All about borderline diabetes (prediabetes)
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
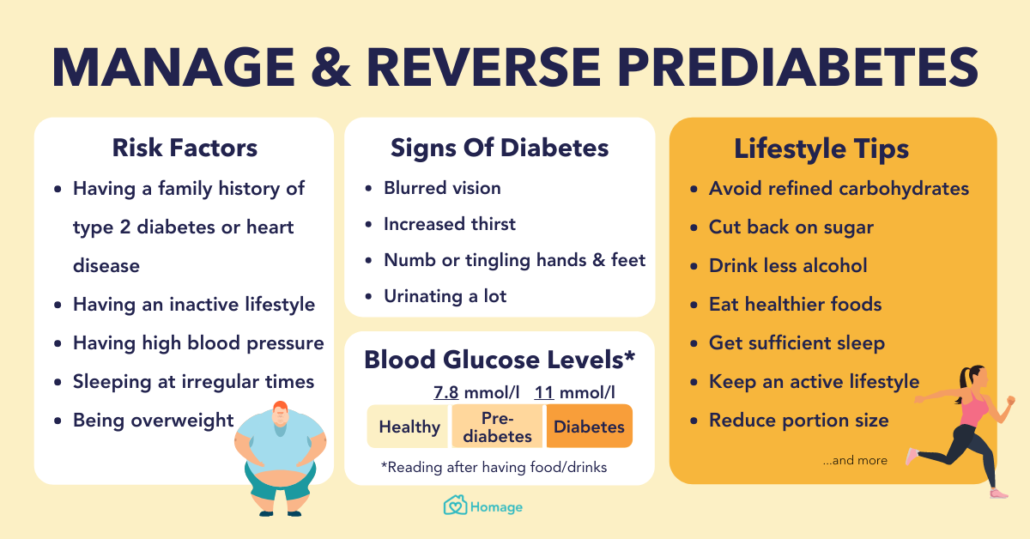
A person with borderline diabetes, or prediabetes, has blood sugar levels that are higher than normal but not yet high enough for a diagnosis of type 2 diabetes.
Borderline diabetes is a condition that may lead to type 2 diabetes. According to the American Diabetes Association, an estimated 10 to 23 percent of people with borderline diabetes will go on to develop type 2 diabetes within 5 years.
Doctors may also refer to borderline diabetes as:
- insulin resistance
- impaired glucose tolerance
- impaired fasting glucose
This article looks at how to recognize risk factors for prediabetes, how to manage the condition, and how to prevent type 2 diabetes from developing.
Symptoms
Prediabetes does not have clear symptoms. Some people may not be aware that they have it until:
- a doctor tests blood glucose and blood pressure levels
- prediabetes has progressed to type 2 diabetes
- a complication occurs, such as a heart attack
If a person’s blood sugar level remains high, they may begin to develop some symptoms of type 2 diabetes. Symptoms include frequent urination and increased thirst.
Most people will not know they have prediabetes until they receive testing.
Causes and risk factors
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), a range of other conditions can increase the risk of prediabetes, including:
- obesity, especially abdominal obesity
- high blood pressure
- high blood fat levels, or triglycerides
- low levels of “good” high-density lipoprotein (HDL) cholesterol
Other risk factors include:
- not getting enough exercise
- having a family history of type 2 diabetes.
According to the American Heart Association, the following lifestyle factors may also be a risk for prediabetes in some people:
- raised stress levels
- smoking
- drinking too much alcohol
Regularly consuming high-sugar drinks may also increase the risk.
One 2017 review found that people who regularly drink sugary beverages face an increased risk of metabolic diseases, such as high blood pressure and high levels of blood glucose and fats.
These metabolic conditions can lead to prediabetes and diabetes.
People who lead an inactive lifestyle are at higher risk of taking in too many calories without burning them through exercise.
Other people who may be at risk of developing prediabetes include those with polycystic ovary syndrome (PCOS) and those who have experienced instances of high blood sugar levels in the past.
Anyone with any of these risk factors may benefit from a prediabetes screening to identify whether they have the condition.
Diagnosis
A doctor typically diagnoses prediabetes with a blood test, particularly a glucose tolerance test. A glucose tolerance test measures how quickly the body can process the sugar in the blood in a 2-hour period.
Other tests include measuring blood sugar levels after a person has not eaten for a specific period. This is called a fasting blood test.
The doctor may also use an A1C test. This involves measuring the average blood sugar levels over 2–3 months. People do not need to fast or take any special liquids or medications for this test, and it gives reliable results.
