Acute kidney failure
Acute kidney failure occurs when your kidneys suddenly become unable to filter waste products from your blood. When your kidneys lose their filtering ability, dangerous levels of wastes may accumulate, and your blood’s chemical makeup may get out of balance.
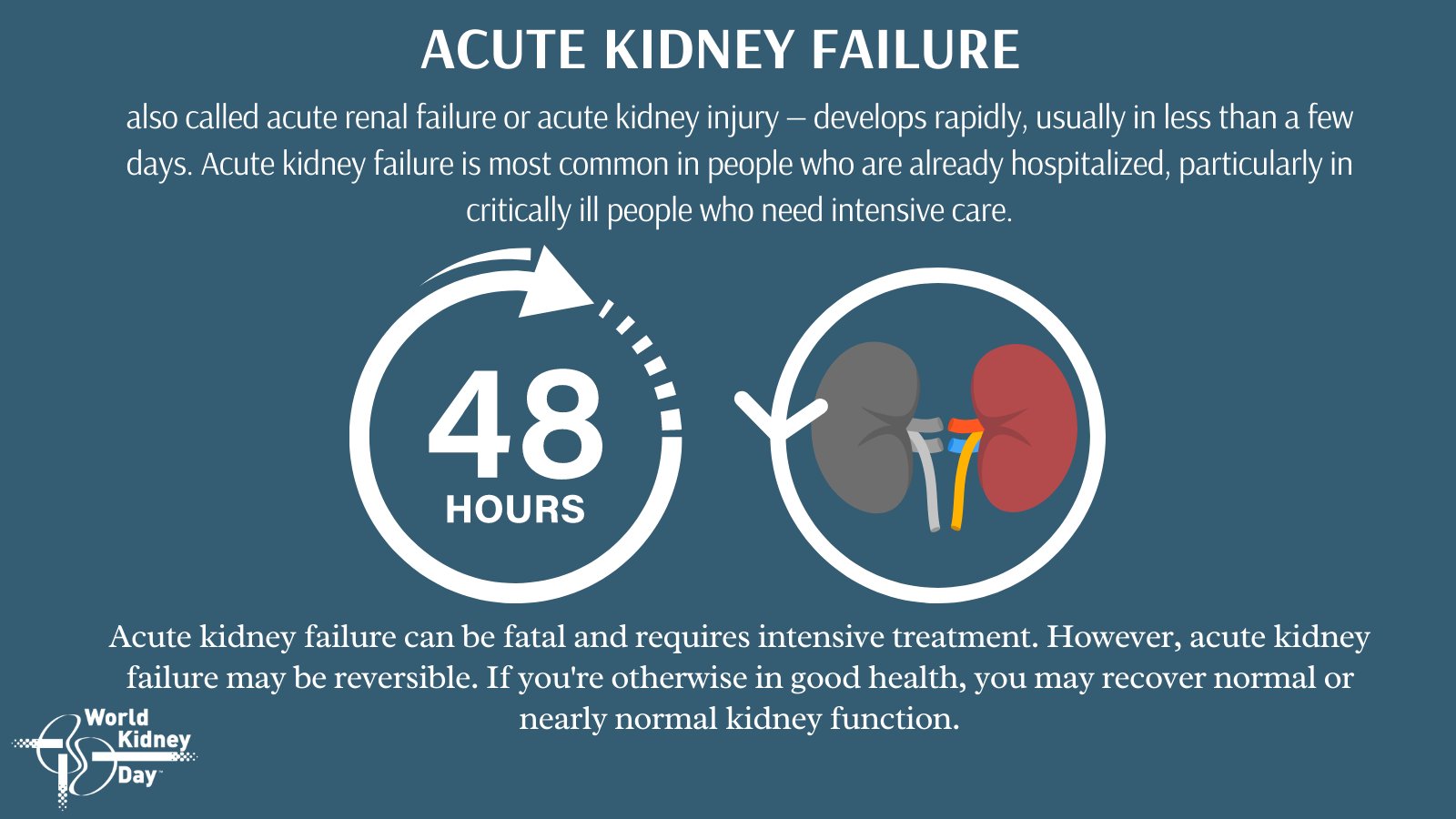
Acute kidney failure — also called acute renal failure or acute kidney injury — develops rapidly, usually in less than a few days. Acute kidney failure is most common in people who are already hospitalized, particularly in critically ill people who need intensive care.
Acute kidney failure can be fatal and requires intensive treatment. However, acute kidney failure may be reversible. If you’re otherwise in good health, you may recover normal or nearly normal kidney function.
Symptoms
Signs and symptoms of acute kidney failure may include:
- Decreased urine output, although occasionally urine output remains normal
- Fluid retention, causing swelling in your legs, ankles or feet
- Shortness of breath
- Fatigue
- Confusion
- Nausea
- Weakness
- Irregular heartbeat
- Chest pain or pressure
- Seizures or coma in severe cases
Sometimes acute kidney failure causes no signs or symptoms and is detected through lab tests done for another reason.
When to see a doctor
See your doctor immediately or seek emergency care if you have signs or symptoms of acute kidney failure.
