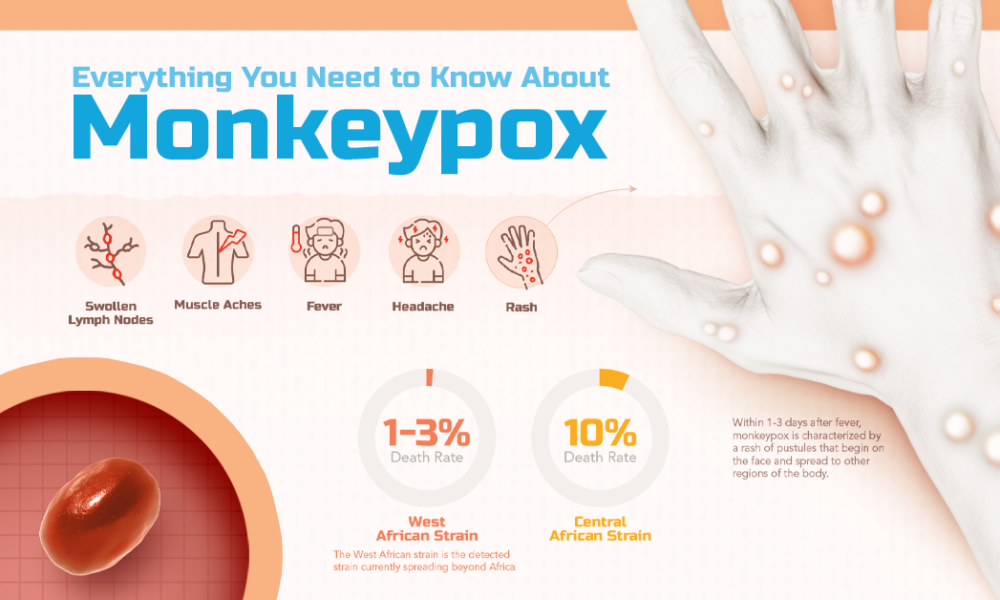
Monkeypox symptoms
People with monkeypox get a rash that may be located on or near the genitals (penis, testicles, labia, and vagina) or anus (butthole) and could be on other areas like the hands, feet, chest, face, or mouth.
- The rash will go through several stages, including scabs, before healing.
- The rash can initially look like pimples or blisters and may be painful or itchy.
Other symptoms of monkeypox can include:
- Fever
- Chills
- Swollen lymph nodes
- Exhaustion
- Muscle aches and backache
- Headache
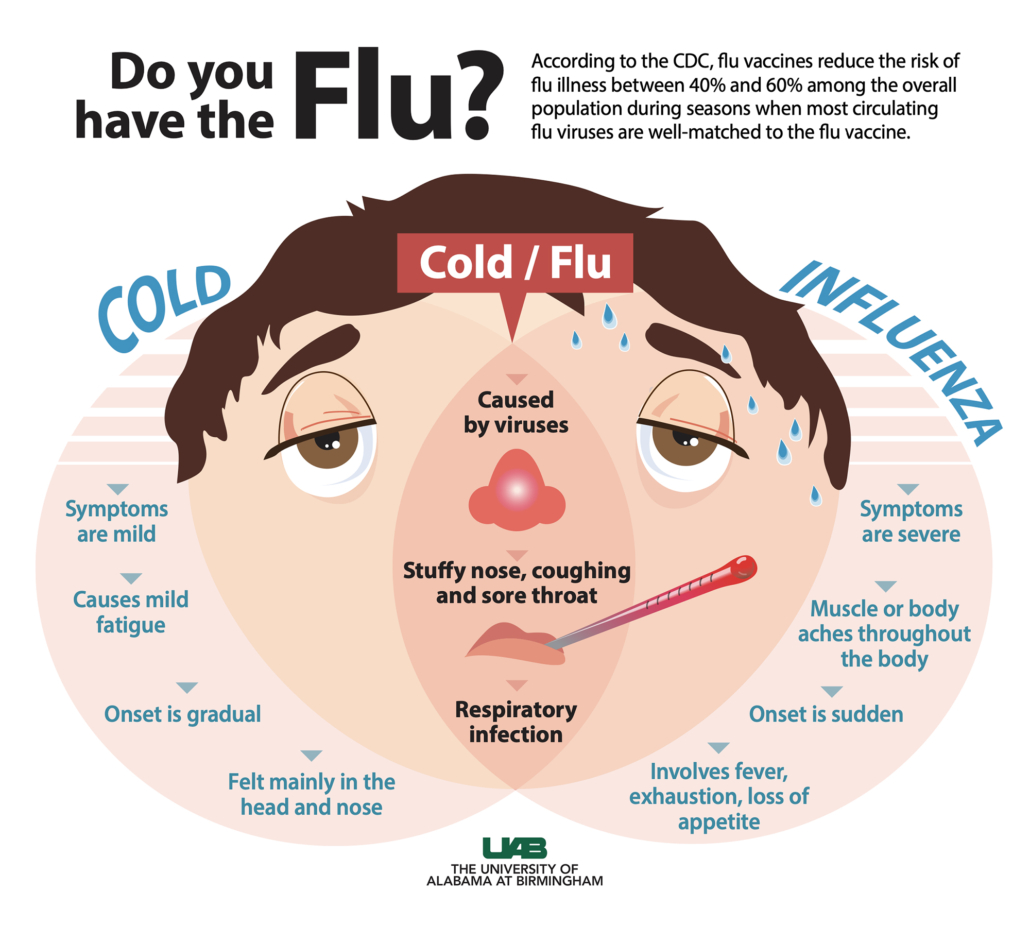
- Respiratory symptoms (e.g. sore throat, nasal congestion, or cough)
You may experience all or only a few symptoms
