Cardiovascular Disease Is Primed to Kill More Older Adults, Especially Blacks and Hispanics
Cardiovascular disease — the No. 1 cause of death among people 65 and older — is poised to become more prevalent in the years ahead, disproportionately affecting Black and Hispanic communities and exacting an enormous toll on the health and quality of life of older Americans.
The estimates are sobering: By 2060, the prevalence of ischemic heart disease (a condition caused by blocked arteries and also known as coronary artery disease) is projected to rise 31% compared with 2025; heart failure will increase 33%; heart attacks will grow by 30%; and strokes will increase by 34%, according to a team of researchers from Harvard and other institutions. The greatest increase will come between 2025 and 2030, they predicted.
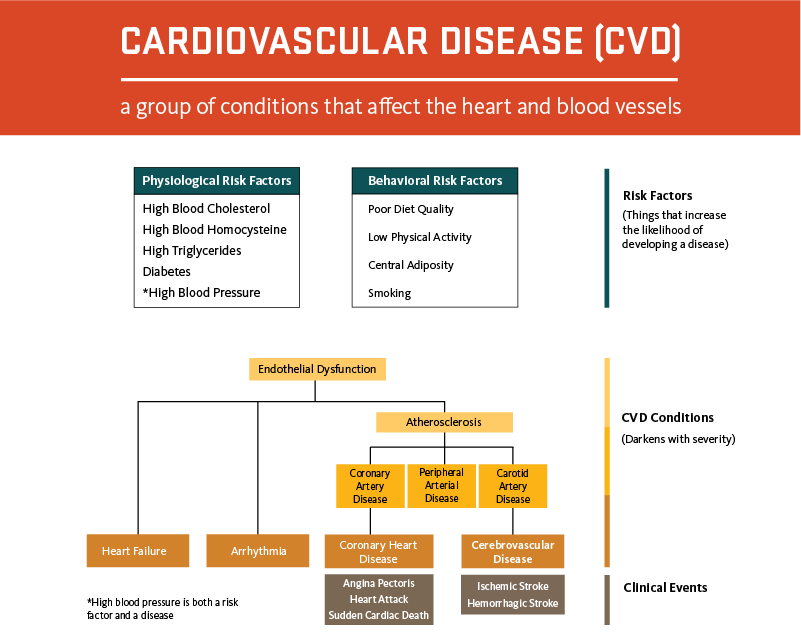
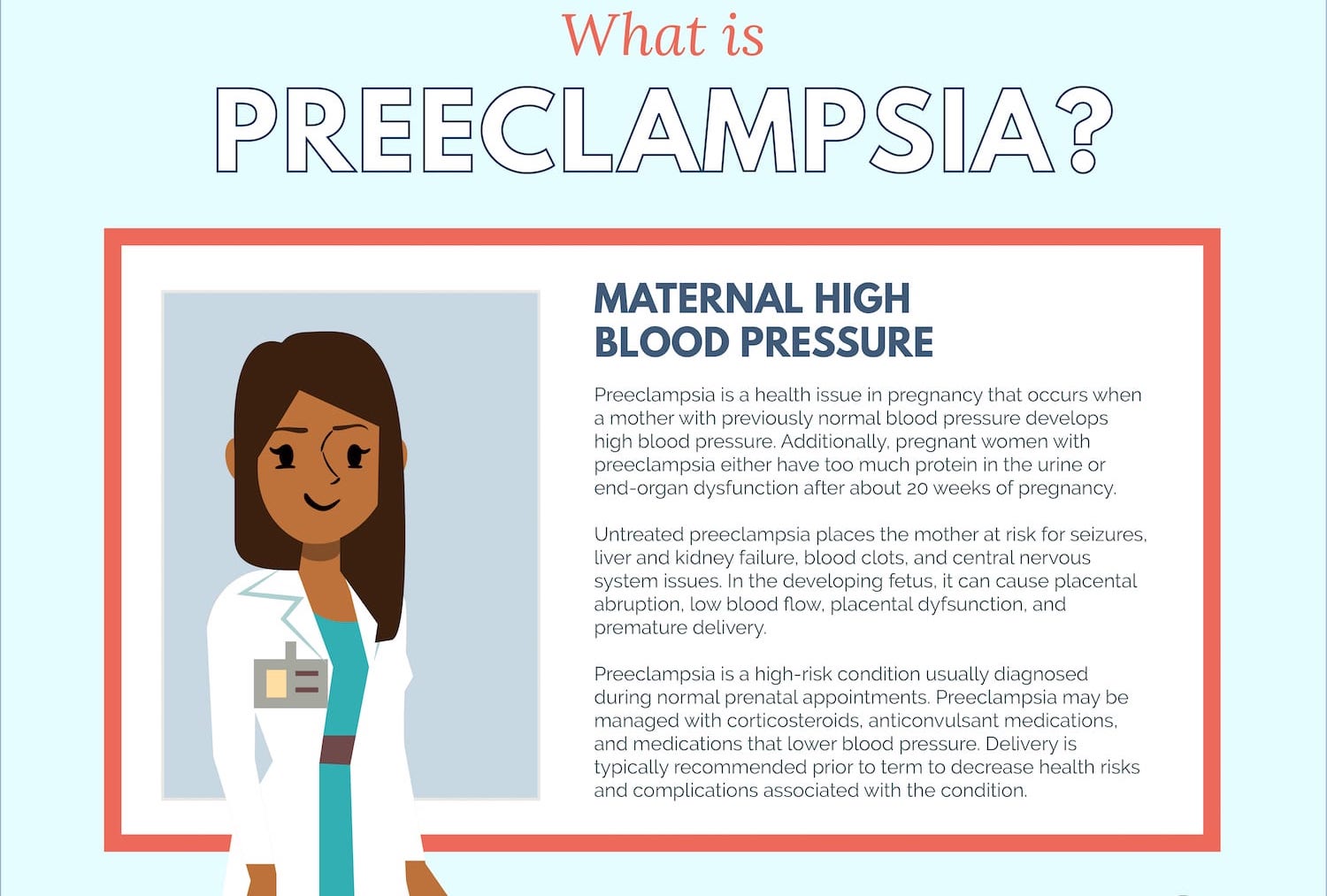
The dramatic expansion of the U.S. aging population (cardiovascular disease is far more common in older adults than in younger people) and rising numbers of people with conditions that put them at risk of heart disease and stroke — high blood pressure, diabetes, and obesity foremost among them — are expected to contribute to this alarming scenario.
Because the risk factors are more common among Black and Hispanic populations, cardiovascular illness and death will become even more common for these groups, the researchers predicted. (Hispanic people can be of any race or combination of races.)
“Disparities in the burden of cardiovascular disease are only going to be exacerbated” unless targeted efforts are made to strengthen health education, expand prevention, and improve access to effective therapies, wrote the authors of an accompanying editorial, from Stony Brook University in New York and Baylor University Medical Center in Texas.
“Whatever focus we’ve had before on managing [cardiovascular] disease risk in Black and Hispanic Americans, we need to redouble our efforts,” said Clyde Yancy, chief of cardiology and vice dean for diversity and inclusion at Northwestern University’s Feinberg School of Medicine in Chicago, who was not involved with the research.
Of course, medical advances, public health policies, and other developments could alter the outlook for cardiovascular disease over the next several decades.