Causes
Acute kidney failure can occur when:
- You have a condition that slows blood flow to your kidneys
- You experience direct damage to your kidneys
- Your kidneys’ urine drainage tubes (ureters) become blocked and wastes can’t leave your body through your urine
Impaired blood flow to the kidneys
Diseases and conditions that may slow blood flow to the kidneys and lead to kidney injury include:
- Blood or fluid loss
- Blood pressure medications
- Heart attack
- Heart disease
- Infection
- Liver failure
- Use of aspirin, ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve, others) or related drugs
- Severe allergic reaction (anaphylaxis)
- Severe burns
- Severe dehydration
Damage to the kidneys
These diseases, conditions and agents may damage the kidneys and lead to acute kidney failure:
- Blood clots in the veins and arteries in and around the kidneys
- Cholesterol deposits that block blood flow in the kidneys
- Glomerulonephritis (gloe-mer-u-loe-nuh-FRY-tis), inflammation of the tiny filters in the kidneys (glomeruli)
- Hemolytic uremic syndrome, a condition that results from premature destruction of red blood cells
- Infection, such as with the virus that causes coronavirus disease 2019 (COVID-19)
- Lupus, an immune system disorder causing glomerulonephritis
- Medications, such as certain chemotherapy drugs, antibiotics and dyes used during imaging tests
- Scleroderma, a group of rare diseases affecting the skin and connective tissues
- Thrombotic thrombocytopenic purpura, a rare blood disorder
- Toxins, such as alcohol, heavy metals and cocaine
- Muscle tissue breakdown (rhabdomyolysis) that leads to kidney damage caused by toxins from muscle tissue destruction
- Breakdown of tumor cells (tumor lysis syndrome), which leads to the release of toxins that can cause kidney injury
Urine blockage in the kidneys
Diseases and conditions that block the passage of urine out of the body (urinary obstructions) and can lead to acute kidney injury include:
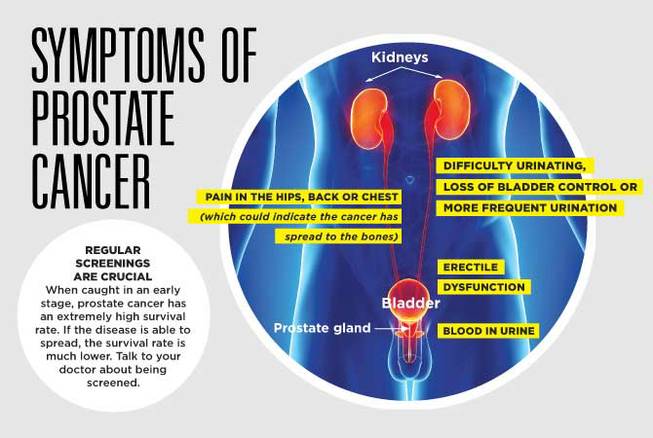
- Bladder cancer
- Blood clots in the urinary tract
- Cervical cancer
- Colon cancer
- Enlarged prostate
- Kidney stones
- Nerve damage involving the nerves that control the bladder
- Prostate cancer
Risk factors
Acute kidney failure almost always occurs in connection with another medical condition or event. Conditions that can increase your risk of acute kidney failure include:
- Being hospitalized, especially for a serious condition that requires intensive care
- Advanced age
- Blockages in the blood vessels in your arms or legs (peripheral artery disease)
- Diabetes
- High blood pressure
- Heart failure
- Kidney diseases
- Liver diseases
- Certain cancers and their treatments
Complications
Potential complications of acute kidney failure include:
- Fluid buildup. Acute kidney failure may lead to a buildup of fluid in your lungs, which can cause shortness of breath.
- Chest pain. If the lining that covers your heart (pericardium) becomes inflamed, you may experience chest pain.
- Muscle weakness. When your body’s fluids and electrolytes — your body’s blood chemistry — are out of balance, muscle weakness can result.
- Permanent kidney damage. Occasionally, acute kidney failure causes permanent loss of kidney function, or end-stage renal disease. People with end-stage renal disease require either permanent dialysis — a mechanical filtration process used to remove toxins and wastes from the body — or a kidney transplant to survive.
- Death. Acute kidney failure can lead to loss of kidney function and, ultimately, death.
Prevention
Acute kidney failure is often difficult to predict or prevent. But you may reduce your risk by taking care of your kidneys. Try to:
- Pay attention to labels when taking over-the-counter (OTC) pain medications. Follow the instructions for OTC pain medications, such as aspirin, acetaminophen (Tylenol, others), ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve, others). Taking too much of these medications may increase your risk of kidney injury. This is especially true if you have pre-existing kidney disease, diabetes or high blood pressure.
- Work with your doctor to manage kidney and other chronic conditions. If you have kidney disease or another condition that increases your risk of acute kidney failure, such as diabetes or high blood pressure, stay on track with treatment goals and follow your doctor’s recommendations to manage your condition.
- Make a healthy lifestyle a priority. Be active; eat a sensible, balanced diet; and drink alcohol only in moderation — if at all.