- Sometimes, people have flu-like symptoms before the rash.
- Some people get a rash first, followed by other symptoms.
- Others only experience a rash.
How long do monkeypox symptoms last?
Monkeypox symptoms usually start within 3 weeks of exposure to the virus. If someone has flu-like symptoms, they will usually develop a rash 1-4 days later.
Monkeypox can be spread from the time symptoms start until the rash has healed, all scabs have fallen off, and a fresh layer of skin has formed. The illness typically lasts 2-4 weeks.
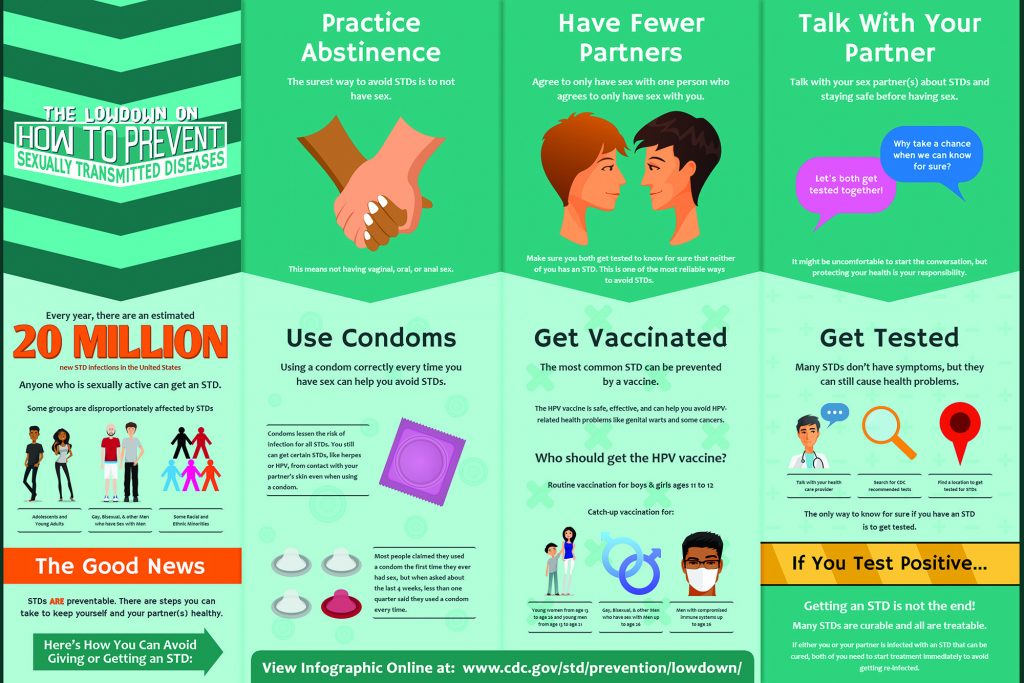
Avoid close contact, including sex or being intimate with anyone, until you have been checked out by a healthcare provider.