More than 80% of cardiovascular deaths occur among adults 65 or older. For about a dozen years, the total number of cardiovascular deaths in this age group has steadily ticked upward, as the ranks of older adults have expanded and previous progress in curbing fatalities from heart disease and strokes has been undermined by Americans’ expanding waistlines, poor diets, and physical inactivity.
Among people 65 and older, cardiovascular deaths plunged 22% between 1999 and 2010, according to data from the National Heart, Lung, and Blood Institute — a testament to new medical and surgical therapies and treatments and a sharp decline in smoking, among other public health initiatives. Then between 2011 and 2019, deaths climbed 13%.
The covid-19 pandemic has also added to the death toll, with coronavirus infections causing serious complications such as blood clots and millions of seniors avoiding seeking medical care out of fear of becoming infected. Most affected have been low-income individuals, and older non-Hispanic Black and Hispanic people, who have died from the virus at disproportionately higher rates than non-Hispanic white people.
“The pandemic laid bare ongoing health inequities,” and that has fueled a new wave of research into disparities across various medical conditions and their causes, said Nakela Cook, a cardiologist and executive director of the Patient-Centered Outcomes Research Institute, an independent organization authorized by Congress.
One of the most detailed examinations yet, published in JAMA Cardiology in March, examined mortality rates in Hispanic, non-Hispanic Black, and non-Hispanic white populations from 1990 to 2019 in all 50 states and the District of Columbia. It showed that Black men remain at the highest risk of dying from cardiovascular disease, especially in Southern states along the Mississippi River and in the northern Midwest. (The age-adjusted mortality rate from cardiovascular disease for Black men in 2019 was 245 per 100,000, compared with 191 per 100,000 for white men and 135 per 100,000 for Hispanic men. Results for women within each demographic were lower.)
Progress stemming deaths from cardiovascular disease in Black men slowed considerably between 2010 and 2019. Across the country, cardiovascular deaths for that group dropped 13%, far less than the 28% decline from 2000 to 2010 and 19% decline from 1990 to 2000. In the regions where Black men were most at risk, the picture was even worse: In Mississippi, for instance, deaths of Black men fell only 1% from 2010 to 2019, while in Michigan they dropped 4%. In the District of Columbia, they actually rose, by nearly 5%.
