5 common myths about obesity
Although obesity is common, there are many misconceptions associated with it — and these myths often fuel social stigma. In this edition of Medical Myths, we tackle five of the most common misunderstandings about obesity.
According to the Centers for Disease Control and Prevention (CDC), in the United States, 42.4% of adults have obesity. Globally, the World Health Organization (WHO) estimate that around 650 million adults have obesity.
People are growing increasingly aware of the health issues associated with obesity. However, despite public health campaigns, myths continue unabated. Many of the most common myths drive stigma that can impact the mental health of people with obesity.
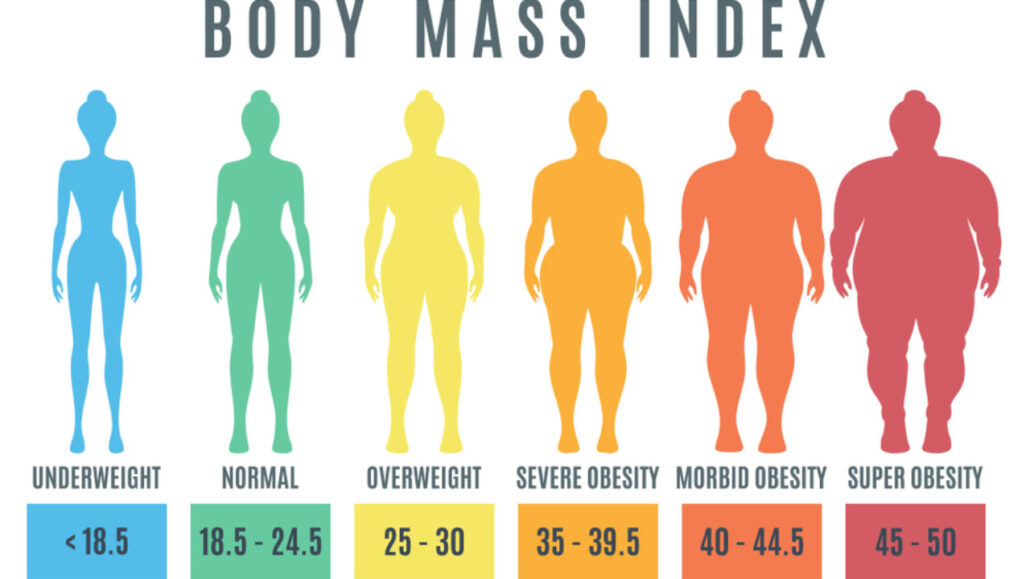
For instance, the results of one 2020 meta-analysis on the subject indicate “a stronger association between weight stigma and diminished mental health with increasing body mass index [BMI].”
Addressing the myths that surround obesity is important. With this in mind, this article will tackle five of the most prevalent misunderstandings around this condition.
1. To reduce obesity, just eat less and move more
In many cases, consuming more calories than the body needs for a prolonged amount of time is the direct cause of obesity. Indeed, the vast majority of measures for reducing obesity aim to lower caloric intake, increase physical activity, or both.
Although diet and exercise are important factors, several unrelated factors can also play a significant part in obesity.
These factors, which people often forget about, include insufficient sleep, psychological stress, chronic pain, endocrine (hormone) disruptors, and the use of certain medications.
In these cases, overeating, for instance, may be a symptom rather than a cause.
Also, some of these factors work together to increase the chance of obesity. As an example, stress can increase the chance of obesity. Due to the prevalence of weight stigma, obesity can be stressful for some people, thereby increasing stress levels and sparking a negative feedback loop.
Added to this, stress can impact sleep quality, and this, in turn, might cause sleep deprivation, which is another factor in the development of obesity. Sleep deprivation also appears to increase stress levels. As one paper explains, “stress hormone levels correlate positively with decreased sleep duration.”
Sleep apnea, wherein a person stops breathing for short periods during sleep, is more prevalent in people with overweight or obesity. Again, a cycle can form: As they gain weight, their sleep apnea may worsen, which can lead to sleep deprivation, which can lead to further weight gain.
As another example, there appears to be an association between chronic pain and obesity. The reasons for this relationship are sure to be complex and differ from person to person, but they likely include chemical factors, sleep, depression, and lifestyle.
It is not difficult to see how chronic pain would both increase stress levels and impact sleep, adding to the negative loops outlined above.
