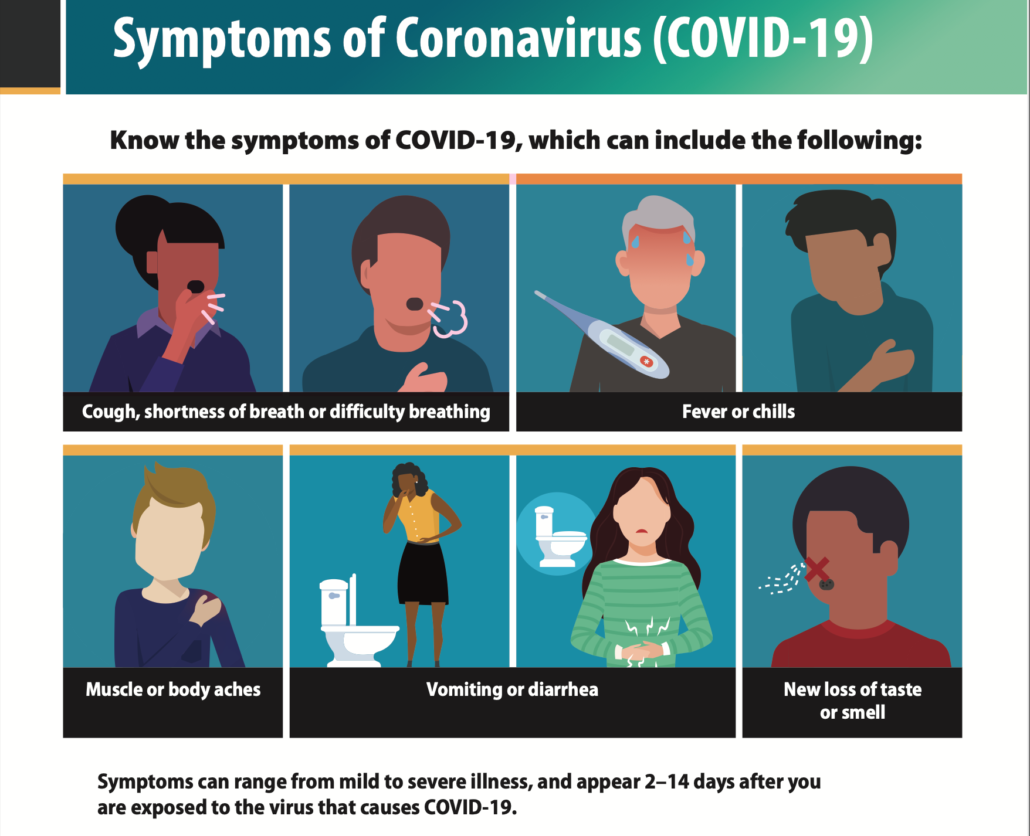
Watch for symptoms of COVID-19
People with COVID-19 have had a wide range of symptoms reported – ranging from mild symptoms to severe illness. Symptoms may appear 2-14 days after exposure to the virus. Anyone can have mild to severe symptoms. People with these symptoms may have COVID-19:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
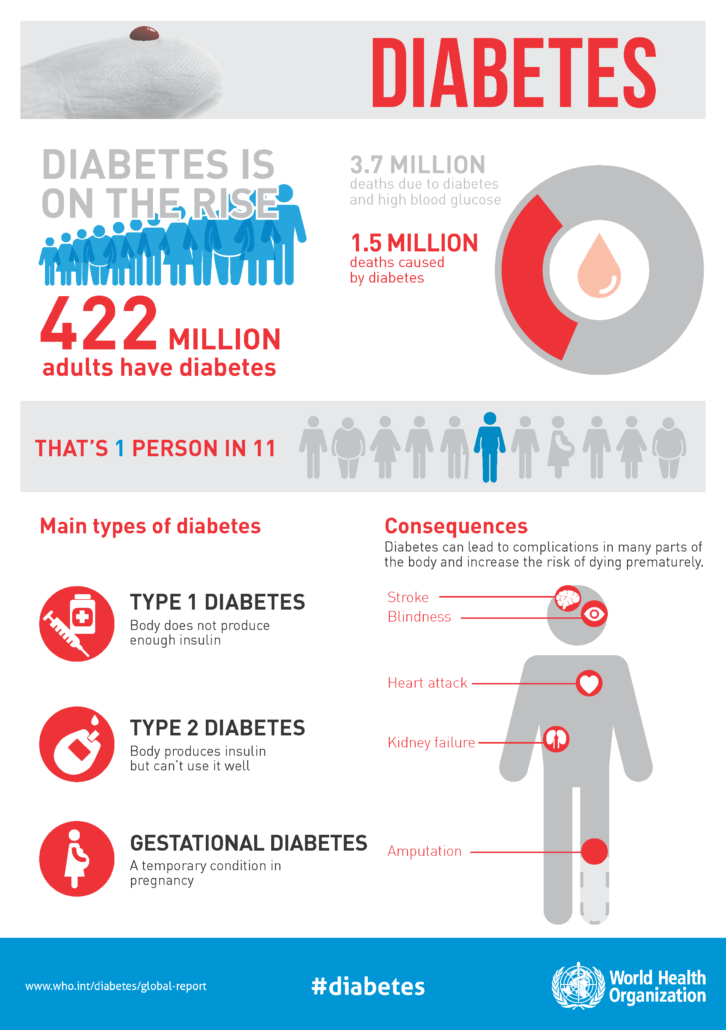
This list does not include all possible symptoms. CDC will continue to update this list as we learn more about COVID-19. Older adults and people who have severe underlying medical conditions like heart or lung disease or diabetes seem to be at higher risk for developing more serious complications from COVID-19 illness.
When to Seek Emergency Medical Attention
Look for emergency warning signs* for COVID-19. If someone is showing any of these signs, seek emergency medical care immediately:
- Trouble breathing
- Persistent pain or pressure in the chest
- New confusion
- Inability to wake or stay awake
- Pale, gray, or blue-colored skin, lips, or nail beds, depending on skin tone
*This list is not all possible symptoms. Please call your medical provider for any other symptoms that are severe or concerning to you.
Call 911 or call ahead to your local emergency facility: Notify the operator that you are seeking care for someone who has or may have COVID-19.
If You Are Sick
- Check symptoms with Coronavirus Self-Checker
- Get tested
- What to do if you are sick
- Isolate if you are sick
- When to quarantine
- How to care for someone who is sick
Difference between COVID-19 & Flu
Influenza (Flu) and COVID-19 are both contagious respiratory illnesses, but they are caused by different viruses. COVID-19 is caused by infection with a new coronavirus (called SARS-CoV-2), and flu is caused by infection with influenza viruses.
COVID-19 seems to spread more easily than flu and causes more serious illnesses in some people. It can also take longer before people show symptoms and people can be contagious for longer. More information about differences between flu and COVID-19 is available in the different sections below.
Because some of the symptoms of flu and COVID-19 are similar, it may be hard to tell the difference between them based on symptoms alone, and testing may be needed to help confirm a diagnosis.
While more is learned every day about COVID-19 and the virus that causes it, there is still a lot that is unknown . This page compares COVID-19 and flu, given the best available information to date.
If you or your family member are at high risk for severe illness, wear a mask or respirator with greater protection in public indoor spaces if you are in an area with a high COVID-19 Community Level. Talk with your healthcare provider about wearing a mask in a medium COVID-19 Community Level.
If you test positive for COVID-19 and have one or more health conditions that increase your risk of becoming very sick, treatment may be available. Contact a health professional right away after a positive test to determine if you may be eligible, even if your symptoms are mild right now. Don’t delay: Treatment must be started within the first few days to be effective.