Everything you need to know about fibromyalgia
Fibromyalgia is a common and chronic syndrome that causes bodily pain and mental distress.
Symptoms of fibromyalgia can be confused with those of arthritis, or joint inflammation. However, unlike arthritis, it has not been found to cause joint or muscle inflammation and damage. It is seen as a rheumatic condition, in other words, one that causes soft tissue pain or myofascial pain.
According to the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), around 5 million adults aged 18 years or over in the United States experience fibromyalgia, and 80 to 90 percent of fibromyalgia patients are women.
Symptoms
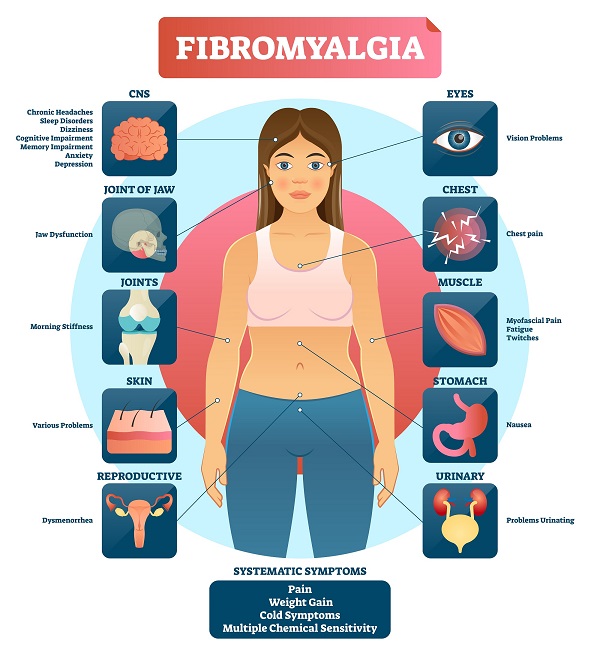
Common symptoms include:
- widespread pain
- jaw pain and stiffness
- pain and tiredness in the face muscles and adjacent fibrous tissues
- stiff joints and muscles in the morning
- headaches
- irregular sleep patterns
- irritable bowel syndrome (IBS)
- painful menstrual periods
- tingling and numbness in the hands and feet
- restless leg syndrome (RLS)
- sensitivity to cold or heat
- difficulties with memory and concentration, known as “fibro-fog”
- fatigue
The following are also possible:
- problems with vision
- nausea
- pelvic and urinary problems
- weight gain
- dizziness
- cold or flu-like symptoms
- skin problems
- chest symptoms
- depression and anxiety
- breathing problems
Symptoms can appear at any time during a person’s life, but they are most commonly reported around the age of 45 years.
Treatment
Around 20 percent of people with fibromyalgia try acupuncture within the first 2 years. It may work, but more research is needed.
Medical attention is needed because fibromyalgia can be difficult to manage. As it is a syndrome, each patient will experience a different set of symptoms, and an individual treatment plan will be necessary.
Treatment may include some or all of the following:
- an active exercise program
- acupuncture
- psychotherapy
- behavior modification therapy
- chiropractic care
- massage
- physical therapy
- low-dose anti-depressants, although these are not a first-line treatment
People with fibromyalgia need to work with their doctor to come up with a treatment plan that provides the best results.
Drugs
Drugs may be recommended to treat certain symptoms.
These may include over-the-counter (OTC) pain relievers. However, the European League Against Rheumatism (EULAR) issued a recommendation against using non-steroidal anti-inflammatory drugs (NSAIDs) to treat fibromyalgia in their updated 2016 guidelines.
Antidepressants, such as duloxetine, or Cymbalta, and milnacipran, or Savella, may help reduce pain. Anti-seizure drugs, such as gabapentin also known as Neurontin, and pregabalin, or Lyrica, may be prescribed.
However, a review has suggested that patients often stop using these drugs because they are not effective in relieving pain or because of their adverse effects.
Patients should tell the doctor about any other medications they are taking to avoid side-effects and interactions with other drugs.
Exercise
A combination of aerobic exercise and resistance training, or strength training, has been linked to a reduction in pain, tenderness, stiffness, and sleep disturbance, in some patients.
If exercise is helping with symptoms, it is important to maintain consistency in order to see progress. Working out with a partner or personal trainer may help to keep the exercise program active.
Acupuncture
Some patients have experienced improvements in their quality of life after starting acupuncture therapy for fibromyalgia. The number of sessions required will depend on the symptoms and their severity.
