10 home remedies for wheezing
Wheezing is a common symptom of various respiratory disorders that cause tightening in the throat. There are several ways a person can stop their wheezing at home without using an inhaler, but these will depend on the cause.
Wheezing happens when the airways are tightened, blocked, or inflamed, making a person’s breathing sound like whistling or squeaking. Common causes include a cold, asthma, allergies, or more serious conditions, such as chronic obstructive pulmonary disease.
Steam inhalation is an effective home remedy for wheezing.
The following home treatments for wheezing aim to open up the airways, reduce the irritants or pollution that a person breathes in, or treat the underlying causes of the wheezing.
If a person has asthma or another medical condition that causes wheezing, they should speak to our doctors in clinic and use the medications prescribed for it, such as an asthma inhaler.
Effective home remedies for wheezing include:
1. Steam inhalation
Inhaling warm, moisture-rich air can be very effective for clearing the sinuses and opening up the airways.Peppermint essential oil may have pain-relieving and anti-inflammatory effects. Research suggests that it may relax the muscles of the respiratory system, which could help to relieve wheezing and other respiratory problems.
If a steam bath does not appeal to you, a sauna room or hot shower can also help loosen congestion. Gently tapping on the back or chest and breathing deeply can help the steam work even better.
2. Hot drinks
Warm and hot drinks can help to loosen up the airways and relieve congestion.
Honey is a natural anti-inflammatory and antimicrobial, so adding a teaspoon of honey to a hot drink may further improve a person’s symptoms.
A 2017 study found that eating one tablespoon of honey twice a day, along with other treatments, helped to relieve throat congestion.
Some people find that peppermint or other menthol teas work well. A person can try experimenting with different teas to find one that helps.
3. Breathing exercises
Breathing exercises may help with COPD, bronchitis, allergies, and other common causes of wheezing.
A 2009 study found that certain yoga-inspired breathing techniques could help with breathing difficulties related to bronchial asthma, including wheezing.
Breathing exercises often include deep, regular inhalations and exhalations. A doctor or respiratory therapist can help with deciding the most effective breathing techniques.
A person may find that they have trouble breathing during a panic attack. Deep breathing exercises can also assist here. It may help to try slow breathing, focusing on breathing deeply into the stomach, and counting breathes.
4. Humidifiers
A humidifier may help to reduce wheezing.
During the dry winter months, wheezing often gets worse. A humidifier in the bedroom can help loosen congestion and reduce the severity of wheezing.
A person can add peppermint or other oils to the water in the humidifier, though they should check the humidifier’s instructions before adding anything other than water.
5. Air filters
Many conditions that cause wheezing can get worse when the air is polluted or in response to allergens. A home air filter can reduce the presence of irritants that may trigger wheezing and breathing trouble.
6. Identifying and removing triggers
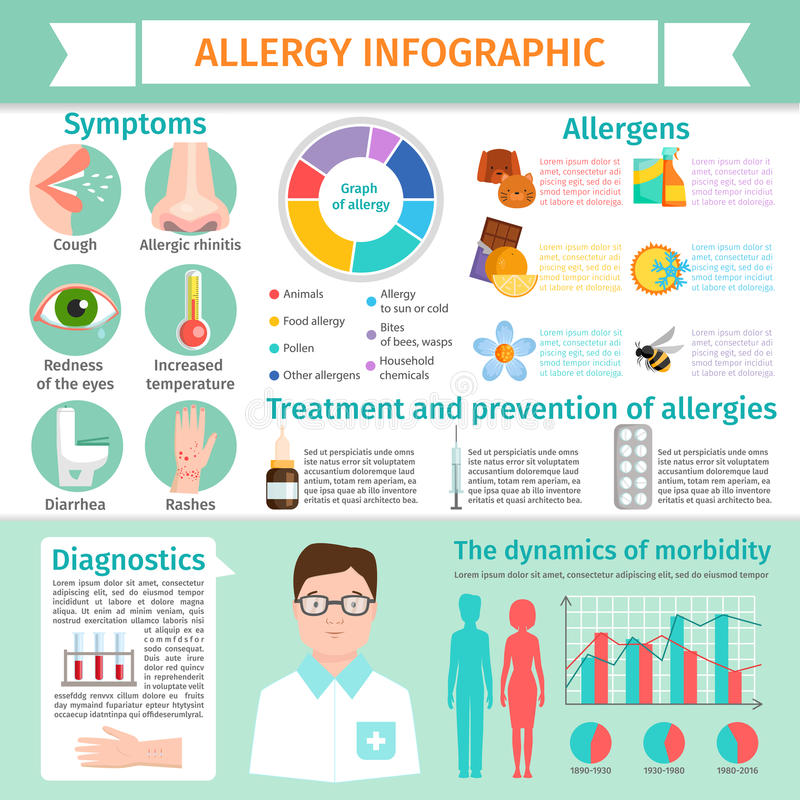
Chronic illnesses such as asthma and allergies may get worse in response to certain triggers, such as stress or allergens. Controlling these triggers, as much as possible, can help.
