some, this microchip will allow shadowy elites to track their every move. In reality, our mobile phones already complete that task effortlessly.
There is no evidence that any of the COVID-19 vaccines contains a microchip.
Although the specifics vary from conspiracy theory to conspiracy theory, some believe that the vaccine contains radio-frequency identification tags. These consist of a radio transponder, radio receiver, and transmitter. It is not possible to shrink these components to a size small enough to fit through the end of a needle.
5. COVID-19 vaccines can make you infertile
There is no evidence that the COVID-19 vaccines impact fertility. Similarly, there is no evidence that they will endanger future pregnancies.
This rumor began because of a link between the spike protein that is coded by the mRNA-based vaccines and a protein called syncytin-1. Syncytin-1 is vital for the placenta to remain attached to the uterus during pregnancy.
However, although the spike protein does share a few amino acids in common with syncytin-1, they are not even nearly similar enough to confuse the immune system.
The rumor appears to have begun courtesy of Dr. Wolfgang Wodarg. In December of last year, he petitioned the European Medicines Agency to halt COVID-19 vaccine trials in the European Union. Among his concerns was the syncytin-1 “issue” mentioned above.
Dr. Wodarg has a history of skepticism toward vaccines and has downplayed the severity of the COVID-19 pandemic. Dr. Wodarg and the former vice president and chief scientist of Pfizer Inc. pharmaceuticals joined voices to make claims about the vaccine producing infertility, thus stoking widespread fears.
However, there is no evidence that any COVID-19 vaccine affects fertility.
6. The COVID-19 vaccine contains fetal tissue
Over the years, anti-vaxxers have spread rumors that vaccines contain fetal tissue. Neither the COVID-19 vaccines nor any other vaccine contains any tissue from fetuses.
As Dr. Michael Head, a senior research fellow at the University of Southampton in the United Kingdom, told the BBC, “There are no fetal cells used in any vaccine production process.”
7. People who have had COVID-19 do not need the vaccine
Even people who have tested positive for SARS-CoV-2 in the past should be vaccinated. As the Centers for Disease Control and Prevention (CDC) write:
“Due to the severe health risks associated with COVID-19 and the fact that reinfection with COVID-19 is possible, [a] vaccine should be offered to you regardless of whether you already had [a SARS-CoV-2] infection.”
There is also a chance that the initial test produced a false positive — in other words, the test was positive, but there was no viral infection. For this reason, it is better to err on the side of caution.
8. After receiving the vaccine, you cannot transmit the virus
COVID-19 vaccines are designed to prevent people from becoming ill following a SARS-CoV-2 infection. However, a person who has been vaccinated may still be able to carry the virus, which means that they might also be able to transmit it.
Because scientists do not yet know whether the vaccines will prevent infection, once a person has been vaccinated, they should continue to wear a mask in public, wash their hands, and practice physical distancing as recommended by regional authorities.
9. Once I have been vaccinated, I can resume a normal life
Unfortunately, for the reasons mentioned above, this is not true.
10. The vaccine will protect against COVID-19 for life
Because scientists have only been studying the virus for around 1 year, we do not know how long immunity will last. According to the WHO:
“It’s too early to know if COVID-19 vaccines will provide long-term protection. […] However, it’s encouraging that available data suggest that most people who recover from COVID-19 develop an immune response that provides at least some period of protection against reinfection — although we’re still learning how strong this protection is and how long it lasts.”
It may be that we will need to have an annual COVID-19 shot, in the same way that we do with the flu shot.
11. People with preexisting conditions cannot take the vaccine
This is untrue. People with most preexisting conditions — including heart disease, diabetes, and lung disease — can take a COVID-19 vaccine. However, if anyone is concerned, it is always advisable to speak with a doctor.
In fact, because preexisting conditions, such as obesity and heart disease, can increase the risk of developing more severe COVID-19 symptoms, being vaccinated is even more important for people with preexisting health issues.
There is an exception: individuals who are allergic to any of the components of the vaccine should not have the shot. Anyone who has had an allergic reaction to any vaccine in the past should speak with their doctor.
However, the CDC recommend “that people with a history of severe allergic reactions not related to vaccines or injectable medications — such as food, pet, venom, environmental, or latex allergies — get vaccinated. People with a history of allergies to oral medications or a family history of severe allergic reactions may also get vaccinated.”
12. People with compromised immune systems cannot have the vaccine
Because the vaccine does not contain a live pathogen, it will not cause an infection. Therefore, individuals who have a compromised immune system can still take the vaccine. However, they may not build up immune protection to the same degree as someone with a fully functioning immune system.