One study found that 1 in 5 people with fibromyalgia use acupuncture within 2 years of diagnosis. The researchers concluded that it may improve pain and stiffness. However, they call for more studies.
Behavior modification therapy
Behavior modification therapy is a form of cognitive behavioral therapy (CBT) that aims to reduce negative, stress- or pain-increasing behaviors and improve positive, mindful behaviors. It includes learning new coping skills and relaxation exercises.
Causes
The exact cause of fibromyalgia is unclear. However, current thinking in the field of Rheumatology suggests that fibromyalgia is a problem with central pain processing in the brain, where there may be an increased sensitivity or perception of pain to a given trigger.
There is a range of likely risk factors, including:
- a stressful, traumatic physical or emotional event, such as a car accident
- repetitive injuries
- rheumatoid arthritis or other autoimmune diseases, such as lupus
- central nervous system (CNS) problems
- the way our genes regulate how we process painful stimuli
Fibromyalgia may also be hereditary. Females who have a close relative with fibromyalgia have a higher risk of experiencing it themselves.
People with rheumatoid arthritis, lupus, or spinal arthritis, known ankylosing spondylitis, have a higher risk of developing fibromyalgia, as do patients with some other rheumatic diseases.
Diagnosis
It can take some time to confirm a diagnosis of fibromyalgia because the symptoms resemble those of other conditions, such as hypothyroidism. These conditions must first be ruled out before diagnosing fibromyalgia.
There are no laboratory tests for the condition, and this, too, can lead to delayed or missed diagnosis.
The American College of Rheumatology has established three criteria for diagnosing fibromyalgia.
- pain and symptoms over the previous week, out of 19 identified body parts, plus levels of fatigue, unsatisfactory sleep, or cognitive problems
- symptoms that have been ongoing for at least 3 months
- no presence of another health problem that would explain the symptoms
Previously, ‘tender points’ were used to diagnose the condition. However, these are no longer recommended to aid the diagnosis of fibromyalgia.
Diet
Dietary measures have been suggested for improving the symptoms of fibromyalgia.
These include:
- High-energy foods that are low in sugar: Foods such as almonds, beans, oatmeal, avocado, and tofu contain plenty of fiber but no added sugar. These can help boost energy throughout the day, helping to improve tiredness symptoms that occur as a result of the condition.
- Avoiding foods that have gluten: A 2014 study has suggested that gluten sensitivity can contribute to fibromyalgia. The study showed that removing foods that contain gluten from the diet may be able to reduce the pain, even in patients who do not have celiac disease. This is also linked to a diet plan for reducing inflammation.
- Cutting out fermentable oligo-di-mono-saccharides and polyols (FODMAP): A recent study showed that a diet low in FODMAP could have promising effects on pain levels in people with fibromyalgia.
- Not eating additives and excitotoxins: One report showed that cutting out additives from the diet, such as aspartame and monosodium glutamate (MSG), can reduce pain symptoms significantly. The pain of the people involved in the study was also shown to increase once these additives were put back in the diet.
- Eating more seeds and nuts: There is little evidence to support a direct relationship between seeds, nuts, and an improvement in fibromyalgia symptoms. However, they are known to contain powerful micronutrients and minerals that are important for cell function, and this may support people with the condition.
Maintaining a balanced diet and healthy weight is vital to ongoing health and can improve a person’s quality of life. Studies have shown that people with both fibromyalgia and obesity showed an improvement in quality of life and pain symptoms once they lost weight.
More research is needed on the effects of diet on fibromyalgia, but making sure the diet is low in sugar and gluten is a good starting point. There is certainly no harm is trying these options to support treatment.
Tender points
When reading up on fibromyalgia, you may have come across the term ‘tender points.’
These are certain areas of the body in which fibromyalgia is said to cause the most pain. These include the back of the head, inner knees, and outer elbows. Pain can also be increased in the neck and shoulders, the outer hips, and the upper chest.
Doctors used to diagnose fibromyalgia based on how they react to pressure at these points. However, this is no longer seen as an accurate way to diagnose the condition, and tender points are no longer used as a reliable indicator of fibromyalgia.
Injections are not advised at these points. However, the pain is now thought to be more widespread and present differently in different people. Instead of specific areas or points of pain, fibromyalgia is identified by the severity and chronic nature of the pain.
Seek medical attention to rule out other causes of pain in these areas.
Outlook
There is no definitive cure for fibromyalgia, but more treatment options and clearer diagnostic criteria are now available.
Symptoms can improve significantly, as long as the patient follows their treatment plan.