According to the American Diabetes Association, a doctor will diagnose prediabetes when test results show the following measurements:
- fasting blood sugar levels of 100–125 milligrams per deciliter (mg/dl)
- glucose tolerance levels of 140–199 mg/dl
- an A1C test result of 5.7–6.4 percent
A doctor will often re-test these levels to confirm that the readings are not due to one-off spikes in blood sugar.
Blood glucose monitors for home use are available for purchase online.
Who should seek screening?
The NIDDK recommend that people with the following risk factors should undergo a prediabetes screening:
- an age of 45 years or over
- obesity or overweight, or a body mass index (BMI) over 25
- a waist circumference larger than 40 inches in males or over 35 inches in females
- a close relative with diabetes
- a condition that increases insulin resistance, including PCOS, acanthosis nigricans, and nonalcoholic steatohepatitis
- an ethnic background that places an individual at high risk of diabetes, including people who are African-American, Asian-American, Latino, Native American, or a Pacific Islander
- a history of gestational diabetes, or diabetes as a result of pregnancy
- having given birth to an infant weighing over 9 pounds
- having a disease that harden the arteries
- recent treatment with glucocorticoids or atypical antipsychotic medications
If a doctor identifies any of these risk factors, they may recommend that the person has a screening for blood glucose levels.
Medical professionals advise repeating screening tests every 1 to 3 years if a person has these risk factors.
The NIDDK has an official resource to check diabetes risk. Click here to take the test.
However, anyone who is concerned that they may have borderline diabetes should visit the doctor for testing and a proper diagnosis.
Treatment
Prediabetes is reversible, but it is often easier to prevent than treat. Lifestyle factors are the primary causes of prediabetes, and making changes in some aspects of life can significantly reduce risk factors.
A balanced, nutritious diet that moderates sugar intake and regular exercise can help reverse borderline diabetes.
According to the American Diabetes Association, diet and nutrition changes should include the following:
- improving intake of unprocessed high-fiber carbohydrates
- increasing fruit and vegetable consumption
- reducing saturated fat and processed meat intake.
Click here to find out more about what to eat with prediabetes.
Exercise is also important. According to a report in Diabetes Care, exercise can help prevent or delay diabetes from developing.
Current guidelines for Americans recommend that adults should:
- have at least 150–300 minutes of moderate-intensity aerobic activity each week
- do muscle-strengthening exercises at least twice a week, such as lifting weights or doing push-ups
Examples of moderate exercise are fast dancing and brisk walking.
Regular exercise and a healthful diet not only help reduce the risk of developing diabetes but also protect the heart against future diseases.
Diabetes Prevention Program
The Diabetes Prevention Program (DPP) was a long-term study that aimed to identify practical steps for reducing diabetes risk and reversing prediabetes.
The people who took part in the DPP Lifestyle Change Program aimed to lose 7 percent of their body weight and maintain this loss through dietary changes and activity. After 3 years, the results of the program showed:
- a 58-percent drop in the risk of developing diabetes regardless of sex or ethnicity, compared with those who took a placebo
- a 71-percent drop in risk people of developing type 2 diabetes among people aged over 60 years
All the people in the program received motivational support on effective diet and exercise and attended “lifestyle change classes,” for the duration of the study.
Follow-ups took place regularly. After 15 years, people in the DPP Lifestyle Change Program continued to see a delay in the onset of diabetes compared to people who took a medication called metformin or a placebo.
Anyone who developed diabetes during the study received extra medical care. However, diet and exercise remained important in managing symptoms and reducing the risk of complications.
Monitoring borderline diabetes
In addition to lifestyle changes, doctors may recommend other steps for managing the risk of diabetes.
Medical management may include treating related conditions, such as obesity and heart disease.
Managing prediabetes also involves continued monitoring of the risk factors and regular testing of blood sugar levels.
A person can reverse borderline diabetes if they can make and maintain the necessary lifestyle changes.
Takeaway
Borderline diabetes is the stage before type 2 diabetes develops. By this stage, blood sugar, blood pressure, and insulin resistance may start reaching harmful levels.
Prediabetes does not usually cause active symptoms, and most people will not be aware they have the condition until it becomes diabetes and starts causing severe health problems.
It is therefore essential for anyone who is at risk of developing diabetes to receive regular screening. Risk factors include high BMI and waist circumference, an age of more than 45 years, or other cardiovascular diseases.
Prediabetes is often reversible with a sustained exercise program and a balanced, low-sugar diet.