Stress, sleep, and pain are just three interlinking factors that can drive obesity. Each person’s case will be different, but simply receiving an instruction to “move more and eat less” might not be an adequate intervention.
As this article will continue to reiterate, calorie intake and exercise are vital factors in reducing obesity, but they do not tell the whole tale.
2. Obesity causes diabetes
Obesity does not directly cause diabetes. It is a risk factor for type 2 diabetes, but not everyone with obesity will develop type 2 diabetes, and not everyone with type 2 diabetes has obesity.
Obesity is also a risk factor for gestational diabetes, which occurs during pregnancy, but it is not a risk factor for type 1 diabetes.
3. People with obesity are lazy
An inactive lifestyle is a factor in obesity, and becoming more active can aid weight loss, but there is more to obesity than inactivity.
One 2011 study used accelerometers to measure the activity levels of 2,832 adults, aged 20–79 years, for 4 days. Their step counts reduced as their weight increased, but the differences were not as significant as one might predict, particularly for women.
The list below shows the women’s weights and how many steps they took per day during this study:
- those with a “healthy” weight: 8,819 steps
- those with overweight: 8,506 steps
- those with obesity: 7,546 steps
When one considers that someone with overweight or obesity expends more energy with each step, the difference between the groups’ overall energy expenditures may be even more slight.
This does not mean that physical activity is not essential for good health, but the story is more complex.
Another factor to consider is that not all people are able to perform physical activity. For instance, some physical disabilities can make moving challenging or impossible.
Also, certain mental health issues can severely impact motivation — and there appears to be a relationship between depression and obesity, which further deepens the complexity.
Aside from physical and mental health issues, some people with obesity may also have a negative body image, which might make leaving their home a more daunting prospect.
4. If your close relatives have obesity, so will you
The relationship between obesity and genetics is complex, but someone whose relatives have obesity will not necessarily develop the condition themselves. However, their chance of doing so is higher.
Understanding the role of genes and the environment in isolation is difficult; people who share similar genes often live together and, therefore, may have similar dietary and lifestyle habits.
In 1990, a group of researchers published a study that helped split genes from the environment. The results appeared in The New England Journal of Medicine.
The scientists investigated twins who had been brought up apart and compared them with twins who had been brought up together. In this way, they hoped to tease apart the impact of genetics and the environment. Overall, they conclude:
“Genetic influences on [BMI] are substantial, whereas the childhood environment has little or no influence.”
One twin study from 1986 reached similar conclusions. The researchers found that the weights of adopted children correlated with the weights of their biological parents, but not with those of their adoptive parents.
Although more recent studies have identified a more significant role for the environment, genetics do appear to play an important part in obesity.
In recent years, scientists have searched for the genes that influence the chance of obesity. As the CDC explain, in most people with obesity, “no single genetic cause can be identified. Since 2006, genome-wide association studies have found more than 50 genes associated with obesity, most with very small effects.”
One gene that is linked to obesity is a variant of a gene called FTO. This variant, according to one 2011 study, is associated with a 20–30% increased chance of obesity.
Although genetics are important, this does not mean that obesity is inevitable for someone whose relatives have the condition. The above study, which involved individuals with the FTO gene variant, looked at the role of exercise. As the paper explains:
“Using data from over 218,000 adults, the authors found that carrying a copy of the susceptibility gene increased the odds of obesity by 1.23-fold. But the size of this influence was 27% less in the genetically susceptible adults who were physically active.”
A review and meta-analysis that investigated the same gene variant came to a similar conclusion. The authors explain that people with the FTO variant “respond equally well to […] weight loss interventions and thus genetic predisposition to obesity associated with the FTO minor allele can be at least partly counteracted through such interventions.”
However, it is important to reiterate the point that these interventions alone may not be helpful for some people.
5. Obesity does not impact health
This is a myth. There are several conditions associated with obesity. For instance, obesity increases the risk of diabetes, high blood pressure, cardiovascular disease, osteoarthritis, sleep apnea, and some mental health conditions.
That said, even modest weight loss can provide health benefits. According to the CDC, “weight loss of 5–10% of your total body weight is likely to produce health benefits, such as improvements in blood pressure, blood cholesterol, and blood sugars.”
Also, a review of existing literature in the BMJ concludes that weight loss interventions “may reduce premature all-cause mortality in adults with obesity.”
Obesity is highly prevalent. Currently, the stigma surrounding the condition is unhelpful and can be damaging. We need to address it whenever we encounter it.