The CDC also explain that few people who have a compromised immune system were involved in the vaccine trials:
“Immunocompromised individuals may receive [a] COVID-19 vaccination if they have no contraindications to vaccination. However, they should be counseled about the unknown vaccine safety profile and effectiveness in immunocompromised populations.”
13. Older adults cannot have the vaccine
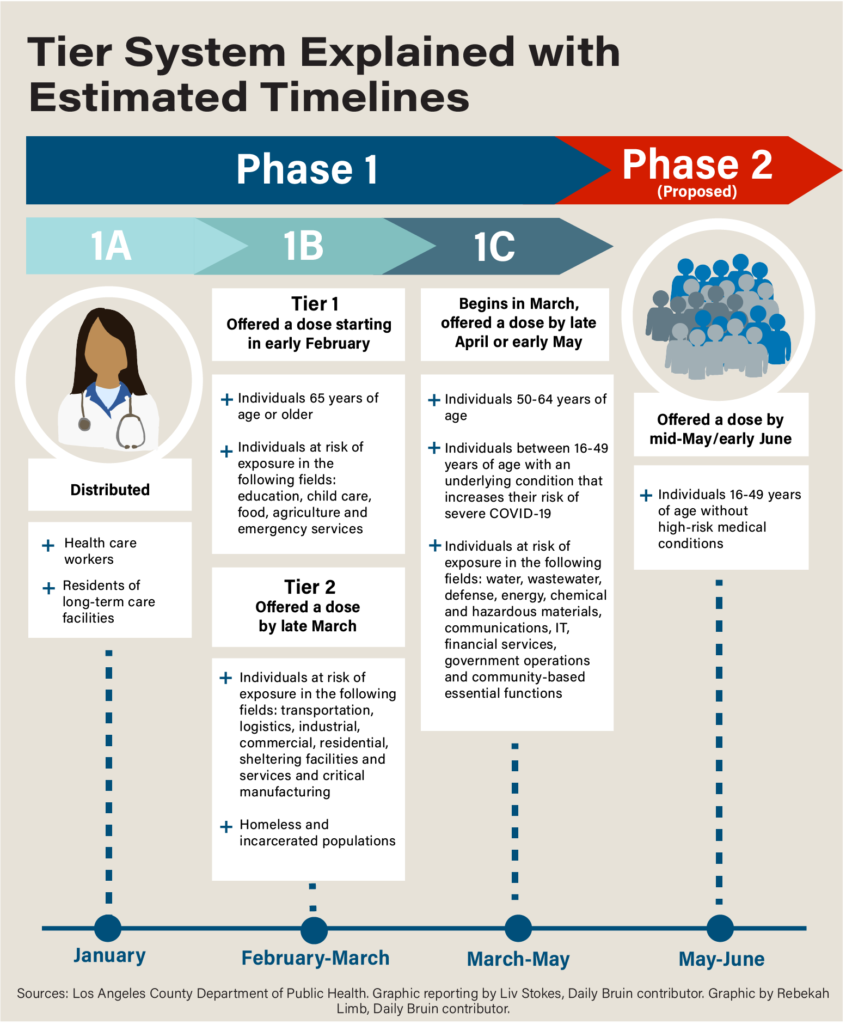
This is a myth. Currently, in most countries where officials are rolling out the vaccine, older adults are being prioritized, as they are most at risk of severe illness.
Also, some of the clinical trials had specific subgroups that included older adults to check the vaccine’s safety in this population.
In Norway, 23 frail older adults died shortly after they received the Pfizer-BioNTech vaccine. This, perhaps, helps explain why this myth is gaining traction.
The Norwegian Medicines Agency (NOMA) are currently investigating the situation. Steinar Madsen, a medical director at NOMA, believes that common adverse reactions, such as fever, nausea, and diarrhea, “may aggravate underlying disease in the elderly.”
Madsen also explained that “these are very rare occurrences, and they occurred in very frail patients with very serious disease.” He went on to add,
“We are now asking for doctors to continue with the vaccination but to carry out extra evaluation of very sick people whose underlying condition might be aggravated by it.”
The take-home
It is hard to believe that not much more than 1 year ago, COVID-19 and SARS-CoV-2 were entirely unknown. Now, we have a number of viable, effective, and safe vaccines.
In this internet-fueled era, rumors grow and spread like wildfire. The addition of a significant dose of fear and anxiety provides the perfect petri dish in which to grow stubborn, dangerous myths.
The situation and the science are moving quickly, and the best advice is to ensure that you always take information from reliable sources and do not pay attention to powerful but misleading social media posts.