Understanding and Recognizing Pre-Migraine Symptoms
Migraine is more than headaches. It’s a neurological condition that impacts more than 36 million Americans, according to the American Migraine Foundation. Migraine can cause severe pain and interrupt your daily activities.
Pre-migraine is one of the four stages of a migraine attack. Pre-migraine symptoms may occur before a migraine attack begins. You may be able to take steps to avoid a painful migraine attack if you can recognize the pre-migraine stage.
What are pre-migraine symptoms?
Migraine has four distinct states. Pre-migraine, called the prodrome stage, consists of a symptom or group of symptoms which let you know that a migraine attack is coming. It can begin anywhere from a few hours to several days before a migraine attack occurs.
The prodrome stage, sometimes also called the pre-headache or premonitory phase, doesn’t occur before every migraine attack, but learning to recognize pre-migraine symptoms can help you take preventative action. It’s also important to know that not everyone who has a prodrome stage will experience the exact same symptoms.
Pre-migraine symptoms may include:
- Mood changes. You might feel depressed, anxious, or irritable without a pinpointable cause.
- Muscle pain. Stiffness and cramping in your neck and shoulders is a common pre migraine symptom.
- Food cravings. You can have strong cravings, especially for sweet foods, before a migraine attack.
- Difficulty concentrating. You might have trouble focusing and feel foggy or confused.
- Fatigue. Even if you had a good night’s sleep, you can feel extra tired leading up to a migraine attack.
- Excessive yawning. Finding yourself yawning frequently throughout the day can be a migraine attack symptom.
- Digestion trouble. You might experience constipation or diarrhea before a migraine attack begins.
- Increased urinary frequency. Needing to visit the bathroom more often than normal is a common prodrome symptom.
- Sensitivity to light and sound. You might have a low tolerance for bright lights and loud sounds before and during a migraine attack.
What to do if you have pre-migraine symptoms
You can start to take action if you recognize pre-migraine symptoms. If you’re being treated by a doctor for migraine, they can help you come up with a pre-migraine management plan that could prevent a full migraine attack from occurring. Try these common steps that can help during the prodrome stage:
- Take pain-relieving medication. It can help to take pain-relieving medication before a migraine attack begins. You can use over-the-counter (OTC) options such as Excedrin, or prescription options. Follow the doctor’s instructions carefully when taking prescription medication for migraine.
- Take any prevention medications. Be careful to not skip a dose of any prevention medications you’ve been prescribed if you’re having prodrome symptoms.
- Avoid any known migraine triggers. It’s always a good idea to avoid anything that triggers your migraine, but taking extra care to avoid triggers when you notice pre migraine symptoms can help prevent a full migraine attack.
- Rest and relax. Taking time to rest and relax can help you prevent a full migraine attack. If you can, try taking a nap or going to bed early. Meditation or other relaxation techniques can be especially useful.
- Find a dark room. It’s best to avoid loud, bright, and stressful situations when pre migraine symptoms occur. Relaxing in a dark and quiet room can help prevent a migraine attack.
- Take a hot shower or bath. A hot shower or bath can help relax your muscles. You can also try warm compresses.
- Try ice packs. Ice packs are a good way to numb your pain and help you rest.
- Drink a caffeinated beverage. Small amounts of caffeine can help relieve pain and can enhance the effects of some OTC pain relief medications. It’s a good idea to stick to a small amount, such as a single cup of coffee or can of soda. Too much caffeine can lead to withdrawal headaches and make it difficult to sleep.
What are the other stages of migraine?
There are three other migraine stages. Not everyone will have every stage during every migraine attack. The migraine stages are:
- Aura stage. For individuals who have an aura with migraine, they usually occur about an hour before a migraine attack. Auras symptoms can vary but often include blurry vision, seeing flashing lights, visual hallucinations, vision loss, numbness, dizziness, and changes in hearing and speech. About one-third of people with migraine experience aura.
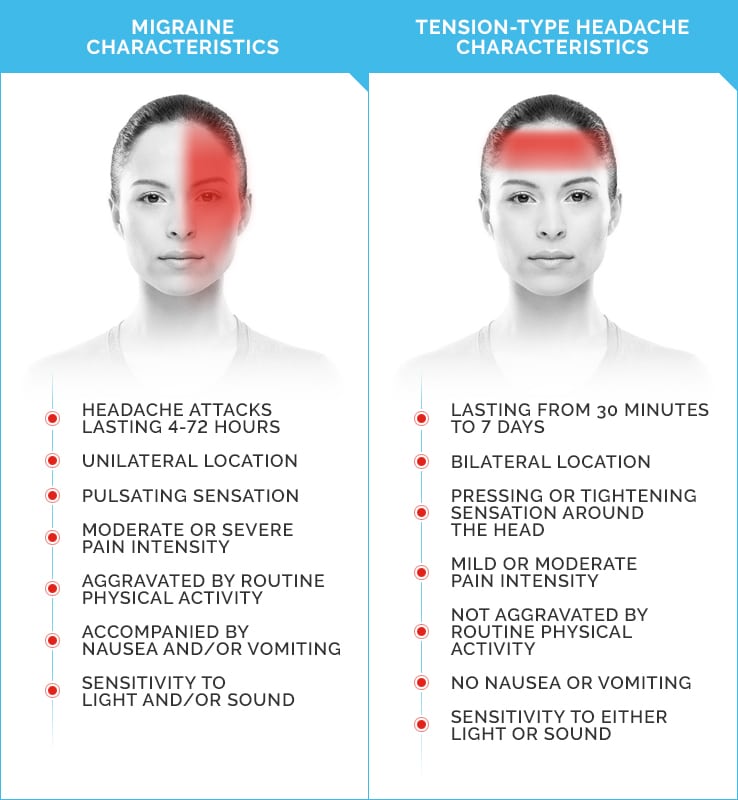
- Headache or attack stage. The headache stage is when moderate-to-severe head pain that’s normally concentrated on one side of your head occurs. Pain is often throbbing and can become more severe when you move. The attack stage can last anywhere from a few hours to 3 days and also includes migraine symptoms such as nausea, vomiting, trouble sleeping, and sensitivity to light, sound, and smells.
- Postdrome or resolution stage. This stage occurs once the migraine attack has faded and can last for a few hours to a few days. Symptoms at this stage often include feeling drained, fatigued, dizzy, and achy. It’s best to continue to avoid triggers and rest as much as you need during this stage.
The takeaway
The pre-migraine stage can start anywhere from a few days to a few hours before you have a migraine attack. Symptoms can vary, but often include:
- confusion
- fatigue
- urinary frequency
- sensitivity to light and sound
- mood changes
- neck pain
- food cravings
Learning to recognize pre-migraine symptoms you experience can help you manage migraine and avoid an attack. Talk with a doctor if you’re having migraine attacks frequently. They can help identify your pre-migraine symptoms and the steps you can take during pre-migraine to avoid an attack.