For instance, a person with a chronic respiratory condition who also has allergies might take allergy medication and avoid allergy triggers.
7. Allergy medications
People with allergies can benefit from a wide variety of allergy medications, including decongestants, corticosteroid tablets, and antihistamines.
Nasal sprays may be especially helpful to relieve a tight chest, congestion, and inflammation that can cause wheezing.
More severe allergies may require prescription allergy medication.
8. Allergy immunotherapy
Immunotherapy is a process of retraining the immune system not to react to allergens.
The most common form of immunotherapy is allergy shots. A person may need several treatments, but over time, immunotherapy can reduce the frequency of wheezing.
Immunotherapy may also be helpful for people with other chronic conditions, such as COPD, who also have allergies.
9. Bronchodilators
Bronchodilators are medications that help relax the lungs and prevent the airways from narrowing. They can help with wheezing caused by COPD and asthma.
Bronchodilators come in two forms:
- Short-acting bronchodilators. Sometimes known as rescue inhalers, these can stop an asthma or COPD attack.
- Long-acting bronchodilators. This variety helps relax the airways over the long-term, reducing the frequency and severity of wheezing episodes.
Bronchodilators should be obtained from a doctor and can then be used at home, as needed.
10. Other medications
A wide variety of medications can treat wheezing that is due to underlying illness. A person who experiences wheezing due to a severe allergic reaction, for instance, may require epinephrine or corticosteroids.
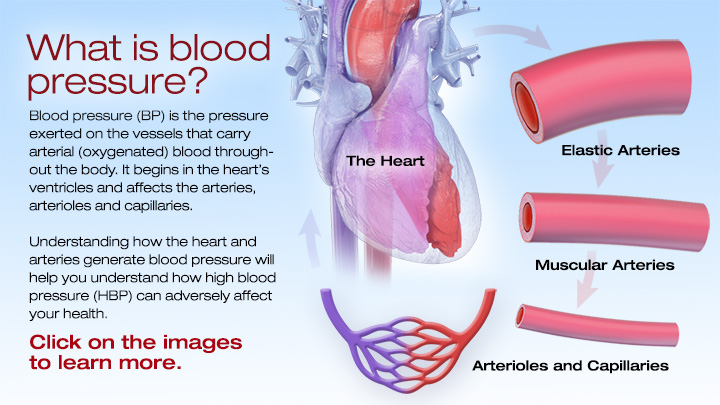
People with heart health issues may take blood pressure medication or blood thinners to prevent further damage to the heart.
It is vital to discuss with a doctor whether medication might help, and how various medications may interact with one another.
Outlook
The long-term outlook for wheezing ultimately depends on its cause. Even when wheezing is due to a chronic illness, it can often be well-managed with medication and home treatments.
Ongoing medical care remains important, however, and people whose symptoms do not improve should consult a doctor. Consider tracking symptoms to identify any underlying triggers for symptoms.
If wheezing is causing concern, it is essential to remain calm, as panicking can worsen wheezing. Keep the breathing slow and regular and seek medical treatment when appropriate.
Even when wheezing is due to a serious medical condition, medications can improve symptoms.