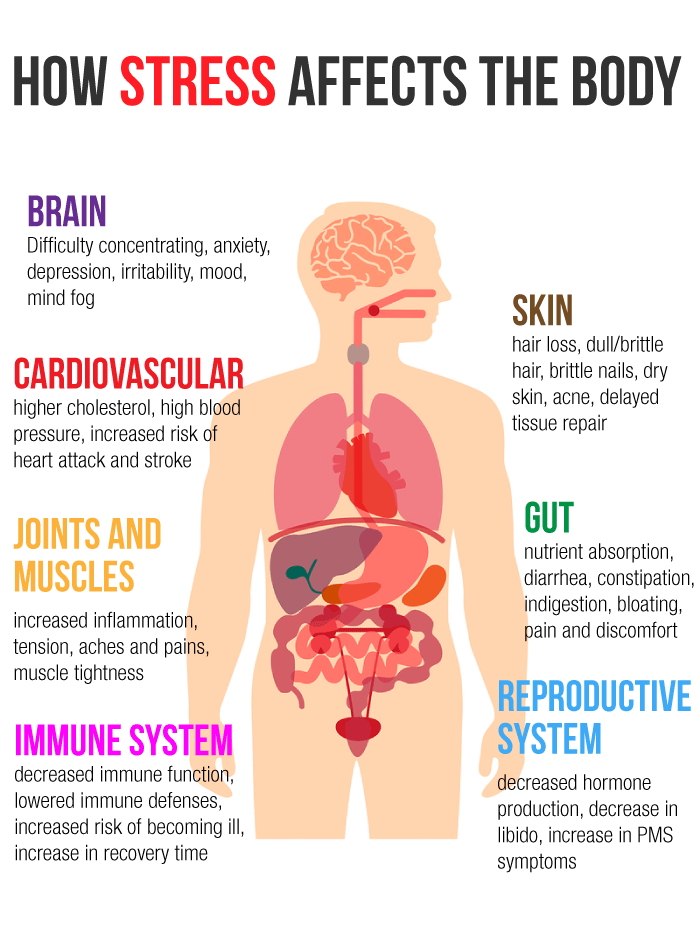
While individual lifestyles are partly responsible for the unequal burden of cardiovascular disease, the American Heart Association’s 2017 scientific statement on the cardiovascular health of African Americans notes that “perceived racial discrimination” and related stress are associated with hypertension, obesity, persistent inflammation, and other clinical processes that raise the risk of cardiovascular disease.
Though Black people are deeply affected, so are other racial and ethnic minorities who experience adversity in their day-to-day lives, several experts noted. However, recent studies of cardiovascular deaths don’t feature some of these groups, including Asian Americans and Native Americans.
What are the implications for the future? Noting significant variations in cardiovascular health outcomes by geographic location, Alain Bertoni, an internist and professor of epidemiology and prevention at Wake Forest University School of Medicine, said, “We may need different solutions in different parts of the country.”
Gregory Roth, a co-author of the JAMA Cardiology paper and an associate professor of cardiology at the University of Washington School of Medicine, called for a renewed effort to educate people in at-risk communities about “modifiable risk factors” — high blood pressure, high cholesterol, obesity, diabetes, smoking, inadequate physical activity, unhealthy diet, and insufficient sleep. The American Heart Association has suggestions on its website for promoting cardiovascular health in each of these areas.
Michelle Albert, a cardiologist and the current president of the American Heart Association, said more attention needs to be paid in medical education to “social determinants of health” — including income, education, housing, neighborhood environments, and community characteristics — so the health care workforce is better prepared to address unmet health needs in vulnerable populations.
Natalie Bello, a cardiologist and the director of hypertension research at the Smidt Heart Institute at Cedars-Sinai Medical Center in Los Angeles, said, “We really need to be going into vulnerable communities and reaching people where they’re at to increase their knowledge of risk factors and how to reduce them.” This could mean deploying community health workers more broadly or expanding innovative programs like ones that bring pharmacists into Black-owned barbershops to educate Black men about high blood pressure, she suggested.
“Now, more than ever, we have the medical therapies and technologies in place to treat cardiovascular conditions,” said Rishi Wadhera, a cardiologist and section head of health policy and equity research at the Smith Center for Outcomes Research in Cardiology at Beth Israel Deaconess Medical Center in Boston. What’s needed, he said, are more vigorous efforts to ensure all older patients, including those from disadvantaged communities, are connected with primary care physicians and receive appropriate screening and treatment for cardiovascular risk factors, and high-quality, evidence-based care in the event of heart failure, a heart attack, or a stroke.