If you don’t have a provider or health insurance, visit a public health clinic near you.
When you see a healthcare provider, wear a mask, and remind them that this virus is circulating in the area.
What to Do If You Are Sick
There is no treatment specifically for monkeypox. Because the viruses that cause monkeypox and smallpox are closely related, drugs and vaccines developed to treat and protect against smallpox may be effective for monkeypox.
However, the type of treatment for a person with monkeypox will depend on how sick someone gets or whether they’re likely to get severely ill. Most people with monkeypox recover fully within 2 to 4 weeks without the need for medical treatment.
Some people, like those with a weakened immune system or genital or rectal rashes, may need treatment. Drugs used to treat monkeypox require a prescription and must be requested by a healthcare provider through the local or state health department.
Taking Care of Yourself
- Use gauze or bandages to cover the rash to limit spread to others and to the environment.
- Don’t lance (pop) or scratch lesions from the rash. This does not speed up recovery and can spread the virus to other parts of the body, increase the chance of spreading the virus to others, and possibly cause the open lesions to become infected by bacteria.
- Do not shave the area with the rash until the scabs have fallen off and a new layer of skin has formed. Shaving can spread the virus and cause more lesions.
- Keep skin lesions/rash clean and dry when not showering or bathing.
- Wash hands often with soap and water or use an alcohol-based hand sanitizer, especially after direct contact with the rash.
- If you have rash on your hands, be careful when washing or using sanitizer so as not to irritate the rash.
- If you have rash on your hands, wear gloves that are non-irritating when handling common objects or touching surfaces in shared spaces. If you can, use disposable gloves that can be discarded after each use (e.g., latex, polyurethane, or nitrile gloves). Reusable gloves should be washed with soap and water between use.
- Wear a well-fitting mask around other people until the rash and all other symptoms have resolved.
- Eat healthy and get plenty of rest to allow your body to heal.
Managing Your Symptoms
Medicines like ibuprofen (Advil, Motrin) and acetaminophen (Tylenol) can help you feel better. Your healthcare provider may prescribe stronger pain relievers as well.
For rash in the mouth, rinse with salt water at least four times a day. Prescription mouthwashes, sometimes called miracle or magic mouthwash, or local anesthetics like viscous lidocaine can be used to manage pain. Oral antiseptics like chlorhexidine mouthwash can be used to help keep the mouth clean.
Contact your healthcare provider if pain becomes severe and unmanageable at home.
Rash Relief
The most important thing is to try to not touch or scratch the rash. This can spread the rash to other parts of the body, increase the chance of spreading the virus to others, and possibly cause open lesions to become infected by bacteria. If you do accidentally touch the rash, wash your hands with soap and water and avoid touching sensitive areas like your eyes, nose, mouth, genitals and rectum (butthole).
Topical benzocaine/lidocaine gels can be used for temporary relief. Oral antihistamines such as Benadryl and topical creams such as calamine lotion or petroleum jelly may help with itching.
Soaking in a warm bath (using oatmeal or other over-the-counter bath products for itchy skin) may offer some relief to the dry, itchy sensations that can come with the rash.
People who have the rash in or around their anus (butthole) or genitals (penis, testicles, labia, vagina), or perineum (taint) may also benefit from a sitz-bath. A sitz bath is a round, shallow basin that can be purchased online or at a pharmacy. Most fit over the rim of a toilet but can also be placed in a bathtub. There is also the option to sit in a bathtub with shallow water. Your healthcare provider may prescribe medication like povidone-iodine or other products to be added to the water in a sitz bath. Adding Epsom salt, vinegar, or baking soda to the water can be soothing.